Difference between revisions of "Surgical Treatment of Proximal Humeral Fractures"
| Line 62: | Line 62: | ||
7. Blix M. Die lange und dle spannung des muskels. Skand Arch Physiol 1891(3):295-318. | 7. Blix M. Die lange und dle spannung des muskels. Skand Arch Physiol 1891(3):295-318. | ||
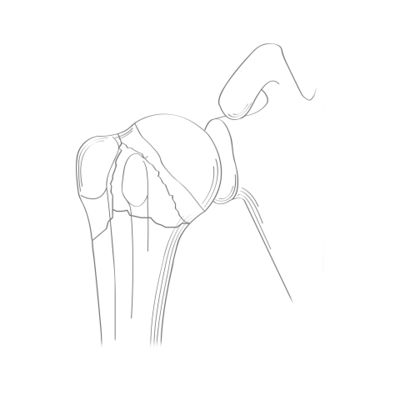
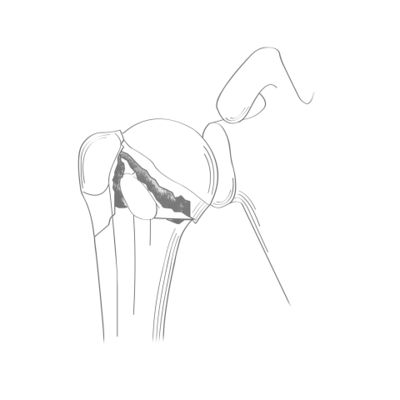
Figure: Different situations or pathological position of the greater tuberosity cause impingement and loss of strength. | Figure: Different situations or pathological position of the greater tuberosity cause impingement and loss of strength. | ||
| + | [[File:1562909015149-lg.jpg|center|thumb|600x600px|''Figure 8. A) Type II cephalotubercular valgus impacted fracture and B) displaced fracture of the greater tuberosity resulting in decreased mobility and loss of strength through relaxation of the cuff. Reproduce from Lädermann et al., with permission.'']] | ||
| − | |||
| + | The lateral offset of the greater tuberosity relative to the diaphyseal axis is another important anatomic variable, but sometimes difficult to restore due to the comminuted, and often porotic nature of fractured tuberosities, giving them an eggshell appearance. The offset is on average 18±2 mm (range, 1 to 22 mm)(Figure). | ||
| − | |||
| − | |||
8. Pearl ML, Volk AG. Coronal plane geometry of the proximal humerus relevant to prosthetic arthroplasty. J Shoulder Elbow Surg. 1996;5(4):320-6. | 8. Pearl ML, Volk AG. Coronal plane geometry of the proximal humerus relevant to prosthetic arthroplasty. J Shoulder Elbow Surg. 1996;5(4):320-6. | ||
| − | |||
| − | |||
| − | + | '''''Role of the lateral offset''''' | |
| + | [[File:1562909015961-lg.jpg|center|thumb|600x600px|''Figure 9. A) Superomedial malposition of the greater tuberosity after a subtubercular varus impacted fracture. Reproduc e from Lädermann et al., with permission.'']] | ||
| − | |||
Every effort should be made to restore this relationship intraoperatively whether by anatomic reconstruction with osteosynthesis (Figure) or during arthroplasty surgery. In the setting of chronic non-union, allograft reconstruction has also been described. | Every effort should be made to restore this relationship intraoperatively whether by anatomic reconstruction with osteosynthesis (Figure) or during arthroplasty surgery. In the setting of chronic non-union, allograft reconstruction has also been described. | ||
9. Lädermann A, Denard P, Abrassart S, Schwitzguébel A. Achilles Tendon Allograft for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity: A Case Report. Knee Surg Sports Traumatol Arthrosc. 2016;Jan 25. | 9. Lädermann A, Denard P, Abrassart S, Schwitzguébel A. Achilles Tendon Allograft for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity: A Case Report. Knee Surg Sports Traumatol Arthrosc. 2016;Jan 25. | ||
Revision as of 20:55, 7 January 2020
Written by Alexandre Lädermann
Contents
Bullet Points
- Assessment of an acute proximal humerus fracture includes a complete trauma series radiography and, where surgical treatment is considered, a CT scan with three-dimensional reconstruction.
- The decisive elements of choice between osteosynthesis and implant are essentially the patient’s age, the risk of humeral head necrosis and bone strength.
- The surgical treatment is difficult and should, in cases of osteosynthesis, lead to an anatomical result.
- According to the literature there is no difference between antegrade intramedullary nailing and plate osteosynthesis. • The reverse implant is increasingly the treatment of choice for the elderly.
- Where stability permits, early, passive mobility rehabilitation should be commenced. If this is not the case, then rehabilitation should be deferred and the patient immobilized in the meantime.
Keywords
Shoulder; proximal humerus fracture; arthroscopy; osteosynthesis; hemiarthroplasty; Intramedullary nailing; plate ; reverse implant.
Prevalence
Proximal humeral fractures are limited to those located above the insertion point of the superior edge of the pectoralis major. They represent 5% of all fractures in patients over 40 years of age.
1. Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg. 2017;26(12):2117-24.
Their incidence, having drastically increased between 1970 (87/100'000 individuals) and 1995 (304/100'000 individuals) seems, for no clear reason, to have reached a plateau since 2010 (297/100'000 individuals in 2015).
2. Kannus P, Niemi S, Sievanen H, Parkkari J. Stabilized Incidence in Proximal Humeral Fractures of Elderly Women: Nationwide Statistics From Finland in 1970-2015. J Gerontol A Biol Sci Med Sci. 2017;72(10):1390-3.
3. Sumrein BO, Huttunen TT, Launonen AP, Berg HE, Fellander-Tsai L, Mattila VM. Proximal humeral fractures in Sweden-a registry-based study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2017;28(3):901-7.
Types of Fracture and Classification
Neer’s Classification
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered
Duparc’s Classification
This classification is mainly used in France. Duparc et al. distinguished extra-articular fractures from articular fractures (Figures).
4. Duparc J. [Classification of articular fractures of the upper extremity of the humerus]. Acta Orthop Belg. 1995;61 Suppl 1:65-70.
Anatomical restitution, and especially the position of the tuberosities after fixation and during all reconstruction work, is essential. The height of the greater tuberosity in relation to the head is crucial. Normally, the tuberosity lies 8±1.2 mm (range, 6 to 10 mm) below the superior most portion of the humeral head.
5. Pearl ML, Volk AG. Coronal plane geometry of the proximal humerus relevant to prosthetic arthroplasty. J Shoulder Elbow Surg. 1996;5(4):320-6.
In non-pathologic conditions, the greater tuberosity is never above the top of the humeral head. As little as 5 mm of displacement not only creates impingement, but also insufficiency in the posterosuperior rotator cuff due to lack of tension relative to the Blix curve (Figure). Similarly, a greater tuberosity that is too low will also harm the rotator cuff.
6. Lädermann A, Denard PJ, Burkhart SS. Arthroscopic management of proximal humerus malunion with tuberoplasty and rotator cuff retensioning. Arthroscopy. 2012;28(9):1220-9.
7. Blix M. Die lange und dle spannung des muskels. Skand Arch Physiol 1891(3):295-318. Figure: Different situations or pathological position of the greater tuberosity cause impingement and loss of strength.
The lateral offset of the greater tuberosity relative to the diaphyseal axis is another important anatomic variable, but sometimes difficult to restore due to the comminuted, and often porotic nature of fractured tuberosities, giving them an eggshell appearance. The offset is on average 18±2 mm (range, 1 to 22 mm)(Figure).
8. Pearl ML, Volk AG. Coronal plane geometry of the proximal humerus relevant to prosthetic arthroplasty. J Shoulder Elbow Surg. 1996;5(4):320-6.
Role of the lateral offset
Every effort should be made to restore this relationship intraoperatively whether by anatomic reconstruction with osteosynthesis (Figure) or during arthroplasty surgery. In the setting of chronic non-union, allograft reconstruction has also been described.
9. Lädermann A, Denard P, Abrassart S, Schwitzguébel A. Achilles Tendon Allograft for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity: A Case Report. Knee Surg Sports Traumatol Arthrosc. 2016;Jan 25.
10. Vandenbussche E, Peraldi P, Naouri JF, Rougereau G, Augereau B. [Four part valgus impacted fractures of the upper extremity of humerus: ilium graft reconstruction. Apropos of 8 cases]. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(7):658-62.
11. Levy JC, Badman B. Reverse shoulder prosthesis for acute four-part fracture: tuberosity fixation using a horseshoe graft. J Orthop Trauma. 2011;25(5):318-24.
Figure: Restitution of the offset by allograft. Source: Lädermann et al.,(9) with permission.
INSERT IMAGE
Figure. 10 A) Coronal CT Scan of a right shoulder. Note the loss of bone from the greater tuberosity. B) Radiograph of the same patient after allograft reconstruction of the humeral head and reinsertion of the rotator cuff. Lastly, the head-shaft relationship must be restored. The neck-shaft angle, posterior tilt and retroversion are key factors. 12. Boileau P, Walch G. The three-dimensional geometry of the proximal humerus. Implications for surgical technique and prosthetic design. J Bone Joint Surg Br. 1997;79(5):857-65. If the above-mentioned key points are not taken into account, or left uncorrected, the sequelae could include malunions that are particularly difficult to treat. Essential points The anatomic requirements to be respected during any intervention for proximal humerus fractures are: 1. The height of the greater tuberosity relative to the proximal humeral head; 2. The lateral offset of the greater tuberosity relative to the diaphyseal axis; 3. The neck-shaft angle, posterior tilt and humeral retroversion. Adjuvant procedures Acromioplasty Acromioplasty is not indicated for acute fractures, except perhaps to improve the workspace in the case of arthroscopic treatment. 13. Charbonnier C, Chague S, Kevelham B, Preissmann D, Kolo FC, Rime O, et al. ArthroPlanner: a surgical planning solution for acromioplasty. International journal of computer assisted radiology and surgery. 2018. Long head of the biceps The consequences of proximal humerus osteosynthesis are characterised by the development of rotator interval fibrosis and adhesions at the long head of the biceps. These result in reduced joint mobility which may explain the postoperative stiffness that is sometimes observed. Moreover, the tendon can become unstable and even interpose between fragments, preventing its reduction. Lastly, trauma causes tendinopathy and even lacerations that can lead to persistent pain. Therefore, it is recommended to routinely perform a tenodesis of the long head of the biceps. 14. McGahan PJ, Patel H, Dickinson E, Leasure J, Montgomery W, 3rd. The effect of biceps adhesions on glenohumeral range of motion: a cadaveric study. J Shoulder Elbow Surg. 2013;22(5):658-65. 15. Visser JD, Rietberg M. Interposition of the tendon of the long head of biceps in fracture separation of the proximal humeral epiphysis. Neth J Surg. 1980;32(1):12-5. 16. Kim JM, Jupiter JB. Traumatic laceration of the long head of the biceps brachii from a displaced surgical neck fracture of the humerus: case report. Journal of surgical orthopaedic advances. 2011;20(4):252-4. 17. Soliman OA, Koptan WM. Proximal humeral fractures treated with hemiarthroplasty: does tenodesis of the long head of the biceps improve results? Injury. 2013;44(4):461-4. 18. Tosounidis T, Hadjileontis C, Georgiadis M, Kafanas A, Kontakis G. The tendon of the long head of the biceps in complex proximal humerus fractures: a histological perspective. Injury. 2010;41(3):273-8. This is done by opening the rotator interval to explore the long head of the biceps tendon. This exposes the biceps and also provides a landmark to define the greater and lesser tuberosities for subsequent anatomic reduction. A tenotomy-tenodesis is performed with sutures joining the fibrous “roof” of the bicipital groove to the tendon. Alternatively, tenodesis may be performed lower to the pectoralis major tendon. This location facilitates visualization of the bicipital groove which can be used to assess version during the reconstruction. The intra-articular part of the tendon is then resected. The rotator interval is left open, so as to control reduction of the humeral head and tuberosity, and to limit mobility loss. Osteosynthesis Closed osteosynthesis (arthroscopy, percutaneous surgery, intramedullary nailing) should be contrasted with open procedures (transosseous suture, plate osteosynthesis). The first have two essential merits: reducing the risk of infection and avoiding the direct approach with its consequences (bone and soft tissue devascularization, postoperative adhesions). However, they only apply to extra-articular or less complex articular fractures, such as fractures of the surgical neck or type II cephalotubercular valgus impacted fractures. Several types of osteosynthesis have been used, from “osteosynthesis à minima” by osteosuture with nonabsorbable thread, to the solid screw epiphyseal plate or its derivatives. Arthroscopy The treatment of tuberosity (Figure 11) or humeral head (Figure) fractures, with or without extension to the surgical neck, is now validated. Figure: Type 2 cephalotubercular fracture treated by arthroscopic reduction INSERT IMAGE
Figure. 11 A) Anteroposterior radiograph of the left shoulder. The lesser tuberosity fracture is non-displaced as opposed to the greater tuberosity. B) Anteroposterior and C) axial radiographs, 6 weeks after arthroscopic anchor-based fixation of the greater tuberosity. The lesser tuberosity fracture was neglected and the upper limb immobilized for 1 month using a Dujarier bandage. The green arrows indicate anchor points
Figure: Arthroscopic treatment of a humeral head fracture.
INSERT IMAGE
Figure. 12 A) Anteroposterior radiograph and B) CT scan of the left shoulder, revealing a humeral head fracture. Six months after arthroscopic reduction without fixation, the Lamy frontal and lateral radiographs confirm a perfect reduction. The rotator cuff and tuberosities are intact, so secondary displacements are limited. Reproduce from Godeneche A, Freychet B, Gunst S, Daggett M, Viste A, Walch G. Arthroscopic Reduction of Acute Traumatic Posterior Glenohumeral Dislocation and Anatomic Neck Fracture Without Internal Fixation: 2-Year Follow-up. Orthop J Sports Med. 2017;5(12):2325967117745486, with permission. with permission.
Surgical technique
This technique has many advantages including being minimally invasive and having both intra-articular and subacromial reduction control. However, it is technically demanding, and not an option for all surgeons and for all fractures. As a general guideline, arthrosopic fixation of the greater tuberosity is generally possible if the thickest part of the fragment if less than 10 mm. Fractures with more distal extension can be challenging to secure laterally if anchor-based fixation is attempted. Surgery is performed with the patient’s arm in light traction and placed in a half-seated or lateral decubitus position. The posterior approach is used, except in cases of posterior dislocation of the humeral head. Other approaches (lateral, anterior, ...) are performed on demand, depending on the type of fracture. The hematoma is drained, and a suction pipe is connected directly to the trocar, allowing the joint to be filled and emptied until a satisfactory view is obtained. An intra-articular and then subacromial assessment is performed after a bursectomy. The type of fracture and its dimensions are assessed and the fractures reduced. Joint fractures do not necessarily require stabilization (concept of the egg cup). Several types of repair are recommended to obtain an anatomic reduction of the tuberosities (single point, double row or tension band).
Percutaneous Pinning or Screw Fixation
Commonly used in paediatric orthopaedics, this technique has also been performed in adults for over 50 years, particularly those with good bone quality and 2- or 3-part fractures.
19. Bohler J. [Treatment of open diaphysial fractures of the long bones]. Acta Orthop Belg. 1962;28:450-76.
It is minimally invasive and therefore decreases the risk of vascular compromise. Another advantage of this technique is that it can be converted, at any time, if adequate reduction or stability cannot be obtained. Fractures are primarily stabilized with ascending fasciculated pins, using at least three diverging ‘palm tree’ pins in the epiphysis (Hacketal, Kapandji). Superior to inferior pins may also be used for greater tuberosity stabilization.
The percutaneous approach, however, has been difficult to establish as a reference technique due to its many disadvantages. Firstly, it is contraindicated for type 2 to 4 articular fractures, with low bone density and significant comminution, all conditions often found elderly patients. Secondly, the variable mechanical quality of the synthesis obtained can lead to long periods of postoperative immobilization and therefore stiffness. Moreover, the reduction technique and pin placement are very demanding. Lastly, many complications such as migration or joint penetration by pins, as well as potential neurological lesions have been reported.
20. Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011;20(2 Suppl):S47-60.
21. Yoon TH, Choi CH, Choi YR, Oh JT, Chun YM. Clinical outcomes of minimally invasive open reduction and internal fixation by screw and washer for displaced greater tuberosity fracture of the humerus. J Shoulder Elbow Surg. 2018.
22. Keener JD, Parsons BO, Flatow EL, Rogers K, Williams GR, Galatz LM. Outcomes after percutaneous reduction and fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(3):330-8.
23. Kamineni S, Ankem H, Sanghavi S. Anatomical considerations for percutaneous proximal humeral fracture fixation. Injury. 2004;35(11):1133-6.
24. Rowles DJ, McGrory JE. Percutaneous pinning of the proximal part of the humerus. An anatomic study. J Bone Joint Surg Am. 2001;83-A(11):1695-9.
A special case, which immediately contraindicates osteosynthesis, is the external fixator used during polytrauma or open fractures with skin damage (Figure).
Figure: External shoulder fixator
INSERT IMAGE
Figure. 13 Illustration of an external shoulder fixator assembly
Surgical technique
The patient is placed in a beach-chair position. The arm must be free, allowing the use of fluoroscopy installed close to the patient's head. The main objective is not necessarily a perfect anatomical reduction, but to align the fragments using gentle and non-traumatic manipulation. Closed reduction and percutaneous fixation of proximal humeral fractures, with or without screws, is based on external manoeuvres using ligamentotaxis.
25. Brooks CH, Revell WJ, Heatley FW. Vascularity of the humeral head after proximal humeral fractures. An anatomical cadaver study. J Bone Joint Surg Br. 1993;75(1):132-6.
For ascending pinning, the pins must be curved at the end to allow for epiphyseal divergence. Pin insertion can be supraepitrochlear, supracondylar, median supraolecranean, or at the tip of the deltoid V. Each approach carries neurological risks related to the local anatomy or joint stiffness in the elbow.
For direct pinning, if the reduction proves to be insufficient, a short superoexternal incision is made under fluoroscopic control at the lateral edge of the acromion. A deltoid split is performed, without detachment from the acromion. A spatula or Rochet punch pressed against the epiphysio-metaphyseal hinge enables careful removal of the humeral head (Figure).
INSERT IMAGE
Figure. 14 A spatula is used to elevate the humeral head This surgical action often results in a spontaneous reduction of the tuberosities. Repositioning may also be facilitated by a bone hook placed in the subacromial space holding the greater tuberosity, while the arm is rotated externally. At this stage, the primary stability of the assembly is completed by pinning between the diaphysis and humeral head and between the tuberosity(s) and humeral head. Cannulated screws of 4.0mm or 4.5mm diameter with washers can then be inserted. Alternatively, threaded pins (which reduce the risk of recession compared to smooth pins) are cut, bent and left subcutaneously (Figure). INSERT IMAGE
Figure. 15 Diagram showing the final pin assembly. With permission from Pierre Hoffmeyer. Percutaneous Antegrade Intramedullary Nailing At first sight, fixation of an epiphysis by an intramedullary nail may seem heretical, but this concept has proved itself and is now validated. Because it is intramedullary, it represents biomechanically stable osteosynthesis (Figure), especially in cases of medial comminution. 26. Clavert P, Hatzidakis A, Boileau P. Anatomical and biomechanical evaluation of an intramedullary nail for fractures of proximal humerus fractures based on tuberosity fixation. Clinical biomechanics. 2016;32:108-12.
INSERT IMAGE
Figure. 16 A) Diagram of intramedullary nailing. With permission from Pierre Hoffmeyer. Preoperative (B) and postoperative (C) anteroposterior radiographs of the intramedullary nailing of a type II cephalotubercular valgus impacted fracture.
The latest nails now benefit from anteroposterior locks, which enable improved tuberosity reconstruction. It seems that adding an unlocked calcar screw in the context of an intramedullary nail does not improve biomechanical properties.
27. Katthagen JC, Schwarze M, Bauer L, Meyer-Kobbe J, Voigt C, Hurschler C, et al. Is there any advantage in placing an additional calcar screw in locked nailing of proximal humeral fractures? Orthopaedics & traumatology, surgery & research : OTSR. 2015;101(4):431-5.
For certain bifocal cephalotubercular and diaphyseal fractures, nailing is the treatment of choice (Figure).
INSERT IMAGE
Figure. 17 Anteroposterior (A) and Lamy incidence (B) radiographs of a large notch posterior dislocation fracture (C) associated with an oblique diaphyseal fracture. Intraoperative view (D) of a femoral allograft fixed with two 3.5mm malleolar screws and fixation of the lesser tuberosity with an anteroposterior 4.5mm screw. Postoperative radiograph of the end result after intramedullary nailing (E).
The usual indications are subtubercular fractures, with or without a tuberosity shear, and type II cephalotubercular valgus impacted fractures. There are problems related to percutaneous intramedullary nailing. It requires multiple muscular and tendinous perforations (deltoid, rotator cuff) and potentially dangerous excisions. It also rules out simple adjuvant procedures, such as bone grafting, long head of the biceps surgery and cerclage of the tuberosities.
Surgical technique
This is a procedure performed under fluoroscopic guidance, in the beach-chair position. The incision is anterior or posterior (Neviaser's portal) at the acromioclavicular interval for valgus or varus misaligned fractures respectively. The nail must be inserted medially so as to pierce the head in a vascularized muscular, and not tendinous, area. It must therefore pierce the humeral head in the cartilaginous area and not at the tuberosity. Distal locking (diaphyseal) is performed first, which enables compression of the fracture site by retrograde impaction using a weight. Compression is maintained by two or three proximal screws locked into the nail.
Osteosuture
Osteosuture includes open reduction and wire fixation. Strapping of the tuberosity is often sufficient to support the humeral head. Various adjuvant techniques having the same rationale can be applied: transosseous fixation, wires emanating from anchor point(s) or fixed on a diaphyseal screw as an external brace (Figure). This is a technically simple and rapid treatment. It is ideal for isolated and displaced tuberosity fractures and may also be used for type II cephalotubercular fractures.
28. Hawkins RJ, Kiefer GN. Internal fixation techniques for proximal humeral fractures. Clin Orthop Relat Res. 1987(223):77-85.
INSERT IMAGE
Figure. 18 A) Anteroposterior radiograph of a type II cephalotubercular fracture. B) Passage of threads through the various rotator cuff tendons. The wires are then folded over a diaphyseal screw to make a Hawkins tension band (C and D).(34) Lamy radiographs. Frontal and lateral views (E and F). Operative technique The patient is placed in a half-seated position. A 4-5 cm deltopectoral or transdeltoid approach is used, depending on the type of fracture (lesser or greater tuberosity). The fracture is located after a bursectomy. The rotator cuff is repaired using an anchor or transosseous sutures. Plate osteosynthesis Modern proximal humerus plating employs locking plates which have improved the biomechanical properties of fixation compared to traditional compression plates. This is particularly important for achieving fixation in the humeral head, where fixation must be unicortical. The angulation of the solid screws can be fixed or variable and various mechanisms are used for locking the screw in the plate (i.e. locking in its housing by a threaded lock nut, or threads in the screw head which lock into the plate). The plate permits 1) anatomic reduction, 2) surgery on the long head of the biceps, 3) transplant options (humeral head, or Bilboquet in cases of osteoporosis), and 4) a firm assembly stabilized by locked screws (i.e. not free anteroposterior screws) for the treatment of tuberosities and the humeral head in cases of ‘head split’ (Figure), and lastly, tension-band suturing of the rotator cuff/tuberosities to the plate. It is therefore preferred for type II to IV complex cephalotubercular fractures where osteosynthesis has been opted for.
INSERT IMAGE
Figure. 19 Frontal (A), Lamy lateral (B) and axial (C) radiographs, 6 weeks after a type II right-sided cephalotubercular ‘head split’ fracture. Note the two anteroposterior malleolar screws that permit compression of the head fracture, while the plate stabilizes the lesser tuberosity fracture. Initially, a high rate of humeral head perforation was reported with locking plate fixation. However, this was likely to due to lack of recognition (inadequate fluoroscopy) and the misconception that all screws must be long. The only locking screws that must be long are the lower calcar screws in cases of medial comminution (Figure). The upper screws must be short (maximum 35 mm) and serve only to stabilize the greater tuberosity.
INSERT IMAGE
Figure. 20 A) Anteroposterior fluoroscopic image taken after locked plate osteosynthesis of a left-sided type II cephalotubercular fracture. Observe the short upper screws, the two lower long calcar screws, and the oblique lower screw supported on good quality distal diaphyseal bone, thereby reducing the size of required incision (6.5 cm). Surgical technique Deltopectoral approach The deltopectoral approach is the most commonly used. It enables osteosynthesis in the vast majority of fractures. A small centimetric posterior approach may also be associated in cases of humeral head dislocation (Figure). In fact, the bicipital groove can often be the starting point for a fracture of the humeral head segment confined behind the glenoid.
INSERT IMAGE
Figure. 21 Coronal (A) and axial (B) CT sections of a left-side type IV cephalotubercular fracture. In this situation, the head should not be reduced via the deltopectoral approach, but simply make a small posterior approach through which a tamp is passed (green arrow) which will push the head backwards (C). Anteroposterior and Lamy lateral postoperative radiographs (D and E, respectively).
The biceps tendon is tenodesed in most cases to facilitate reduction and identify the tuberosities. The upper border of the pectoralis major tendon can serve as a site of tenodesis. The subscapularis, supraspinatus, and infraspinatus are tagged with nonabsorbable sutures. These sutures are then subsequently passed through holes in the plate and to provide a tension-band construct. Such fixation often provides the best fixation of the tuberosities since the tendinous structures are often stronger than osteoporotic bone. The deltopectoral approach provides only a limited view of the greater tuberosity, which can be improved by putting the arm in abduction and internal rotation after placement of a Brown retractor.
The intertubercular fracture line is situated 8 mm lateral to the bicipital groove. At this stage, devascularization of the bone fragments should be avoided by conserving the anterior circumflex and ascending bicipital arteries. The idea is to stay lateral to the bicipital groove. The approach to the humeral head fragment is intertubercular by widening the separation of the two tuberosities. Reduction is performed using a 2.5 mm pin (Figure).
INSERT IMAGE
Figure. 22 A 2.5 mm Kirchner pin is inserted into the humeral head and used as a ‘joystick’ to manipulate the head fragment. With permission from Pierre Hoffmeyer. Distally, the anterior insertion of the deltoid is elevated using a periosteal elevator and the plate is slipped-in subperiosteally. The plate is temporarily secured with one cortical screw and then the height is adjusted as needed to ensure the that the inferior locking screws are at the medial calcar. In order to limit the length of the incision the distal screw is inserted obliquely. The sutures from the rotator cuff tendon may need to be passed through the plate prior to securing to the diaphysis depending on the plate design (Figure).
INSERT IMAGE
Figure. 23 Osteosynthesis of a type II cephalotubercular fracture. Four sutures have been passed through the rotator cuff tendon (A). The sutures are then passed through the plate before fixation. Once osteosynthesis is completed, the next step is to tension the sutures, thereby reinforcing the assembly (B). Transdeltoid approach A so-called mini-invasive transdeltoid variant is an option. The patient is placed in a half-seated position. A 4-5 cm approach is used in line with the acromion. The axillary nerve is isolated and the plate is then slipped between the cortex and the nerve (Figure). However, the authors of this article have stopped performing this approach because we have observed a higher rate of postoperative stiffness with this approach. Furthermore, implant removal for or conversion to arthroplasty (either at the initial surgery or for failure of fixation) is more easily performed through a deltopectoral approach.
INSERT IMAGE
Figure. 24 A) Locating the axillary nerve. B) Reduction of the fracture, support by pins and introduction of the plate. C-E) Fluoroscopic images and final result (F).
Hemiarthroplasty
The simple humeral implant is a remedy in cases of technically impossible osteosynthesis or fractures posing a risk of significant necrosis in young patients. It is restricted to cephalotubercular fractures of types III to IV in young patients. Reconstruction requires restoration of the humeral length, correct implant retroversion, restoration of the epiphyseal width, stable implant fixation, and a robust osteosynthesis of the tuberosities.
Functional results vary depending on the patient’s age, and especially the anatomical consolidation of the tuberosities. They can be excellent when it comes to mobility and pain. But, if the tuberosities are not consolidated then mobility results are poor, with an average anterior elevation of 90°. They do, however, remain acceptable for pain.
29. Boileau P, Winter M, Cikes A, Han Y, Carles M, Walch G, et al. Can surgeons predict what makes a good hemiarthroplasty for fracture? J Shoulder Elbow Surg. 2013;22(11):1495-506.
Surgical technique
The approach is most commonly deltopectoral. The joint is accessed by working through the fracture fragments in the setting of a 4-part fracture, or dividing the lesser and greater tuberosities in the setting of a 3-part fracture. The humeral head fragment is extracted. As with plate fixation, the rotator cuff is tagged with multiple sutures for subsequent fixation of the tuberosities.
30. Collin P, Laubster E, Denard PJ, Akue FA, Lädermann A. The Nice knot as an improvement on current knot options: A mechanical analysis. Orthopaedics & traumatology, surgery & research : OTSR. 2016;102(3):293-6.
Correct positioning of the implant and the tuberosities is an essential step, which will determine the quality of the functional result (cf above). The lateral offset is restored either by introducing a graft between the implant and the greater tuberosity if the implant does not fill the space, or by using a wide metaphyseal implant with no graft.
31. White JJ, Soothill JR, Morgan M, Clark DI, Espag MP, Tambe AA. Outcomes for a large metaphyseal volume hemiarthroplasty in complex fractures of the proximal humerus. J Shoulder Elbow Surg. 2017;26(3):478-83.
Height can be assessed fluoroscopically by restoring a Gothic arch appearance or by locating the insertion point of the pectoralis major.
32. Krishnan SG, Bennion PW, Reineck JR, Burkhead WZ. Hemiarthroplasty for proximal humeral fracture: restoration of the Gothic arch. Orthop Clin North Am. 2008;39(4):441-50.
33. Kim BS, Kim DH, Song KS, Min BW, Bae KC, Cho CH. Is the pectoralis major tendon a reliable reference for restoration of humeral length with fracture hemiarthroplasty? J Shoulder Elbow Surg. 2018;27(2):e45-e9.
In fact, the distance separating the upper edge of this tendon from the great tendon at the top of the humeral head is relatively constant (5.5 cm). With regard to the rotation of the implant, 20-30° retroversion (measured from a flexed elbow relative to the forearm) is normally recommended. This is 10° less than the anatomical retroversion, measured on the bi-epicondylar axis, taking into account the physiological valgus. Before implanting the final stem, a number 2.0 drill-hole is made at the metaphyseal level, through which two non-absorbable sutures are threaded to be used for fixation of the tuberosities in the vertical plane.
The stems may be cemented or non-cemented. The cement mantle should not reach the tuberositis which could jeopardise their integration.
34. Singh A, Padilla M, Nyberg EM, Chocas M, Anakwenze O, Mirzayan R, et al. Cement technique correlates with tuberosity healing in hemiarthroplasty for proximal humeral fracture. J Shoulder Elbow Surg. 2017;26(3):437-42.
A “black and tan” technique is an effective method for ensuring this. The implant is reduced and the tuberosities are stabilized using Boileau’s technique.
35. Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011;20(2 Suppl):S47-60.
Reverse Shoulder Arthroplasty
In patients aged over 65, reverse implants are now more frequently performed than osteosynthesis and hemiarthroplasty. A systematic review of level I and II studies shows that reverse shoulder arthroplasty (RSA) grants better outcomes and is associated with fewer complications than hemiarthroplasty at short term follow-up.
36. Lädermann, A. Chiu, JC. Collin, P. Piotton, S. Nover, L. Scheibel, M. Hemi- vs reverse shoulder arthroplasty for acute proximal humeral fractures: a systematic review of level I and II studies. Obere Extremität. 2019
Effectively, for these elderly patients, with comorbidities and osteoporosis, hemiarthroplasty failure is a significant risk. While reverse shoulder arthroplasty does not rely as much on tuberosity healing, function proves to be higher when the tuberosities heal. Therefore, the tuberositis should be preserved and every effort should be made to achieve healing in the setting of reverse shoulder arthroplasty. Reverse shoulder arthroplasty is contraindicated in young and active patients, apart from exceptional lifesaving situations, and in cases of infection or when the axillary nerve is involved. In fact, except for partial mobility recovery, the complication rate remains high.
37. Ek ET, Neukom L, Catanzaro S, Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22(9):1199-208.
Surgical (Operative) Technique
Apart from time spent on the glenoid, implantation is in all respects similar to hemiarthroplasty. Exposure of the glenoid is easy given the absence of the proximal humerus. The glenoid cartilage is then removed using a curette and carefully milled by hand, given the absence of osteoarthritis. The glenoid baseplate should be placed so that the glenosphere is flush or slightly overhangs the lower edge of the glenoid (Figure 25) to avoid frictional impingements.
38. Lädermann A, Gueorguiev B, Charbonnier C, Stimec BV, Fasel JH, Zderic I, et al. Scapular Notching on Kinematic Simulated Range of Motion After Reverse Shoulder Arthroplasty Is Not the Result of Impingement in Adduction. Medicine (Baltimore). 2015;94(38):e1615.
One must be cognizant of the relationship between the baseplate and the selected glenosphere size. For instance, a 42 mm glenosphere will overlap a 25 mm baseplate by 8.5mm, whereas a 36 mm glenosphere will only overlap the baseplate by 5.5 mm. Thus, baseplate position may vary depending on baseplate diameter and glenosphere size. The glenosphere should preferably be neutral or only minimally lateralized. In our experience lateralized and inferior eccentric glenospheres are associated with lower rates of tuberosity healing (Unpublished data). The implant is then reduced and the tuberosities reinserted according to the technique described by Boileau et al. Higher rates of tuberosity healing have been reported with 135 degreesstems as opposed to 155 degrees stems, but no study has directly compared these to date.
INSERT IMAGE
Figure. 25 Frontal, axial and lateral Lamy radiographs after a reverse total shoulder implant. Note the lower positioning of the glenoid baseplate, the satisfactory reconstruction of the tuberosities, and the absence of cement at the autograft level. Rehabilitation Rehabilitation (or the absence thereof) after a proximal humerus fracture is crucial, and partly conditions the outcome. After surgery everything conspires to create a stiff shoulder: the patient’s fear, pain, hemarthrosis and periarticular hematoma, muscle contusion, capsular tear, bicipital tendinopathy, etc.. Ideally, the shoulder should be rehabilitated as soon as possible, depending on the stability of the osteosynthesis. Once mobility has been regained, we never recommend reinforcement, but rather a gradual and reasonable resumption of activity. 39. Charbonnier C, Lädermann A, Kevelham B, Chague S, Hoffmeyer P, Holzer N. Shoulder strengthening exercises adapted to specific shoulder pathologies can be selected using new simulation techniques: a pilot study. International journal of computer assisted radiology and surgery. 2017. In general, the hand, wrist and elbow should be actively mobilized as soon as possible. Stable Osteosynthesis These are fixations obtained using antegrade intramedullary nailing or plates. Assisted active mobilization can be immediate. No immobilization is recommended. Physiotherapy is only intra-hospital the day after surgery to teach a rehabilitation protocol. 40. Liotard J. Painful shoulder rehabilitation: How to do it simple. Revue du rhumatisme monographies. 2010;77(3):239-45. Osteosynthesis with Relative Stability This type of rehabilitation applies to osteosuture and screwing of the tuberosities. Early and aggressive rehabilitation can in fact be harmful by provoking secondary displacement. The patient is immobilized using a sling elbow at the side or neutral abduction-rotation pillow, depending on the tuberosities involved (lesser and greater, respectively). Passive mobilization is recommended, as short pendulum exercises repeated at least 5 times a day, elevation by self mobilization in the supine position, elbow stretched, with slow, highest possible elevations, and rotations with elbows bent at 90°, using a baton held in both hands, but only mobilized by the healthy upper limb. 41. Denard PJ, Lädermann A, Burkhart SS. Prevention and management of stiffness after arthroscopic rotator cuff repair: systematic review and implications for rotator cuff healing. Arthroscopy. 2011;27(6):842-8. ‘Dry’ physiotherapy or balneotherapy may be prescribed. It includes progress monitoring and correct performance of the exercises, patient motivation, relaxing massages of the scapular belt and passive mobilization exercises. Non-stable osteosynthesis and implants Fasciculated retrograde nailing, insertion, partial fixation and implants are usually immobilized for 1 month to allow consolidation of the fragments. Physiotherapy is deferred until later. Decision Making Successful treatment depends on not only technical but also decision-making capabilities. Evidence confirming the best treatment for these fractures is lacking. However, it has recently been shown that the therapeutic consensus is directly correlated to the success of the surgery. 42. Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. The Cochrane database of systematic reviews. 2015(11):CD000434. 43. LaMartina J, 2nd, Christmas KN, Simon P, Streit JJ, Allert JW, Clark J, et al. Difficulty in decision making in the treatment of displaced proximal humerus fractures: the effect of uncertainty on surgical outcomes. J Shoulder Elbow Surg. 2018;27(3):470-7. Humeral head fractures It is difficult to codify the treatment of such a rare fracture. The following guidelines, though not based on experience, have the merit of common sense. In the elderly, the risk of humeral head necrosis immediately invokes reverse shoulder arthroplasty. In young patients, simple reduction, with or without associated osteosynthesis using screws or pins, seems valid. 44. Godeneche A, Freychet B, Gunst S, Daggett M, Viste A, Walch G. Arthroscopic Reduction of Acute Traumatic Posterior Glenohumeral Dislocation and Anatomic Neck Fracture Without Internal Fixation: 2-Year Follow-up. Orthop J Sports Med. 2017;5(12):2325967117745486. Displaced tuberosity fractures with a stable epiphyseal-diaphyseal union If the fragment is small and considered to be a type A1 bony rotator cuff lesion then arthroscopic reinsertion or open osteosuture give similar results. A large and solid fragment lends itself to screwing and nailing, while osteosuture will be preferred in cases of porous and split bone. 45. Liao W, Zhang H, Li Z, Li J. Is Arthroscopic Technique Superior to Open Reduction Internal Fixation in the Treatment of Isolated Displaced Greater Tuberosity Fractures? Clin Orthop Relat Res. 2016;474(5):1269-79. 46. Lädermann A, Burkhart SS, Hoffmeyer P, Neyton L, Collin P, Yates E, et al. Classification of full-thickness rotator cuff lesions: a review. EFORT Open Rev. 2016;1(12):420-30. Type II-IV cephalotubercular and bicipital fractures in the young It seems acceptable to restore anatomy in young or biologically healthy patients. Epiphyseal plate osteosynthesis and antegrade nailing give similar results. The first is preferred in cases where the medial hinge is preserved. Hemiarthroplasty is justified when there is a high risk of humeral head necrosis. 47. Gadea F, Favard L, Boileau P, Cuny C, d'Ollone T, Saragaglia D, et al. Fixation of 4-part fractures of the proximal humerus: Can we identify radiological criteria that support locking plates or IM nailing? Comparative, retrospective study of 107 cases. Orthopaedics & traumatology, surgery & research : OTSR. 2016;102(8):963-70. Type II-IV cephalotubercular and bicipital groove fractures in the elderly It seems reasonable to immediately resort to reverse shoulder arthroplasty in elderly patients having many comorbidities and lesser functional needs. A reverse implant seems all the more indicated when the displacement is large. The best treatment is osteosynthesis, then any conservative treatment, and lastly hemiarthroplasty. Osteosynthesis is the option having the most frequent revisions according to a recent meta-analysis. 48. Du S, Ye J, Chen H, Li X, Lin Q. Interventions for Treating 3- or 4-part proximal humeral fractures in elderly patient: A network meta-analysis of randomized controlled trials. Int J Surg. 2017;48:240-6. 49. van der Merwe M, Boyle MJ, Frampton CMA, Ball CM. Reverse shoulder arthroplasty compared with hemiarthroplasty in the treatment of acute proximal humeral fractures. J Shoulder Elbow Surg. 2017;26(9):1539-45. Isolated sub-tubercular fractures Closed nailing or plate osteosynthesis are coeval. Plates are preferred in young patients to conserve their rotator cuff and facilitate their removal, and nails are used on older patients for whom removal of material is debatable. Fasciculated nailing are reserve for paediatric cases as it has not been proven in adults in comparative studies. 50. Lee W, Park JY, Chun YM. Operative Treatment of 2-Part Surgical Neck Fracture of the Humerus: Intramedullary Nail Versus Locking Compression Plate With Technical Consideration. J Orthop Trauma. 2017;31(9):e270-e4. 51. Milin L, Sirveaux F, Eloy F, Mainard D, Mole D, Coudane H. Comparison of modified Hackethal bundle nailing versus anterograde nailing for fixation of surgical neck fractures of the humerus: retrospective study of 105 cases. Orthopaedics & traumatology, surgery & research : OTSR. 2014;100(3):265-70.