Shoulder:Trauma
Contents
- 1 Proximal Humeral Fracture
- 1.1 Bullet Points
- 1.2 Keywords
- 1.3 Prevalence
- 1.4 Anatomy
- 1.5 Types of Fracture and Classification
- 1.6 Conservative Treatment (Nonoperative Treatment)
- 1.7 Adjuvant procedures
- 1.8 Osteosynthesis
- 1.9 Hemiarthroplasty
- 1.10 Reverse Shoulder Arthroplasty
- 1.11 Rehabilitation
- 1.12 Decision Making
- 1.13 References
- 2 Proximal Humeral Fracture Sequelae
- 3 What would Codman have thought about this?
Proximal Humeral Fracture
Bullet Points
- Assessment of an acute proximal humerus fracture includes a complete trauma series radiography and, where surgical treatment is considered, a CT scan with three-dimensional reconstruction.
- The decisive elements of choice between osteosynthesis and implant are essentially the patient’s age, the risk of humeral head necrosis and bone strength.
- The surgical treatment is difficult and should, in cases of osteosynthesis, lead to an anatomical result.
- According to the literature there is no difference between antegrade intramedullary nailing and plate osteosynthesis.
- The reverse implant is increasingly the treatment of choice for the elderly.
- Where stability permits, early, passive mobility rehabilitation should be commenced. If this is not the case, then rehabilitation should be deferred and the patient immobilized in the meantime.
Keywords
Shoulder; Proximal humerus fracture; Arthroscopy; Osteosynthesis; Hemi arthroplasty; Intramedullary nailing; Plate; Reverse implant.
Prevalence
Proximal humeral fractures are limited to those located above the insertion point of the superior edge of the pectoralis major. They represent 5% of all fractures in patients over 40 years of age.[1]
Their incidence having drastically increased between 1970 (87/100'000 individuals) and 1995 (304/100'000 individuals) seems, for no clear reason, to have reached a plateau since 2010 (297/100'000 individuals in 2015).[2][3]
Anatomy
Morphology
Anatomical restitution, and especially the position of the tuberosities after fixation and during all reconstruction work, is essential. The height of the greater tuberosity in relation to the head is crucial. Normally, the tuberosity lies 8±1.2 mm (range, 6 to 10 mm) below the superior most portion of the humeral head.[4]
In non-pathologic conditions, the greater tuberosity is never above the top of the humeral head. As little as 5 mm of displacement not only creates impingement, but also insufficiency in the posterosuperior rotator cuff due to lack of tension relative to the Blix curve (Figure 1). Malunion can result in a mechanical block to shoulder abduction or external rotation and altered rotator cuff mechanics causing weakness. Consequently, surgical fixation is recommended for fractures with residual displacement greater than 5 mm, or 3 mm in active patients involved in frequent overhead activity. Similarly, a greater tuberosity that is too low will also harm the rotator cuff.[5][6]
The superior edge of the pectoralis major and the top of the humeral head is a reliable measure that can be used intraoperatively to decide the height of the humerus prosthesis or humeral head in comminuted fractures of the proximal humerus. Pectoralis major tendons inserted 54 to 56 mm distal to the superior aspect of the humeral head and 47 mm distal to superomedial tip of greater tuberosity.[7][8] The distance between the superior edge of the pectoralis major and the top of the humeral head might be shorter (49 mm) in Asiatic women.[9] In a study using the pectoralis major tendon as a reference intraoperatively reconstruction of the height of the humerus prosthesis measured by evaluating the radiological humeral length in comparison to the contralateral side within 7 mm±7 mm could be shown.[10]
The pectoralis major insertion is also very reproducible regarding its relationship to retroversion. The mean distance to the posterior fin of the prosthesis was 10 mm and the mean angle 25 degrees.[11]
The pectorals major insertion has a reproducible relation to the bicipital groove, making it a good landmark for tuberosities positioning in case of fracture reconstruction.[12]
The lateral offset of the greater tuberosity relative to the diaphyseal axis is another important anatomic variable, but sometimes difficult to restore due to the comminuted, and often porotic nature of fractured tuberosities, giving them an eggshell appearance. The offset is on average 18±2 mm (range between 1 to 22 mm) (Figure 2).[4]
Every effort should be made to restore this relationship intraoperatively whether by anatomic reconstruction with osteosynthesis (Figure 3) or during arthroplasty surgery. In the setting of chronic non-union, allograft reconstruction has also been described.[13][14][15]
Lastly, the head-shaft relationship must be restored. The neck-shaft angle, posterior tilt and retroversion are key factors.[16]
If the above-mentioned key points are not taken into account, or left uncorrected, the sequelae could include malunions that are particularly difficult to treat.
Vascular
The perfusion of the proximal humerus arises from the anterior and posterior humeral circumflex arteries, themselves terminal branches of the axillary artery (Figure 4). Due to the location of these vessels in close proximity to the fracture, they can be subject to lesions (Figure?). The anterior humeral circumflex artery courses along the inferior border of the subscapularis. The artery gives off an anterolateral ascending branch that courses along the lateral aspect of the bicipital groove before entering the humeral head and becoming the arcuate artery. The anterior humeral circumflex vessel continues postero-laterally to anastomose with the posterior humeral circumflex vessel. The posterior humeral circumflex artery travels with the axillary nerve through the quadrilateral space before it goes on to its anastomosis with the anterior humeral circumflex. It has been believed that the anterolateral branch of the anterior humeral circumflex artery is the main source of perfusion of the humeral head with the posterior vessels only perfusing a small portion of the head. It seems that 64 % of the humeral head blood supply is derived from the posterior humeral circumflex artery and the anterior vessel only accounted for 36 % of the perfusion,[17] This finding and the numerous extraosseous anastomoses that can compensate explain the rather low rate of avascular necrosis. Thus, the humeral head has the possibility to revascularize after injury. Isolated surgical neck and isolated greater tuberosity fractures have a very low incidence of osteonecrosis as the blood supply to the humeral head is relatively preserved. Four-part fractures have a higher incidence of osteonecrosis than three-part fractures. Four-part fractures with associated dislocation have the highest risk for osteonecrosis.The presence of humeral head ischemia in the acute injury setting does not predict subsequent avascular necrosis. The predictive characteristics of humeral head ischemia, from most predictive to least predictive, are: calcar length less than 8 mm, disrupted medial hinge, humeral head angulation more than 45 degrees, and head-split fracture. Hertel et al. evaluated predictors of humeral head ischemia at the time of surgery in a prospective study of 100 intracapsular proximal humerus fractures. They found the most accurate predictive measures of humeral head ischemia, from most accurate to least accurate, were: a calcar length <8 mm, disruption of the medial hinge, basic fracture pattern, displacement of the humeral head >45 degrees, displacement of the tuberosities >10 mm, glenohumeral dislocation and head-split fractures (equally predictive).[18]
Nerve
The axillary nerve comes off the of the brachial plexus (middle trunk, posterior division, posterior cord) carrying fibers from C5 and C6. The axillary nerve travels through the quadrangular space with the posterior circumflex humeral artery and vein to innervate the teres minor and deltoid muscles and supply sensation over the lateral shoulder. The axillary nerve is located approximately 7 cm from the tip of the acromion.[19]
Types of Fracture and Classification
Codman's Classification
Neer’s Classification
The classification does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
Proximal humerus fractures are classified based on the relationship of 4 fracture fragments: greater tuberosity, lesser tuberosity, articular surface, shaft. Parts are considered separate parts, if displacement is > 1 cm or angulation is >45°.
Duparc’s Classification
This classification is mainly used in France. Duparc et al. distinguished extra-articular fractures from articular fractures (Figures 6-12).[20]
Essential points
The anatomic requirements to be respected during any intervention for proximal humerus fractures are:
- The height of the greater tuberosity relative to the proximal humeral head;
- The lateral offset of the greater tuberosity relative to the diaphyseal axis;
- The neck-shaft angle, posterior tilt and humeral retroversion.
Conservative Treatment (Nonoperative Treatment)
Non- or minimally displaced proximal humerus fractures are most commonly managed nonoperatively with the majority of patients returning to their baseline functional status by 1 year. Effectively, the shoulder tolerates a substantial degree of malunion and many of these fractures are minimally displaced. Koval et al. studied 104 patients with one-part proximal humerus fractures treated non-operatively, and found 80% with good or excellent results[21]. They also found that 90% of patients treated non-operatively had either no or mild pain in the shoulder at follow-up. Overall fracture displacement (i.e. impacted varus fractures) has a minor impact on fracture healing and functional outcome.[22] Court-Brown et al. showed that the patient age was the major factor in the overall outcome: younger patients had the best results.[23]
Tejwani et al. performed a prospective study of 67 patients with 1-part proximal humerus fractures.[24] At 1-year follow up the American Shoulder and Elbow Surgeons Shoulder (ASES) score and functional status was similar to pre-injury status. However, range of motion of the affected shoulder was diminished in both external and internal rotation. Anterior forward flexion was preserved.
Hanson et al.[22] prospectively analyzed 160 patients with proximal humerus fractures of all Neer types (1-4 parts and head-splitting) managed nonoperatively. At 1-year follow up, 93% patients showed solid union. Delayed union and nonunion was 7% with patients that smoke. This was 5.5 times greater than non-smokers. Constant and DASH scores improved steadily over time but were still lower compared to the contralateral extremity. Of employed patients, 97.6% returned to work with a median time off of 10 weeks and no difference between manual and nonmanual workers.
Long period of immobilization are not recommended. Lefevre-Colau et al. performed a randomized prospective study on 74 patients with an impacted proximal humerus fracture[25]. One group was treated with early mobilization of the shoulder (within 3 days after the fracture), while the other group was immobilized for 3 weeks followed by physiotherapy. They concluded that early mobilization was safe and allowed a quicker return to functional use of the affected limb. Practically, if a controlled X-ray does not show secondary displacement at 10 days, a passive mobilization should be encouraged.
Adjuvant procedures
Acromioplasty
Acromioplasty is not indicated for acute fractures, except perhaps to improve the workspace in the case of arthroscopic treatment.[26]
Long head of the biceps
The consequences of proximal humerus osteosynthesis are characterised by the development of rotator interval fibrosis and adhesions at the long head of the biceps. These result in reduced joint mobility which may explain the postoperative stiffness that is sometimes observed. Moreover, the tendon can become unstable and even interpose between fragments, preventing its reduction. Lastly, trauma causes tendinopathy and even lacerations that can lead to persistent pain. Therefore, it is recommended to routinely perform a tenodesis of the long head of the biceps by opening the rotator interval to explore the long head of the biceps tendon.[27][28][29][30][31]
This exposes the biceps and also provides a landmark to define the greater and lesser tuberosities for subsequent anatomic reduction. A tenotomy-tenodesis is performed with sutures joining the fibrous “roof” of the bicipital groove to the tendon. Alternatively, tenodesis may be performed lower to the pectoralis major tendon. This location facilitates visualization of the bicipital groove which can be used to assess version during the reconstruction. The intra-articular part of the tendon is then resected. The rotator interval is left open, so as to control reduction of the humeral head and tuberosity, and to limit mobility loss.
Osteosynthesis
Closed osteosynthesis (arthroscopy, percutaneous surgery, intramedullary nailing) should be contrasted with open procedures (transosseous suture, plate osteosynthesis). The first have two essential merits: reducing the risk of infection and avoiding the direct approach with its consequences (bone and soft tissue devascularization, postoperative adhesions). However, they only apply to extra-articular or less complex articular fractures, such as fractures of the surgical neck or type II cephalotubercular valgus impacted fractures. Several types of osteosynthesis have been used, from “osteosynthesis à minima” by osteosuture with nonabsorbable thread, to the solid screw epiphyseal plate or its derivatives.
Arthroscopy
The treatment of tuberosity (Figure 13 and Movie/Video 1) or humeral head fractures (Figure 14), with or without extension to the surgical neck, is now validated.

Surgical technique
This technique has many advantages including being minimal invasiveness and intra-articular and subacromial reduction control. However, it is technically demanding, and not an option for all surgeons and for all fractures. As a general guideline, arthrosopic fixation of the greater tuberosity is possible, if the thickest part of the fragment is less than 10 mm. Fractures with more distal extension can be challenging to secure laterally, if anchor-based fixation is attempted. Surgery is performed with the patient’s arm in light traction and placed in a half-seated or lateral decubitus position. The posterior approach is used, except posterior dislocation of the humeral head. Other approaches (lateral, anterior, ...) are performed on demand, depending on the fracture type. The hematoma is drained, and a suction pipe is connected directly to the trocar, allowing the joint to be filled and emptied until a satisfactory view is obtained. An intra-articular and then subacromial assessment is performed after a bursectomy. The type of fracture and its dimensions are assessed and the fractures reduced. Joint fractures do not necessarily require stabilization (concept of the egg cup). Several types of repair are recommended to obtain an anatomic reduction of the tuberosities (single point, double row or tension band).
Percutaneous Pinning or Screw Fixation
Commonly used in paediatric orthopaedics, this technique has also been performed in adults for over 50 years, particularly those with good bone quality and 2- or 3-part fractures.[33]
It is minimally invasive and therefore decreases the risk of vascular compromise. Another advantage of this technique is that it can be converted, at any time, if adequate reduction or stability cannot be obtained. Fractures are primarily stabilized with ascending fasciculated pins, using at least three diverging ‘palm tree’ pins in the epiphysis (Hacketal, Kapandji). Superior to inferior pins may also be used for greater tuberosity stabilization.
The percutaneous approach has been difficult to establish as a reference technique due to its many disadvantages. Firstly, it is contraindicated for type 2 to 4 articular fractures, with low bone density and significant comminution, all conditions are often found in elderly patients. Secondly, the variable mechanical quality of the synthesis obtained can lead to long periods of postoperative immobilization and therefore stiffness. Moreover, the reduction technique and pin placement are very demanding. Lastly, many complications such as migration or joint penetration by pins, as well as potential neurological lesions have been reported.[34][35][36][37][38] Moreover, there is a risk to injure important anatomic structures in the shoulder. Lateral pins should be distal enough to avoid injury to the anterior branch of the axillary nerve, and multiple fluoroscopic views should be obtained to avoid penetration of the humeral head cartilage. There may be a risk of injury of the cephalic vein, the biceps tendon, and the musculocutaneous nerve by anterior pins, and these pins should be employed with caution. Greater tuberosity pins should be placed with the arm in external rotation, should be aimed for at 20 mm from the inferior aspect of the humeral head, and should not overpenetrate the cortex.[38]
A special case, which immediately contraindicates osteosynthesis, is the external fixator used during polytrauma or open fractures with skin damage (Figure 15).
Surgical Technique
The patient is placed in a beach-chair position. The arm must be free, allowing the use of fluoroscopy installed close to the patient's head. The main objective is not necessarily a perfect anatomical reduction, but alignment of the fragments using gentle and non-traumatic manipulation. Closed reduction and percutaneous fixation of proximal humeral fractures, with or without screws, is based on external manoeuvres using ligamentotaxis.[39]
For ascending pinning, the pins must be curved at the end to allow for epiphyseal divergence. Pin insertion can be supraepitrochlear, supracondylar, median supraolecranean, or at the tip of the deltoid V. Each approach carries neurological risks related to the local anatomy or joint stiffness in the elbow. For direct pinning, if the reduction proves to be insufficient, a short superoexternal incision is made under fluoroscopic control at the lateral edge of the acromion. A deltoid split is performed without detachment from the acromion. A spatula or Rochet punch pressed against the epiphysio-metaphyseal hinge enables careful removal of the humeral head (Figure 16).
This surgical action often results in a spontaneous reduction of the tuberosities. Repositioning may also be facilitated by a bone hook placed in the subacromial space holding the greater tuberosity, while the arm is rotated externally. At this stage, the primary stability of the assembly is completed by pinning between the diaphysis and humeral head and between the tuberosity(s) and humeral head. Then cannulated screws of 4.0 mm or 4.5 mm diameter with washers can be inserted. Alternatively, threaded pins (which reduce the risk of recession compared to smooth pins) are cut, bent and left subcutaneously (Figure 17).
Percutaneous Antegrade Intramedullary Nailing
At first sight, fixation of an epiphysis by an intramedullary nail may seem heretical, but this concept has proved itself and is now validated. Because it is intramedullary, it represents biomechanically stable osteosynthesis (Figure 18), especially in cases of medial comminution.[40]
The latest nails now benefit from anteroposterior locks, which enable improved tuberosity reconstruction. It seems that adding an unlocked calcar screw in the context of an intramedullary nail does not improve biomechanical properties.[41]
For certain bifocal cephalotubercular and diaphyseal fractures, nailing is the treatment of choice (Figure 19).

The usual indications are subtubercular fractures, with or without a tuberosity shear, and type II cephalotubercular valgus impacted fractures. There are problems related to percutaneous intramedullary nailing. It requires multiple muscular and tendinous perforations (deltoid, rotator cuff) and potentially dangerous excisions. It also rules out simple adjuvant procedures, such as bone grafting, long head of the biceps surgery and cerclage of the tuberosities.
Surgical technique
This procedure is performed in the beach-chair position under fluoroscopic guidance. The incision is anterior or posterior (Neviaser's portal) at the acromioclavicular interval for valgus or varus misaligned fractures respectively. The nail must be inserted medially so as to pierce the head in a vascularized muscular, but not tendinous area. Therefore, it must pierce the humeral head in the cartilaginous area and not at the tuberosity. Distal locking (diaphyseal) is performed first, which enables compression of the fracture site by retrograde impaction using a weight. Compression is maintained by two or three proximal screws locked into the nail.
Osteosuture
Osteosuture includes open reduction and wire fixation. Strapping of the tuberosity is often sufficient to support the humeral head. Various adjuvant techniques having the same rationale can be applied: transosseous fixation, wires emanating from anchor point(s) or fixed on a diaphyseal screw as an external brace (Figure 20). This is a technically simple and rapid treatment. It is ideal for isolated and displaced tuberosity fractures and may also be used for type II cephalotubercular fractures.[42]

Operative technique
The patient is placed in a half-seated position. A 4-5 cm deltopectoral or transdeltoid approach is used, depending on the type of fracture (lesser or greater tuberosity). The fracture is located after a bursectomy. The rotator cuff is repaired using an anchor or transosseous sutures.
Plate osteosynthesis
Modern proximal humerus plating employs locking plates with improved biomechanical properties of fixation compared with traditional compression plates. This is particularly important for achieving fixation in the humeral head, where fixation must be unicortical. The angulation of the solid screws can be fixed or variable and various mechanisms are used for locking the screw in the plate (i.e. locking in its housing by a threaded lock nut, or threads in the screw head which lock into the plate). The plate permits 1) anatomic reduction, 2) surgery on the long head of the biceps, 3) transplant options (humeral head, or Bilboquet in cases of osteoporosis), and 4) a firm assembly stabilized by locked screws (i.e. not free anteroposterior screws) for the treatment of tuberosities and the humeral head in cases of ‘head split’ (Figure 21), and lastly, tension-band suturing of the rotator cuff/tuberosities to the plate. It is therefore preferred for type II to IV complex cephalotubercular fractures where osteosynthesis has been opted for (Video 2).
Initially, a high rate of humeral head perforation was reported with locking plate fixation. However, this was likely to due to lack of recognition (inadequate fluoroscopy) and the misconception that all screws must be long. The only locking screws that must be long are the lower calcar screws in cases of medial comminution (Figure 22). The upper screws must be short (maximum 35 mm) and serve only to stabilize the greater tuberosity.

Surgical Technique (Operative Treatment)
Deltopectoral approach
The deltopectoral approach is the most commonly used. It enables osteosynthesis in the vast majority of fractures. A small centimetric posterior approach may also be associated in cases of humeral head dislocation (Figure 23). In fact, the bicipital groove can often be the starting point for a fracture of the humeral head segment confined behind the glenoid.

The biceps tendon is tenodesed in most cases to facilitate reduction and identify the tuberosities. The upper border of the pectoralis major tendon can serve as a site of tenodesis. The subscapularis, supraspinatus, and infraspinatus are tagged with nonabsorbable sutures. These sutures are then subsequently passed through holes in the plate and to provide a tension-band construct. Such fixation often provides the best fixation of the tuberosities since the tendinous structures are often stronger than osteoporotic bone. The deltopectoral approach provides only a limited view of the greater tuberosity, which can be improved by putting the arm in abduction and internal rotation after placement of a Brown retractor.
The intertubercular fracture line is situated 8 mm lateral to the bicipital groove. At this stage, devascularization of the bone fragments should be avoided by conserving the anterior circumflex and ascending bicipital arteries. The idea is to stay lateral to the bicipital groove. The approach to the humeral head fragment is intertubercular by widening the separation of the two tuberosities. Reduction is performed using a 2.5 mm pin (Figure 24).
Distally, the anterior insertion of the deltoid is elevated using a periosteal elevator and the plate is slipped-in subperiosteally. The plate is temporarily secured with one cortical screw and then the height is adjusted as needed to ensure the that the inferior locking screws are at the medial calcar. To limit the length of the incision the distal screw is inserted obliquely. The sutures from the rotator cuff tendon may need to be passed through the plate prior to securing to the diaphysis depending on the plate design (Figure 25).

Transdeltoid approach
A so-called mini-invasive transdeltoid variant is an option. The patient is placed in a half-seated position. A 4-5 cm approach is used in line with the acromion. The axillary nerve is isolated and the plate is then slipped between the cortex and the nerve (Figure 26).
However, the authors of this article have stopped performing this approach because we have observed a higher rate of postoperative stiffness with this approach. Furthermore, implant removal for or conversion to arthroplasty (either at the initial surgery or for failure of fixation) is easier performed through a deltopectoral approach.
Complications of plate osteosynthesis
The following table summarizes the initial complication rate of proximal humeral fixation by plate.[43]
| Complication | Rate |
|---|---|
| Screw penetration | 33.3 |
| Osteonecrosis | 14.6 |
| Infection | 12.5 |
| Heterotopic ossification | 8.3 |
| Malunion | 8.3 |
| Removal of hardware | 8.3 |
| Hardware failure | 6.5 |
| Nonunion | 4.2 |
| Osteoarthrosis | 2.1 |
| Postoperative capsular contracture | 2.1 |
The risk of complications and the long-term outcomes in patients with a severely displaced fracture or a fracture-dislocation of the proximal part of the humerus treated with open reduction and plate fixation (ORIF) has been evaluated by Robinson et al.[44] They found 24% of postoperative stiffness, 7% of fixation failure/nonunion, and 4% of late osteonecrosis or posttraumatic osteoarthritis. The patients' mean levels of pain, function, and satisfaction with treatment were good to excellent, supporting the use of primary open reduction and plate fixation (ORIF) in medically fit patients with a severely displaced fracture or a fracture-dislocation of the proximal part of the humerus.[44] Wijgman et al. reviewed the results of 60 patients with 3 or 4 part fractures who underwent open reduction internal fixation (ORIF) with a T-plate or cerclage wires and found 87% had good/excellent results based on the Constant score[45]. Interestingly 22 pts (37%) had avascular necrosis, yet 17 of these 22 (77%) patients had excellent/good Constant scores.
Hemiarthroplasty
The simple humeral implant is a remedy in cases of technically impossible osteosynthesis or fractures posing a risk of significant necrosis in young patients. It is restricted to cephalotubercular fractures of types III to IV in young patients. Reconstruction requires restoration of the humeral length, correct implant retroversion, restoration of the epiphyseal width, stable implant fixation, and a robust osteosynthesis of the tuberosities.
Functional results vary depending on the patient’s age, and especially the anatomical consolidation of the tuberosities. They can be excellent when it comes to mobility and pain. But if the tuberosities are not consolidated, then mobility results are poor, with an average anterior elevation of 90°. They do, however, remain acceptable for pain.[46]
Surgical technique
The approach is most commonly deltopectoral. The joint is accessed by working through the fracture fragments in the setting of a 4-part fracture, or dividing the lesser and greater tuberosities in the setting of a 3-part fracture. The humeral head fragment is extracted. As with plate fixation, the rotator cuff is tagged with multiple sutures for subsequent fixation of the tuberosities.[47]
Correct positioning of the implant and the tuberosities is an essential step, which will determine the quality of the functional result (cf above?->see above). The lateral offset is restored either by introducing a graft between the implant and the greater tuberosity, if the implant does not fill the space, or by using a wide metaphyseal implant with no graft.[48]
Height can be assessed fluoroscopically by restoring a Gothic arch appearance or by locating the insertion point of the pectoralis major.[9][49]
In fact, the distance separating the upper edge of this tendon from the great tendon at the top of the humeral head is relatively constant (5.5 cm). With regard to the rotation of the implant, 20-30° retroversion (measured from a flexed elbow relative to the forearm) is normally recommended. This is 10° less than the anatomical retroversion, measured on the bi-epicondylar axis, taking into account the physiological valgus. Before implanting the final stem, a number 2.0 drill-hole is made at the metaphyseal level, through which two non-absorbable sutures are threaded to be used for fixation of the tuberosities in the vertical plane.
The stems may be cemented or non-cemented. The cement mantle should not reach the tuberositis which could jeopardise their integration.[50]
A “black and tan” technique is an effective method for ensuring this. The implant is reduced and the tuberosities are stabilized using Boileau’s technique.[34]
Reverse Shoulder Arthroplasty
In patients aged over 65 with highly comminuted fractures, a compromised rotator cuff, articular surface disruption, a short metaphyseal hinge, initial varus angulation > 20 degrees, or fracture dislocation, reverse implants are now more frequently performed than osteosynthesis and hemiarthroplasty. A systematic review of level I and II studies shows that reverse shoulder arthroplasty (RSA) grants better outcomes and is associated with fewer complications than hemiarthroplasty at short term follow-up.[51]
Effectively, for these elderly patients, with comorbidities and osteoporosis, hemiarthroplasty failure is a significant risk. While reverse shoulder arthroplasty does not rely as much on tuberosity healing, function proves to be higher when the tuberosities heal. Therefore, the tuberositis should be preserved and every effort should be made to achieve healing in the setting of reverse shoulder arthroplasty. Reverse shoulder arthroplasty is contraindicated in young and active patients, apart from exceptional lifesaving situations, and in cases of infection or when the axillary nerve is involved. In fact, except for partial mobility recovery, the complication rate remains high.[52]
Surgical (Operative) Technique
Apart from time spent on the glenoid, implantation is in all respects similar to hemiarthroplasty. Exposure of the glenoid is easy given the absence of the proximal humerus. The glenoid cartilage is then removed using a curette and carefully milled by hand, given the absence of osteoarthritis. The glenoid baseplate should be placed so that the glenosphere is flush or slightly overhangs the lower edge of the glenoid (Figure 27) to avoid frictional impingements.[53] Jain et al. performed a systematic review to compare clinical and functional outcomes of reverse shoulder arthroplasty in proximal humeral fractures with and without tuberosity healing. They reported that reverse shoulder arthroplasty with healed greater tuberosity showed better range of motion, especially forward flexion and external rotation and Constant scores, compared with the nonhealed greater tuberosity. Repairing tuberosities improve rotations and anterior stability.[54][55] Reverse shoulder arthroplasty for fracture with a 135° prothesis inclination is associated with higher tuberosity healing rates compared with 145° or 155°.[55] Cemented stems are usually preferred to cemented stems due to poor bone quality and lower revision rate according to the Australian registry.
The glenosphere should preferably be neutral or only minimally lateralized. In our experience lateralized and inferior eccentric glenospheres are associated with lower rates of tuberosity healing (unpublished data). The implant is then reduced and the tuberosities reinserted according to the technique described by Boileau et al.[34] Higher rates of tuberosity healing have been reported with 135 degrees stems as opposed to 155 degrees stems, but no study has directly compared these to date.

Rehabilitation
Rehabilitation (or the absence thereof) after a proximal humerus fracture is crucial, and partly conditions the outcome.
After surgery everything conspires to create a stiff shoulder: the patient’s fear, pain, hemarthrosis and periarticular hematoma, muscle contusion, capsular tear, bicipital tendinopathy, etc. Ideally, the shoulder should be rehabilitated as soon as possible, depending on the stability of the osteosynthesis. Once mobility has been regained, we never recommend reinforcement, but rather a gradual and reasonable resumption of activity.[56]
In general, the hand, wrist and elbow should be actively mobilized as soon as possible.
Stable Osteosynthesis
These are fixations obtained using antegrade intramedullary nailing or plates. Assisted active mobilization can be immediate. No immobilization is recommended. Physiotherapy is only intra-hospital the day after surgery to teach a rehabilitation protocol.[57]
Osteosynthesis with Relative Stability
This type of rehabilitation applies to osteosuture and screwing of the tuberosities. Early and aggressive rehabilitation can in fact be harmful by provoking secondary displacement. The patient is immobilized using a sling elbow at the side or neutral abduction-rotation pillow, depending on the tuberosities involved (lesser and greater, respectively). Passive mobilization is recommended, as short pendulum exercises repeated at least 5 times a day, elevation by self mobilization in the supine position, elbow stretched, with slow, highest possible elevations, and rotations with elbows bent at 90°, using a baton held in both hands, but only mobilized by the healthy upper limb.[58]
‘Dry’ physiotherapy or balneotherapy may be prescribed. It includes progress monitoring and correct performance of the exercises, patient motivation, relaxing massages of the scapular belt and passive mobilization exercises.
Non-stable osteosynthesis and implants
Fasciculated retrograde nailing, insertion, partial fixation and implants are usually immobilized for one month to allow consolidation of the fragments. Physiotherapy is deferred until later.
Decision Making
Successful treatment depends not only on technical, but also decision-making capabilities. Evidence confirming the best treatment for these fractures is lacking. However, it has recently been shown that the therapeutic consensus is directly correlated with the surgery success.[59][60] Operative management should be considered in patients with head splitting proximal humerus fractures and in those with dislocations that cannot be reduced. Surgical management is also considered in proximal humerus fractures associated with humeral shaft fractures.
Humeral head fractures
It is difficult to codify the treatment of such a rare fracture. The following guidelines, though not based on experience, have the merit of common sense. In the elderly, the risk of humeral head necrosis immediately invokes reverse shoulder arthroplasty. In young patients, simple reduction, with or without associated osteosynthesis using screws or pins, seems valid.[32]
Displaced tuberosity fractures with a stable epiphyseal-diaphyseal union
Surgical management is considered in fractures where the greater tuberosity is displaced >5 mm. If the fragment is small and considered to be a type A1 bony rotator cuff lesion, then arthroscopic reinsertion or open osteosuture gives similar results. A large and solid fragment lends itself to screwing and nailing, while osteosuture will be preferred in cases of porous and split bone.[61][62]
Type II-IV cephalotubercular in the young
It seems acceptable to restore anatomy in young or biologically healthy patients. Epiphyseal plate osteosynthesis and antegrade nailing give similar results. The first one is preferred in cases when the medial hinge is preserved. Erasmo et al. examined of 82 cases of humerus fracture dislocations treated with the lateral locking plates. Overall outcomes were excellent to good based on standard scoring systems. Complications included avascular necrosis (12%), varus positioning of the head (4.8%), impingement syndrome (3.6%), secondary screw perforation (3.6%), non-union (2.4%) and infection (1.2%).[63] Robinson et al. looked at severely impacted valgus proximal humeral fractures treated with open reduction internal fixation in young patients[64]. Anatomic reduction is required with lateral plating to re-establish the normal head/neck angle. Good to excellent results were achieved with fixation methods.
Hemiarthroplasty is justified when there is a high risk of humeral head necrosis.[65]
Type II-IV cephalotubercular in the elderly
It seems reasonable to immediately resort to reverse shoulder arthroplasty in elderly patients having many comorbidities and lesser functional needs. A reverse implant seems all the more indicated when the displacement is large. The best treatment is osteosynthesis, then any conservative treatment, and lastly hemiarthroplasty. Osteosynthesis is the option having the most frequent revisions according to a recent meta-analysis.[66][67]
Isolated sub-tubercular fractures
Closed nailing or plate osteosynthesis are coeval. Plates are preferred in young patients to conserve their rotator cuff and facilitate their removal, and nails are used in older patients for whom removal of material is debatable. Fasciculated nailing is reserved for paediatric cases as it has not been proven in adults in comparative studies.[68][69]
References
- ↑ Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg. 2017;26:2117-24.
- ↑ Kannus P, Niemi S, Sievanen H, Parkkari J. Stabilized Incidence in Proximal Humeral Fractures of Elderly Women: Nationwide Statistics From Finland in 1970-2015. J Gerontol A Biol Sci Med Sci. 2017;72:1390-3.
- ↑ Sumrein BO, Huttunen TT, Launonen AP, Berg HE, Fellander-Tsai L, Mattila VM. Proximal humeral fractures in Sweden-a registry-based study. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2017;28:901-7.
- ↑ 4.0 4.1 Pearl ML, Volk AG. Coronal plane geometry of the proximal humerus relevant to prosthetic arthroplasty. J Shoulder Elbow Surg. 1996;5:320-6.
- ↑ 5.0 5.1 5.2 Lädermann A, Denard PJ, Burkhart SS. Arthroscopic management of proximal humerus malunion with tuberoplasty and rotator cuff retensioning. Arthroscopy. 2012;28:1220-9.
- ↑ Blix M. Die lange und die spannung des muskels. Skand Arch Physiol 1892;3:295-318.
- ↑ Murachovsky J, Ikemoto RY, Nascimento LG, Fujiki EN, Milani C, Warner JJ. Pectoralis major tendon reference (PMT): a new method for accurate restoration of humeral length with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2006;15:675-8
- ↑ Sahu D, Jagiasi JD, Valavi AS, Ubale T. The Distance between the Pectoralis Major Tendon Insertion and the Top of the Humeral Head is a Reliable Landmark: An Anatomic Study. Joints 2019;7:37-40
- ↑ 9.0 9.1 Kim BS, Kim DH, Song KS, Min BW, Bae KC, Cho CH. Is the pectoralis major tendon a reliable reference for restoration of humeral length with fracture hemiarthroplasty? J Shoulder Elbow Surg. 2018;27:e45-e9
- ↑ Greiner SH, Kääb MJ, Kröning I, Scheibel M, Perka C. Reconstruction of humeral length and centering of the prosthetic head in hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2008;17:709-14
- ↑ Torrens C, Corrales M, Melendo E, Solano A, Rodríguez-Baeza A, Cáceres E. The pectoralis major tendon as a reference for restoring humeral length and retroversion with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2008;17:947-50
- ↑ Cikes A, Trudeau-Rivest E, Canet F, Hebert-Davies J, Rouleau D. Repositioning of the humeral tuberosities can be guided by pectoralis major insertion. Strat Traum Limb Recon 2014;9:127-131
- ↑ 13.0 13.1 Lädermann A, Denard P, Abrassart S, Schwitzguébel A. Achilles Tendon Allograft for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity: A Case Report. Knee Surg Sports Traumatol Arthrosc. 2017;25:2147-50
- ↑ Vandenbussche E, Peraldi P, Naouri JF, Rougereau G, Augereau B. Four part valgus impacted fractures of the upper extremity of humerus: ilium graft reconstruction. Apropos of 8 cases. Rev Chir Orthop Reparatrice Appar Mot. 1996;82:658-62.
- ↑ Levy JC, Badman B. Reverse shoulder prosthesis for acute four-part fracture: tuberosity fixation using a horseshoe graft. J Orthop Trauma. 2011;25:318-24.
- ↑ Boileau P, Walch G. The three-dimensional geometry of the proximal humerus. Implications for surgical technique and prosthetic design. J Bone Joint Surg Br.1997;79:857-65.
- ↑ Hettrich CM, Boraiah S, Dyke JP, Neviaser A, Helfet DL, Lorich DG. Quantitative assessment of the vascularity of the proximal part of the humerus. J Bone Joint Surg Am. 2010;92:943-8
- ↑ Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427-33
- ↑ Cetik O, Uslu M, Acar HI, Comert A, Tekdemir I, Cift H.Is there a safe area for the axillary nerve in the deltoid muscle? A cadaveric study. J Bone Joint Surg Am. 2006;88:2395-9
- ↑ Duparc J. Classification des fractures articulaires de l'extrémité supérieure de l'humérus [Classification of articular fractures of the upper extremity of the humerus]. Acta Orthop Belg. 1995;61 Suppl 1:65-70. French.
- ↑ Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79:203-7
- ↑ 22.0 22.1 Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg. 2009;18:612-21
- ↑ Court-Brown CM, McQueen MM. The impacted varus (A2.2) proximal humeral fracture: prediction of outcome and results of nonoperative treatment in 99 patients. Acta Orthop Scand. 2004;75:736-40
- ↑ Tejwani NC, Liporace F, Walsh M, France MA, Zuckerman JD, Egol KA. Functional outcome following one-part proximal humeral fractures: a prospective study. J Shoulder Elbow Surg. 2008;17:216-9
- ↑ Lefevre-Colau MM, Babinet A, Fayad F, Fermanian J, Anract P, Roren A, Kansao J, Revel M, Poiraudeau S. Immediate mobilization compared with conventional immobilization for the impacted nonoperatively treated proximal humeral fracture. A randomized controlled trial. J Bone Joint Surg Am. 2007;89:2582-90
- ↑ Charbonnier C, Chague S, Kevelham B, Preissmann D, Kolo FC, Rime O, Laedermann A. ArthroPlanner: a surgical planning solution for acromioplasty. International journal of computer assisted radiology and surgery 2018;13:2009-2019
- ↑ McGahan PJ, Patel H, Dickinson E, Leasure J, Montgomery W, 3rd. The effect of biceps adhesions on glenohumeral range of motion: a cadaveric study. J Shoulder Elbow Surg. 2013;22:658-65.
- ↑ Visser JD, Rietberg M. Interposition of the tendon of the long head of biceps in fracture separation of the proximal humeral epiphysis. Neth J Surg. 1980;32:12-5.
- ↑ Kim JM, Jupiter JB. Traumatic laceration of the long head of the biceps brachii from a displaced surgical neck fracture of the humerus: case report. Journal of surgical orthopaedic advances. 2011;20:252-4.
- ↑ Soliman OA, Koptan WM. Proximal humeral fractures treated with hemiarthroplasty: does tenodesis of the long head of the biceps improve results? Injury 2013;44:461-4.
- ↑ Tosounidis T, Hadjileontis C, Georgiadis M, Kafanas A, Kontakis G. The tendon of the long head of the biceps in complex proximal humerus fractures: a histological perspective. Injury 2010;41:273-8.
- ↑ 32.0 32.1 Godeneche A, Freychet B, Gunst S, Daggett M, Viste A, Walch G. Arthroscopic Reduction of Acute Traumatic Posterior Glenohumeral Dislocation and Anatomic Neck Fracture Without Internal Fixation: 2-Year Follow-up. Orthop J Sports Med. 2017;5:2325967117745486
- ↑ 33.0 33.1 Bohler J. [Treatment of open diaphysial fractures of the long bones]. Acta Orthop Belg.1962;28:450-76. French
- ↑ 34.0 34.1 34.2 Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011;20(2 Suppl):S47-60.
- ↑ Yoon TH, Choi CH, Choi YR, Oh JT, Chun YM. Clinical outcomes of minimally invasive open reduction and internal fixation by screw and washer for displaced greater tuberosity fracture of the humerus. J Shoulder Elbow Surg 2018;27:e173-e177.
- ↑ Keener JD, Parsons BO, Flatow EL, Rogers K, Williams GR, Galatz LM. Outcomes after percutaneous reduction and fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16:330-8.
- ↑ Kamineni S, Ankem H, Sanghavi S. Anatomical considerations for percutaneous proximal humeral fracture fixation. Injury 2004;35:1133-6.
- ↑ 38.0 38.1 Rowles DJ, McGrory JE. Percutaneous pinning of the proximal part of the humerus. An anatomic study. J Bone Joint Surg Am. 2001;83:1695-9.
- ↑ Brooks CH, Revell WJ, Heatley FW. Vascularity of the humeral head after proximal humeral fractures. An anatomical cadaver study. J Bone Joint Surg Br. 1993;75(1):132-6.
- ↑ Clavert P, Hatzidakis A, Boileau P. Anatomical and biomechanical evaluation of an intramedullary nail for fractures of proximal humerus fractures based on tuberosity fixation. Clinical biomechanics. 2016;32:108-12.
- ↑ Katthagen JC, Schwarze M, Bauer L, Meyer-Kobbe J, Voigt C, Hurschler C, Lill H Is there any advantage in placing an additional calcar screw in locked nailing of proximal humeral fractures? Orthop Traumatol Surg Res (OTSR) 2015;101:431-5.
- ↑ Hawkins RJ, Kiefer GN. Internal fixation techniques for proximal humeral fractures. Clin Orthop Relat Res. 1987;223:77-85.
- ↑ Fisher ND, Barger JM, Driesman AS, Belayneh R, Konda SR, Egol KA. Fracture Severity Based on Classification Does Not Predict Outcome Following Proximal Humerus Fracture. Orthopedics 2017;40:368-374
- ↑ 44.0 44.1 Robinson CM, Stirling PHC, Goudie EB, MacDonald DJ, Strelzow JA. Complications and Long-Term Outcomes of Open Reduction and Plate Fixation of Proximal Humeral Fractures. J Bone Joint Surg Am. 2019;101:2129-2139
- ↑ Wijgman AJ, Roolker W, Patt TW, Raaymakers EL, Marti RK. Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Am. 2002;84:1919-25
- ↑ Boileau P, Winter M, Cikes A, Han Y, Carles M, Walch G, Schwartz D.G. Can surgeons predict what makes a good hemiarthroplasty for fracture? J Shoulder Elbow Surg. 2013;22:1495-506.
- ↑ Collin P, Laubster E, Denard PJ, Akuè FA, Lädermann A. The Nice knot as an improvement on current knot options: A mechanical analysis. Orthop Traumatol Surg Res (OTSR) 2016;102:293-6.
- ↑ White JJ, Soothill JR, Morgan M, Clark DI, Espag MP, Tambe AA. Outcomes for a large metaphyseal volume hemiarthroplasty in complex fractures of the proximal humerus. J Shoulder Elbow Surg. 2017;26:478-83.
- ↑ Krishnan SG, Bennion PW, Reineck JR, Burkhead WZ. Hemiarthroplasty for proximal humeral fracture: restoration of the Gothic arch. Orthop Clin North Am. 2008;39:441-50.
- ↑ Singh A, Padilla M, Nyberg EM, Chocas M, Anakwenze O, Mirzayan R, Yian EH, Navarro RA. Cement technique correlates with tuberosity healing in hemiarthroplasty for proximal humeral fracture. J Shoulder Elbow Surg. 2017;26:437-42.
- ↑ Lädermann, A. Chiu, JC. Collin, P. Piotton, S. Nover, L. Scheibel, M. Hemi- vs reverse shoulder arthroplasty for acute proximal humeral fractures. Obere Extremität 2019;14:127–35.
- ↑ Ek ET, Neukom L, Catanzaro S, Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199-208.
- ↑ Lädermann A, Gueorguiev B, Charbonnier C, Stimec BV, Fasel JHD, Zderic I, Hagen J, Walch G. Scapular Notching on Kinematic Simulated Range of Motion After Reverse Shoulder Arthroplasty Is Not the Result of Impingement in Adduction. Medicine (Baltimore). 2015;94:e1615.
- ↑ Jain NP, Mannan SS, Dharmarajan R, Rangan A. Tuberosity healing after reverse shoulder arthroplasty for complex proximal humeral fractures in elderly patients-does it improve outcomes? A systematic review and meta-analysis. J Shoulder Elbow Surg 2019;28:e78-e91
- ↑ 55.0 55.1 O'Sullivan J, Lädermann A, Parsons BO, Werner BC, Steinbeck J, Tokish JM, Denard PJ.A Systematic Review of Tuberosity Healing and Outcomes following Reverse Shoulder Arthroplasty for Fracture According to Humeral Inclination of the Prosthesis. J Shoulder Elbow Surg. 2020; 29:1938-49
- ↑ Charbonnier C, Lädermann A, Kevelham B, Chague S, Hoffmeyer P, Holzer N. Shoulder strengthening exercises adapted to specific shoulder pathologies can be selected using new simulation techniques: a pilot study. Int J Comput Assist Radiol Surg. 2018;13:321-330.
- ↑ Liotard J. Rééducation d’une épaule douloureuse : comment faire simple [Painful shoulder rehabilitation: How to do it simple] Revue du rhumatisme monographies. 2010;77:239-45. French
- ↑ Denard PJ, Lädermann A, Burkhart SS. Prevention and management of stiffness after arthroscopic rotator cuff repair: systematic review and implications for rotator cuff healing. Arthroscopy. 2011;27:842-8.
- ↑ Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015;11:CD000434.
- ↑ LaMartina J, 2nd, Christmas KN, Simon P, Streit JJ, Allert JW, Clark J, Otto RJ, Abdelfattah A, Mighell MA, Frankle MA. Difficulty in decision making in the treatment of displaced proximal humerus fractures: the effect of uncertainty on surgical outcomes. J Shoulder Elbow Surg. 2018;27:470-7.
- ↑ Liao W, Zhang H, Li Z, Li J. Is Arthroscopic Technique Superior to Open Reduction Internal Fixation in the Treatment of Isolated Displaced Greater Tuberosity Fractures? Clin Orthop Relat Res. 2016;474:1269-79.
- ↑ Lädermann A, Burkhart SS, Hoffmeyer P, Neyton L, Collin P, Yates E, Denard PJ. Classification of full-thickness rotator cuff lesions: a review. EFORT Open Rev. 2017;1:420-30.
- ↑ Erasmo R, Guerra G, Guerra L. Fractures and fracture-dislocations of the proximal humerus: A retrospective analysis of 82 cases treated with the Philos(®) locking plate. Injury 2014;45 Suppl 6:S43-8
- ↑ Robinson CM, Khan LA, Akhtar MA. Treatment of anterior fracture-dislocations of the proximal humerus by open reduction and internal fixation. J Bone Joint Surg Br. 2006;88:502-8.
- ↑ Gadea F, Favard L, Boileau P, Cuny C, d'Ollone T, Saragaglia D, Sirveaux F, SoFCOT. Fixation of 4-part fractures of the proximal humerus: Can we identify radiological criteria that support locking plates or IM nailing? Comparative, retrospective study of 107 cases. Orthop Traumatol Surg Res (OTSR) 2016;102:963-70.
- ↑ Du S, Ye J, Chen H, Li X, Lin Q. Interventions for Treating 3- or 4-part proximal humeral fractures in elderly patient: A network meta-analysis of randomized controlled trials. Int J Surg. 2017;48:240-6.
- ↑ van der Merwe M, Boyle MJ, Frampton CMA, Ball CM. Reverse shoulder arthroplasty compared with hemiarthroplasty in the treatment of acute proximal humeral fractures. J Shoulder Elbow Surg. 2017;26:1539-45.
- ↑ Lee W, Park JY, Chun YM. Operative Treatment of 2-Part Surgical Neck Fracture of the Humerus: Intramedullary Nail Versus Locking Compression Plate With Technical Consideration. J Orthop Trauma. 2017;31:e270-e4.
- ↑ Milin L, Sirveaux F, Eloy F, Mainard D, Mole D, Coudane H. Comparison of modified Hackethal bundle nailing versus anterograde nailing for fixation of surgical neck fractures of the humerus: retrospective study of 105 cases. Orthop Traumatol Surg Res (OTSR) 2014;100:265-70.
Proximal Humeral Fracture Sequelae
Bullet Points
Keywords
Prevalence
Types of Fracture Sequelae and Classification
Treatement
Conservative Treatment (Nonoperative Treatment)
Surgical Technique (Operative Treatment)
Treatment of a chronic nonunion of the proximal humerus in the elderly should be treated with fixation when possible (Figure 1 and Video 1). Critical attention should be paid to correct all deformities: tuberosity positioning, articular surface realignment, soft tissue balancing, and treatment of soft tissue contractures. Attempts at anatomic total shoulder arthroplasty have failed. Reverse shoulder arthroplasty is generally recommended when the fracture has eroded enough to prevent successful fixation, if the tuberosities have resorbed, if the rotator cuff is torn, or other findings are present that would limit the success rate of fixation.
The referenced article by Cheung et Sperling[1] reviews treatment options for proximal humeral nonunions and reports successful use of arthroplasty in treating elderly osteoporotic proximal humeral nonunions as a pain-relieving procedure.
References
- ↑ Cheung EV, Sperling JW. Management of proximal humeral nonunions and malunions. Orthop Clin North Am. 2008;39:475-82
What would Codman have thought about this?
Fractures in relation to the subacromial bursa
I DO not intend to describe in detail the diagnosis or treatment of fractures about the shoulder, but to state briefly certain points which are suggested from a study of the bursa and tendons, and their probable relations to the fragments in the various types of bone injury.
It is an interesting fact that the acromion process, although so obviously exposed to any blow in this region, nevertheless is rarely broken. One reason is because the scapula is loosely attached to the chest wall and has no direct connection with the rest of the skeleton, except through the articulation at the inner end of the clavicle. A direct downward force striking on the acromion process meets little resistance, for the whole shoulder yields unless the line of the force is transmitted in whole or in great part to the clavicle. As a rule, downward forces acting on the acromion tilt the lower angle of the scapula inward and the blow slides off the shoulder, leaving only an abrasion of the skin at the point of impact. The acromio-clavicular ligaments may be ruptured if the acromion does not thus elude the full drive of the blow.
In the case of most blows or falls on the shoulder the scapula will merely be knocked downward or to the side in one direction or the other, and the strain of the blow will be taken by the muscles which hold the scapula in place. If the line of force is nearly or directly in the line of the axis of the clavicle, the latter will be broken or its ends will be dislocated. The great exception to this rule that the whole shoulder will yield before the acromion will be broken, is when the nature of the downward force is direct and also sudden, as from some heavy object; e.g., an iron bar striking the acromion. In such a case, the shoulder as a whole does not have time to move, so that the acromion or its base may be broken directly beneath the object with which the blow is struck. Such fractures, although often comminuted, are not usually of a complicated character or difficult to treat, because even though the inertia resists most of a sudden blow, a certain amount of yielding of the whole shoulder takes place and the fragments are not driven far out of position. Also there is much fibrous tissue to hold the fragments together. The bursa is in direct relation with part of the under surface of the acromion and might fill with blood, but I have never opened the bursa in such a case and demonstrated hemorrhage.
Injuries affecting this region by indirect violence (as in hyper-abduction of the arm in falling) very rarely injure the acromion, or even dislocate the acromio-clavicular joint, although the latter is obviously weaker than the bone of the acromion. This is probably due to the fact that the clavicular part of the joint lies above the acromial part. When the violence is indirect it must be transmitted through the acromion as a fulcrum, yet the latter does not break. As Stevens says, the edge which receives the strain is built like a Roman arch.
The coracoid process is also a very firm piece of bone and rarely is affected by any kind of violence, direct or indirect. Fracture of its base in conjunction with fracture of the scapula is not very uncommon.
The outer end of the clavicle does not lie in direct relation to the subacromial bursa, for the coraco-acromial ligament is between them. This portion of the clavicle is seldom fractured, except by direct blows, although fractures often occur at the junction of the middle and outer thirds.
In all forms of violent injuries to the shoulder, the upper end of the humerus is the part most commonly injured, because its structure is much less firm than that of the acromion and coracoid, and because of the leverage which may be exerted by the shaft of the humerus. The long arm of the lever of the humerus applies the force with the acromion as a fulcrum in the neighborhood between the surgical and anatomic necks of the bone, which necessarily receive the strain when the humerus is abducted or elevated. The upper edge of the glenoid, to which the biceps tendon guides the tuberosities, acts like a wedge to separate the tuberosities from the articular head. (Plate IX.) The acromion acts as a fulcrum applied to the region of the neck at the base of the greater tuberosity. The articular head of the bone is then either dislocated or broken off at the sulcus. Often it suffers both injuries to some degree. (See Fig. 57.) If the articular head becomes free and remains displaced, the injury is called a fracture-dislocation.
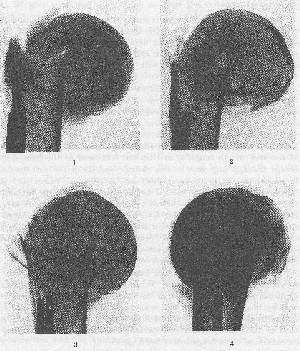
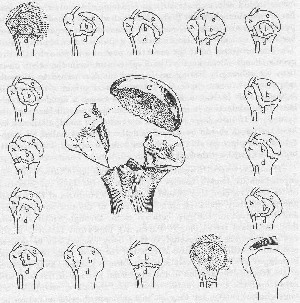
Reference to Fig. 60 shows that the epiphyseal line is retained in adult life as a thin wedge-shaped subdivision, marking off the tuberosities and ihe anatomic head from the diaphysis. The lines of cleavage of most fractures in this region follow near these old lines of epiphyseal union, and the head of the bone tends to become divided into four main fragments, or various combinations of these four fragments.
The tuberosities break off from the shaft at or near the transverse epiphyseal line, and the two tuberosities are also frequently partially separated by a line of fracture down the bicipital groove, this line representing very nearly their former vertical epiphyseal union. The fragments of the tuberosities usually remain in continuity with the tendinous insertions of the short rotators which are attached to them. The articular head forms the third unit and the shaft the fourth.
Since the base of the bursa is firmly attached to the periosteum of the greater tuberosity and the distal three-fourths inch of the supraspinatus tendon, this part of the bursa tends to remain in normal relations with the tendon and the tuberosity, while the sub-coracoid portion may remain with the lesser tuberosity and the subscapularis.
The anatomic head completely covered with its cartilage may be separated from the bone at the line of the sulcus which surrounds it, and become entirely free. This fragment may be displaced in various directions. If the violence is great, and probably even if it is only of moderate degree, the inferior, weak part of the capsule of the joint is usually badly torn or peeled away from the anterior part of the neck of the scapula, so that the free head of the bone may escape through any rent in this capsule and lie in the soft tissue. It is perhaps better to say it may be "left behind," than that it "escapes." In one such case, I found the head with its surfaces reversed, lying beneath the deltoid (Fig. 57). In another such case, I removed it from the areolar tissue in the axilla and by a sabre-cut incision replaced it again in its proper position. In the first case the anatomic head was left behind where it had been displaced in the erect phase, while in the second case it was left behind in the later phase when the humerus had come to the side.
The tuberosities, on the other hand, being attached to the short rotators, do not tend to escape. When one operates on cases of this kind, one finds the fragments of the tuberosities held in on the glenoid by the short rotators as a man might take his hat and hold it on the further side of a tree which he clasped with his hands. The head of the bone, whether free or still attached to the shaft, may lie outside of these fragments. (See Fig. 58.)
In these complicated cases, the subdeltoid portion of the bursa is of course often torn to some extent, but the portion beneath the acromion is scarcely affected. In other words, the under surface of the acromion, the supraspinatus tendon, and the external surface of the tuberosity are still covered with synovial membrane. When all the fragments are replaced, the major portion of the bursa may be still undamaged. Even when the bursa is torn on its periphery, it tends to heal readily and may be replaced by small bursal sacs, which together perform the function of the undamaged normal sac.
In less complicated fractures where displacement has not taken place, the subacromial bursa is probably torn very little. I am inclined to think that in simple fractures, as of the tuberosity, it is not torn at all. The fact that the recovery from fractures of the tuberosity which are not much displaced is rapid, and experience in the two following cases make me feel quite certain of this position.
CASE REPORTS
Mr. E. A. F. Age 36. Massachusetts General Hospital No.145677 E. S., Dec. 21, 1905.
The X-ray in this case showed a fracture of the tuberosity of the humerus. In the belief that the tuberosity had been pulled off by the supraspinatus and might be replaced accurately, the bursa was explored. It was found, however, that the whole bursa was normal. The line of fracture could be felt through the base of the bursa indistinctly, but it was thought best not to undertake any further exploration. Recovery was uneventful.
No. 10. Mr. M. McD. Age 23. Massachusetts General Hospital No. 174045 E. S., Jan. 20, 1911. In a similar case exploration showed that the bursa was intact and the tuberosity was satisfactorily uniting to the surface from which it was torn.
Figure 60 illustrates schematic drawings of the usual forms of fracture in this neighborhood. Naturally, I am unable to state that these are positive findings; they are only positive in the two cases referred to above and in a number of more complicated cases on which I have done operations. Most of these fractures are not complicated by disturbance of the function, and unite readily because the raw surfaces of bone are virtually in contact and are not bathed in joint fluid. Even if a little joint fluid can obtain access to them their own bleeding and clotting displaces it. This is not so with cases in which the evulsed fragment is small, and in which the bridging of the tissue must take place through a space constantly bathed in synovial fluid. To my mind in many other fractures such as those of the scaphoid in the wrist and of the femoral neck, the principle holds good that free access of synovial fluid to unapposed raw bone surfaces delays union.
If one realizes that the tuberosities have tendons firmly attached to their upper edges and that the base of the subacromial bursa is firmly attached to their superficial surfaces, and that they are usually concavo-convex pieces of cortex, frequently partially still attached to the periosteum on their lower edges, and more or less retained in place by the biceps tendon, it should be easier to reduce these fractures and to care for them intelligently.
The fact that the short rotators have firm holds on these fragments should help us materially in replacing them. If the fragment has the position shown in Plate IX, which we may consider the usual position, we are likely to be able to reduce it by carrying the elbow backward and inward, thus exerting a pull on the supraspinatus. The fragment may be at the same time pushed into place by the surgeon's thumb. Occasionally the displacement is in the other direction, the tuberosity having been pulled too far inward by the sub-scapularis. In some cases, the fragment having been pulled by the supraspinatus too far under the acromion causes a decided obstacle, because in abduction it impinges between the humeral head and the acromion. If such cases cannot be corrected by manipulation, I believe the bursa should be incised and the fragment pulled back and retained in place by sutures, or even screwed or nailed down to its bed in the greater tuberosity.
If such retracted fragments are very small, as in cases where the supraspinatus tendon carries a portion of the facet of insertion under the acromion, they should be classed as ruptures of the tendon, and immediately operated upon. The sizes of the raw bone surfaces and the extent of the gap between them, through which synovial fluid may pass from joint to bursa, are important factors. If the raw surfaces are large enough so that bony contact can be secured and maintained, union will occur, but if the bit of bone is small and is dragged away by the tendon, the problem is the same as in rupture of the tendon. Separation of the superficial portion of the facet and rupture of the supraspinatus tendon are, therefore, essentially the same clinical entity, for they make a permanent communication between joint and bursa. Since this gap never heals and remains a cause of persistent irritation, the patient is usually worse off than if the lesion were a much more extensive fracture.
It is interesting to speculate as to the behavior of the biceps tendon and of its sheath in cases of fracture in this region. Anatomically in a normal patient, the long tendinous head of the biceps has its origin at the fibrous rim of the upper edge of the glenoid. Occasionally the whole tendon or a part of it may arise from the adjacent portion of the capsule as a developmental error, for normally the biceps tendon in the embryo is first a part of the capsule and then separates from it. In the normal case there is no mesentery, or any form of sheath or other attachment, covering the biceps tendon as it traverses the joint between the cartilaginous head and the under surface of the capsule, until it reaches the intertubercular notch and descends into the bicipital groove. Here there is a synovial lined canal two or three inches long, which is a direct extension of the joint. The head of the humerus, using this tendon and its canal as a guide, runs up and down. It is not a fact, as may be superficially thought, that the long head of the biceps runs up and down in the groove when we move our forearms. To obtain motion between the biceps tendon and the bicipital groove in the humerus, one must move the scapulo-humeral joint. The expansion or contraction of the biceps muscle itself does not move the tendon in the groove, although it increases tension in that tendon. Extension of the elbow will also increase the tension in the tendon, although it will not move it. When the tendon is a little way down in the groove, it gets its blood supply through a mesentery-like fold in the lower portion of the sheath. That this tendon has a very superficial blood supply is sometimes beautifully demonstrated at operations for rupture of the supraspinatus. It may be seen crossing the gap, and is of a bright pink color, owing to the congestion of fine superficial blood vessels. This lower portion or sheath, where the synovial membrane ceases, necessarily has a certain amount of movement from the areolar tissue around it, which allows for play just above the belly of the biceps muscle. Fractures in this region, e.g., the typical fractures of the greater tuberosity, do not tear the tendon out of the groove on the distal fragment or on the proximal; in fact, the periosteum usually is only bent at the lower point and is not entirely disrupted. The tendon of the pectoralis major holds the distal portion of the biceps tendon in contact with the shaft.
Since the biceps may function in any position of the gleno-humeral joint, whether the latter is adducted, abducted, internally or externally rotated, the relation of the biceps tendon to the articular surface of the humerus is constantly changing. Bearing these functions in mind, let us consider what would happen when the typical fracture of the head of the bone occurs in three or four fragments. In a typical fracture in the pivotal position, the tendon would not be involved until the descent of the arm, when it might either be caught among the fragments, or might function in helping to realign them.
It seems to me highly probable that the lines of cleavage in these comminuted fractures take place near the bicipital groove, beneath the synovial and periosteal lining of this groove, so that when separation occurs, the biceps carries its sheath and the tuberosity with it. Unless this is so, it is very hard for me to account for the fact that in most cases the function of the shoulder joint returns so rapidly after fractures in this region. In the few cases in which I have had the opportunity to dissect specimens this actually was the case. (Fig. 59.) The biceps tendon would be caught between the fragments and its function destroyed if it failed to carry some of its sheath with it. At operation in badly displaced cases one often finds the tendon irrevocably injured, perhaps evulsed or caught behind the head next to the glenoid (Fig. 58), but in most cases where the fracture can be well set, the biceps somehow manages to regain its function.
Probably few surgeons consider these bursas and tendon sheaths in treating fractures in this region. It has seemed to me that the consideration of these structures has helped me personally in handling these cases. If one bears in mind the typical fracture shown in Fig. 60 and the other fractures in this region as merely incomplete forms of this typical one, he will have a feeling of understanding as he treats each individual case. Bearing in mind the four fragments which usually occur in the severe fractures, we may form subordinate types according to whether any two or three fragments remain united. Usually the four fragments are only partially separated, and either because held by periosteum and the musculo-tendinous cuff, or because prompt reduction has taken place, lie in mutually normal relations, even if as a group they are not in line with the shaft. If we could see the exact cracks in most fractures, I think we should find them more complicated than usually shown by the X-ray. In clear pictures there is much subordinate splintering of small bits of cortex. In many cases where the X-ray shows the head as one fragment, detailed study of clearly defined stereoscopic films would show the tuberosities partially separated from the head and from each other, but still held together by bits of fascia and periosteum, or by the cuff itself. The group is held together by the musculo-tendinous cuff in a jumbled mass, but still in mutual apposition, and if we can manage to cap this rather wobbly head on the top of the shaft we may obtain a good result. Usually this means disengaging the inner edge of the lower fragment from the head. The shaft is almost invariably in front of and somewhat mesad to the comminuted head.
The really important question is whether there has been escape of the articular head out of the capsule. So long as the articular head remains attached to a tuberosity, it cannot displace permanently, and so long as it remains between the tuberosities and the glenoid we may hope for a good result; but if it has escaped from the capsule there should be no delay in deciding between operation and a stiff shoulder. Social and general conditions determine this decision, and the surgeon cannot promise much, for when he operates he will find a difficult task. My belief is that the head of the bone should be replaced through a sabre-cut incision, and that the chances of a good result would be far greater if the operation were done within a few days of the injury than if it should be delayed.
We have previously mentioned various deductions from the Pivotal Paradox, but there may be another and a very important one in connection with the reduction of fractures.
Since it is probable that most fractures of the head of the humerus occur in elevation, and since in this position the long head of the biceps is relaxed, it is likely that reduction may be best accomplished by returning the arm to this position, while traction is exerted on the elbow with the forearm flexed. The forearm should then be extended while still exerting traction. Next the arm and extended forearm should be brought to the side in external rotation via the coronal plane. The forearm could then be flexed and rotated inward into the sling position if desired, for the fragments would be engaged as soon as the traction was omitted.

This maneuver would use the long head of the biceps as a guide to replacement of the fragments, since the tendon presumably still is held in its groove in both the upper fragment and in the shaft and neither fragment is capable of further outward rotation under normal circumstances. Theoretically, this maneuver, provided the long head of the biceps has remained attached to the glenoid rim, would disengage the impacted inner edge of the lower fragment and lock the fragments in proper position in most cases of epiphyseal separation, transverse fracture, and even in cases of comminuted fracture in which the tuberosities were still more or less held together by the musculo-tendinous cuff, by shreds of periosteum and by the intact base of the bursa. Even when the articular head has been displaced as in Fig. 57, it might be approximated to the shaft and tuberosities in the erect position and pushed back into the socket by the descent of the arm in the coronal plane! It is conceivable, also, that when the anatomic head has been dislocated in the axilla, it might be returned by the reverse motion.
Reference to the diagrams will give sufficient information on the minor fractures, except in two particular forms which are not generally understood.
One of these difficult types is simple impaction of the anatomic head into the tuberosity (Fig. 62b), which remains attached to the shaft. I do not mean the usual impaction of the shaft into the head. I have found that impaction of the head into the tuberosity is more disabling than some of the fractures with much wider separation of the fragments. The result of this impaction is that the length of the anatomic neck of the humerus is shortened, and the relation of the curve of the articular head is changed by rotation on the axis of the shaft. Furthermore, there is a scissor-like action on the articular edge as it obliterates the sulcus where the short rotators are attached. In other words, it cuts the attachments of the short rotators so that it leaves but a thin margin where they can secure their hold of the facets of insertion. There must necessarily be a considerable degree of traumatic tendinitis following such lesions. It is quite likely that the biceps tendon is pinched and held. Certainly from a clinical point of view, the convalescence in these cases is often delayed, and the clinical picture becomes similar to that of a severe bursitis.

Another disabling form of fracture of slight extent and probably not very common, but usually unrecognized, is depression of the greater tuberosity (Fig. 62a). It is probably due to direct violence when the arm is in dorsal flexion, but perhaps it may occur from
impact on the glenoid in elevation. I have seen at least one such case. This form of fracture is easy to overlook, and one reason for this is that the patient is usually able to use the arm for a time after he has suffered the injury. Since the tuberosity is depressed, he may even be able to elevate the arm, and as it takes some time for the formation of a callus of sufficient degree to impinge under the acromion, there is a period of fair use of the arm before serious restriction begins. Neither patient nor physician realize the extent of the injury and the Rontgenologist also may overlook it.
The following is a report which I made to an insurance company on such a case, April 11, 1929:
"The patient is a well-developed, intelligent electrician of thirty-seven. He states that he has never had any serious accident, sickness or operation except a badly cut wrist as a boy, and diphtheria when still younger. "Day before yesterday (April 9th) he fell from a ladder, and in falling struck his left shoulder on a marble slab. Although the shoulder felt sore and bruised, he continued to work, thinking that the pain would soon go away. He has continued to work since, except that he went to your clinic yesterday and was referred here by Dr. L. He has been working this morning and is able to get along because he is the boss and can have his men do the manual work. He can help with one hand. On the first night after the accident he woke with much pain, but last night there was less trouble. He can use the arm a little, but it is sore.
"Examination. This patient has good muscles and good control over them. He appears to be a very intelligent, sensible person, not inclined to exaggerate his troubles. There is a conspicuous ecchymosis to the inner side of his left arm and some deep swelling beneath it. Both correspond to the regional course which hemorrhage takes when it runs down the bicipital groove, namely, along the tendon of the biceps and then down the supracondylar areolar tissue about the internal condyle, and then into the subcutaneous tissue of the forearm. This is almost a pathognomonic sign of involvement of the base of the bicipital groove by a fracture. It perhaps may occur with rupture of the long head of the biceps.
"The motions of the joint are not much restricted, but there is some very decided restriction in abduction. There is no atrophy and only slight tenderness over the greater tuberosity. The biceps cannot be exerted without causing some pain. The X-ray supports the diagnosis of a depressed fracture of the greater tuberosity, and this accords with the clinical symptoms.
"This type of fracture is rare and apparently trivial at first sight, but in the cases I have seen it has proved in the end to be more incapacitating than fractures of the surgical neck. It goes through two stages. In the first stage the symptoms are less severe, and are caused by the mere alteration caused by the depression of the tuberosity and the hemorrhage about it. The second stage causes more incapacity, because the callus about the fragment impinges on the acromion as the arm is raised. Then, too, the trabecules, which are crushed together, dissolve, and an osteitis is set up, so that in the X-ray you get the appearance of a sequestration of the depressed fragment. At this time—perhaps three to six months from now—there is much disability and pain. Since the fragment is pressed inward, the long head of the biceps may be damaged and become adherent in the flattened, narrowed groove. Also the supraspinatus tendon is partially pinched off at the edge of the articular head.
"Naturally, there is no standard treatment for such a lesion. The usual methods of treating fractures do not apply, where there is no need of reduction or immobilization. Even if you could raise the depressed fragment, the callus would impinge even more on the acromion. It seems to me it would be better to let nature take care of it than to interfere. If I had such an accident I would work as much as I could without too much pain. "Fortunately, from what this man says, he is not obliged to do much actual work, and can hold his job without using the arm a great deal. He probably earned enough, that to be idle and lose the difference between his pay and his compensation would be a great hardship. I should think he would prefer to work as long as he can hold his job. The question, naturally, came up as to whether physiotherapy or other palliative treatment would do him any good and hasten his recovery. I do not believe any form of treatment would help him, and almost any form of treatment would harm him as much. If pain or soreness is very severe, he could try massage or diathermy, if, practically, after a few trials he found that he obtained enough relief to pay for the trouble. "He would naturally want to know whether free use of the arm would help or hinder his recovery, and on the other hand, if perfect rest would lead to shorter convalescence. I believe there might be a slight difference between complete rest and strenuous use, in favor of the former. The more he uses it the bigger the callus is likely to be, but the less he uses it, the less the change in circulation and the slower the rate of repair. I regard this as a toss-up, and if it were my arm would be guided solely by the discomfort caused by use. There are too few precedents to go by to offer any evidence of importance. I have never seen but a few cases, and do not know the exact efforts made at treatment, or the exact results. My general impression is of a slow return to normal function after not less than a year.
"A similar case which I saw for the Industrial Accident Board was incapacitated for over two years when I last heard from him, but the patient was an Italian laborer, and this man will work with soreness that would frighten an Italian. If I were in this man's place, I would stick to my job as long as I could stand it, using my arm a little, but not much. I would take no treatment and hope that the exercise of work would keep me generally fit and thus hasten my repair."
I saw the patient again on Sept. 30th, 1929. He had kept at work about three weeks before he quit, and then had baking and massage at the insurer's clinic. Rotation was free, but abduction was limited by the callus. There was atrophy of the spinati.
In November he went to work as an electrician, and worked off and on in spite of some pain for over a year. Even when I saw him last, on Dec. 3, 1930, he was still complaining of weakness and soreness in the shoulder, but at this time could do overhead work.
Fractures of the tuberosity which are not depressed sometimes also have this protracted course, and show late bursal symptoms from irregularities in the base of the bursa caused by callus, but in these cases where the fragment is at first depressed, there is an early, relatively painless stage. Fixation in any fracture of the tuberosity is likely to delay recovery rather than to hasten it.
It is remarkable in studying the literature of fractures in the upper end of the humerus to find how little detail is given to the probable relations which the muscles and bursas bear to the fragments. Few authors even mention the subacromial bursa in this connection, and many do not even mention the tendons of the short rotators. Stevens has given by far the best brief account of the mechanics of the shoulder joint that I know of. In some minor respects, I do not agree with what he has said, but as a whole, I regard his articles as very sound. I should like to quote many pages, did space permit.
Diagnosis. So far as positive diagnosis is concerned, we depend upon the X-ray. The clinical signs in the types delineated in Figs. 62a and 62b suggest those of rupture of the supraspinatus tendon, since either by partial crushing of the tissues at the time of the original injury, or by contiguity from hemorrhage about the fracture, a bursitis is started up. Later, the callus deforms the base of the bursa and makes it irregular, so that its smooth action is lost. Hence, we have the usual symptoms of bursitis, spasm, and restriction of motion preventing rotation and abduction. They are all present, but masked by the usual symptoms of fracture. There will also be localized tenderness in the same region as in cases of rupture of the tendon, and there may be, in certain stages, a jog in the scapulo-humeral motion as the callus passes under the acromion. The main clinical diagnostic point is the feeling to the examiner's finger, that the whole tuberosity is enlarged (at first by hemorrhage and later by callus). If the tuberosity is broken, an important sign often delayed for a few days, but seen within the first week, is the appearance of ecchymosis, as described in the last case history. This ecchymosis may also appear posteriorly to the deltoid in the post-axillary fold. If it is present below the lesion along the course of the biceps, one may feel fairly sure that there is a fracture near the tuberosities. I think it is present to some extent in most cases of fracture of the head of the humerus, but very frequently does not appear until after twenty-four hours from the time of the injury.
Prognosis and Treatment. One can by no means prophesy the length of the convalescence by the degree of fragmentation or displacement shown in the X-ray. Stevens is correct in his contention that it is the traumatic arthritis which needs attention more than the fractures. Traumatic arthritis, to my mind, means changes in the bursae and musculo-tendinous cuff. The probable degree of communication which exists between the joint and the subacromial bursa through the gaps between the fragments is of great importance. Perhaps some day we shall determine such points by injecting non-radiable fluids between the fragments.
As a very obvious contrast in prognosis, it may be said that if the tip of the tuberosity is torn off by the supraspinatus and withdrawn a half-inch beneath the acromion, the prognosis of the period of disability would be much greater than in a case of fracture of the surgical neck, and considerably greater than in a case of a comminuted fracture in which the articular head and tuberosities were separated, but could be reasonably well returned to their normal position. Since apparently minor fractures may lay a patient up much longer than obviously severe ones, it would be a good rule for any industrial insurer to put every case of shoulder injury in a hospital for careful study and expert opinion. A few days with the arm elevated in every case might reduce the average period of disability by many weeks.
The use of an airplane splint is not satisfactory; because there is too much danger of nerve paralysis and of ischasmia. Stevens says: "External rotation in abduction as a treatment is almost an impossibility of accomplishment unless the patient remains in bed. In bed it is the simplest method and not an uncomfortable position for the patient."
As a matter of fact, it is impracticable to treat all cases in a hospital or even in bed at home. This is more because it is not customary to place these patients in a hospital than it is because such treatment would not be wise. Minor cases often occupy hospital beds which might well be used for the early stages of the treatment of these fractures of the head of the humerus.
Stevens used a special splint to maintain the arm in external rotation and abduction. My method is simply to apply light traction to the upper arm and to allow the weight of the forearm to sag backwards (recumbent position) in external rotation, using a fillet about the wrist which permits the patient to use the forearm, but restrains him from getting it in a completely internally or externally rotated position. As I treat these cases, I visualize the bursas and try to give the patient enough active and passive motion to keep pumping blood or clot out of the bursae into the areolar tissues, where it can be rapidly absorbed, leaving the joint and bursae clean. This does not mean much motion, but a little is very much better than fixation. I would not hesitate to put the arm in elevation in a Balkan frame, or to permit the patient to move it anywhere above the level of the shoulder. I do think that it is important to keep a certain amount of pull on the humerus to prevent the biceps and triceps from driving the shaft upward on the fragments. Early stooping exercises are desirable.
Concerning the choice of cases which should be put in bed and those which may be treated in some ambulatory way, my judgment would rest largely on whether or not I thought the subacromial bursa was seriously torn, and as to whether there was enough gap between the fragments to delay union. As I have stated before, I believe that many of the fractures of the tuberosity occur beneath the base of the bursa, without involving it at all. Such cases should not be confined, but the stooping exercises with the arm relaxed should be used to make sure that adhesions in the bursa do not take place. I believe that unless there is some very unusual condition, any case of fracture of the upper end of the humerus should have fairly good motion in six weeks, and the patient should certainly be at work in six months.
There is one very striking thing about fractures of the humerus, and that is that most cases eventually recover pretty good use of their shoulders in spite of any kind of treatment. Only those in which the displacement is very great or in which the treatment is neglected very grossly (perhaps by the patient) result in ankylosis. In cases in which the reduction is imperfect, consultation should not be postponed, because early operation is far more promising than if it is delayed for even a few weeks. Surgical skill in handling fractures of the head of the humerus will be displayed more in attaining rapid and comfortable recovery than in ultimately securing good results, for nature alone would produce them in most cases. Injudicious fixation is responsible for most delays and failures in the recovery of normal function. As in all pathologic conditions of the shoulder in which function is prevented, atrophy of the spinati occurs in a few weeks and usually does not disappear for many months.
REFERENCES
PHEMISTEH, D. B., Fractures of the Greater Tuberosity of the Humerus, Ann. of Surgery, 1912, Ivi, 440-449. The above article by Phemister reviews the literature and discusses in an interesting way the methods of operation for fractures of the greater tuberosity. ROBERTS, S. M., Fractures of the Upper End of the Humerus; End Result Study, which shows Advantages of Early Active Motion. J. A. M. A. 98; 367-373. Jan. 30, 1932. This is the best article to which I can refer as to the present status of treatment of these fractures in progressive hospital clinics in America, for there is always some degree of progress that has not yet taken its place in the text books. It is a careful study of a series of cases treated at the Massachusetts General Hospital, where much attention has been devoted to fractures, during the last decade, by an active "fracture committee," so that the results may be assumed to be better than the average, even though they include a considerable number of instances where there was long delay in seeking hospital treatment. Nevertheless, it is evident that even in these carefully treated cases, the results are by no means perfect. Although appointed consulting surgeon to this hospital in 1929, I have had nothing to do with the treatment of these cases, nor have my principles of reduction, illustrated on page 324, Fig. 61, ever been tried out. The excellence of the results obtained by Dr. Roberts and his colleagues has in no way been dependent on the theories expounded in this chapter, which in many respects differ from those on which treatment was based in their cases. Are my theories sound enough to be tested? If so, by whom? At any rate, the economic loss in their series of fractures was evidently far less extravagant than would have been incurred in an equivalent number of cases of unrecognized complete ruptures of the supraspinatus.