Difference between revisions of "Acute or Recurrent Anteroinferior Glenohumeral Instability"
| Line 362: | Line 362: | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| − | ![[File:1562549774884-lg.jpg|center|thumb|412x412px]] | + | ![[File:1562549774884-lg.jpg|center|thumb|412x412px]]A |
| − | ![[File:1562549775216-lg.jpg|center|thumb|300x300px]] | + | ![[File:1562549775216-lg.jpg|center|thumb|300x300px]]B |
| − | ![[File:1562549777852-lg.jpg|center|thumb|376x376px]] | + | ![[File:1562549777852-lg.jpg|center|thumb|376x376px]]C |
|} | |} | ||
| − | <br /> | + | ''Figure. 28 Illustration of the three effects A) the sling effect, B) the bony effect and C) the retensioning of the capsule. Courtesy of Gilles Walch.''<br /> |
==References== | ==References== | ||
<references /> | <references /> | ||
Revision as of 20:38, 3 January 2020
Contents
- 1 Bullet points
- 2 Key words
- 3 History
- 4 Anecdote
- 5 Anatomical Considerations
- 6 Prevalence
- 7 Pathoanatomy and biomechanics
- 8 Natural History and Risk Factors of Dislocation or Recurrences
- 9 Natural History
- 10 Classification
- 11 Clinical Presentation and Essential Physical Examination
- 12 Apprehension
- 13 Scores
- 14 Essential Radiology
- 15 Treatments
- 15.1 Methods of Reduction
- 15.2 Conservative (Nonoperative) Treatment
- 15.3 Treatment of Acute First Traumatic Dislocations
- 15.4 Surgical (Operative) Treatment
- 16 References
Bullet points
- One of most common shoulder injuries, 1.7% annual rate in general population.
- High recurrence rate that correlates with age at dislocation, up to 80-90% in teenagers (90% chance for recurrence in age <20).
- Osseous lesions, either humeral or glenoid, are identified in 95.0%. The risk of failure of arthroscopic treatment is higher if not addressed. A glenoid bony defect of >20-25% is considered "critical" and is biomechanically highly unstable and require bony procedure to restore bone loss (Latarjet, Bristow, other sources of autograft or allograft).
- A Malgaigne (Hill Sachs) defect is a chondral impaction injury in the posterosuperior humeral head secondary to contact with the glenoid rim. It is present in 80% of traumatic dislocations and 25% of traumatic subluxations.
- Axillary nerve injury is most often a transient neurapraxia of the axillary nerve and is present in up to 5% of patients.
- Incidence of associated rotator cuff tears increase with age of 40 (30% at 40, 80% at 60).
- Static glenohumeral stabilizers are the bone, the ligaments, the capsule, the labrum, and the negative pressure. The dynamic ones are the rotator cuff and long head of biceps tendon.
- The labrum contributes to 50% of additional glenoid depth.
- Anterior static shoulder stability with arm in 90 degrees of abduction and external rotation is provided by the anterior band of inferior glenohumeral ligament (main restraint).
- The middle glenohumeral ligament provides static restraint with arm in 45° of abduction and external rotation.
- The superior glenohumeral ligament provides static restraint with arm at the side.
- The physical examination demonstrates instability if the apprehension test is positive, multidirectional hyperlaxity when the external rotation at side is equal or above 85 degrees, and a pathological laxity of the inferior glenohumeral ligament if the hyperabduction test is positive.
- Three views plain radiographs, including true anteroposterior of the glenohumeral joint, scapular Y (scapular lateral), and Velpeau axillary views are the mainstay of imaging in the setting of acute traumatic anterior instability. Plain radiographs including anteroposterior in neutral, internal and external rotations, scapular Y and Bernageau views are obtained for recurrent instability. Magnetic resonance imaging (MRI) arthrogram is useful to assess for labral or rotator cuff tears, computed tomography (CT) for bone loss assessment.
- Conservative treatment after the first traumatic anterior dislocation is recommended for patients who are not actively engaged in sports, above the age of 30 years old, with a low functional demand, with an associated humeral fracture, or for the athlete with an in-season shoulder dislocation.
- Rehabilitation consist of strengthening of dynamic stabilizers (rotator cuff and periscapular musculature), exercises for proprioception and other specific treatments if apprehension persist.
- Surgical treatment included Bankart repair, capsular plication +/- soft tissue procedures (such as remplissage or dynamic anterior stabilization (DAS) if < 20% bone loss.
- If bone loss ≥ 20%, bone reconstruction with Latarjet, Bristow or free bone block transfers such as Eden-Hybinette is recommended.
Key words
Anterior glenohumeral instability; shoulder dislocation; subluxation; reduction; bone loss; Malgaigne; Hill-Sachs; Bankart; capsular shift; remplissage; dynamic anterior stabilization (DAS); Latarjet; Bristow; free bone block transfer; Eden-Hybinette; complication; recurrence; pull-out.
History
The first recorded depictions of shoulder reduction are ancient.[1]
Egyptian hieroglyphs dated 3000 years earlier, pictorially depict a leverage method of shoulder manipulation, They have been followed by the Greeks and Romans. Around 400 BC, Hippocrates, the father of Western medicine, introduced the traction method to reduce the shoulder. [2][3][4]
In 1855, Malgaigne was the first one to describe the humeral bone loss also called Hill-Sachs lesion.[5]
In the 1890s, the understanding of the unstable shoulder was elucidated by the work of two French researchers, Broca and Hartman who introduced the concept of capsulolabral damage following dislocations as possible cause of recurrent instability. Notably, most of the findings considered current hallmarks of shoulder instability, including Bankart lesion, bony Bankart, Kim lesion, as well as anterior and posterior labral periosteal sleeve avulsions and glenoid avulsions of glenohumeral ligaments, were described in their papers, decades before the eponymous figures to whom they are now commonly assigned depicted them.[6]
In 1906, Perthes in Germany and a few years later, Bankart in the UK ascertained that the detachment of the labrum caused instability of the shoulder and emphasized reattachment of the labrum to stabilize the joint.[7][8]
Current free bone grafting techniques are based on the initial descriptions by Eden in 1918 and Hybinette in 1932 using autologous iliac crest.[9][10]
Due to donor site morbidity with autologous iliac crest bone grafting techniques, different auto- and allogeneic bone materials have been evaluated as alternatives. Open and arthroscopic approaches using distal clavicle, femoral head, distal tibial allografts or coracoid process are currently used. The first coracoid process transplant was probably realized by the German surgeon Noeske in 1921.[11]
Nowadays, two most popular bony procedures included the Latarjet and its variant, the Bristow.[12][13]
Anecdote
(unpublished data, courtesy of Gilles Walch) At the beginning of the 1950s, Albert Trillat, the head of the orthopedic surgical clinic at the Edouard Herriot Hospital in Lyon (France) and also the promoter of the "no touch technique", reported combination of an anterior labro-ligamentous complex reinsertion when feasible with a reduction of a so-called coraco-glenoid outlet by means of a coracoid osteoclasy and nail fixation (Figures).[14]
Another surgeon, Michel Latarjet, who was mainly active in the field of thoracic surgery, visited Dr. Trillat to learn the aforementioned technique. When Latarjet supposedly tried to reproduce the Trillat procedure, he carried an involuntary complete coracoid osteotomy. Thenceforth, not knowing what to do with the bony fragment, he fixed it to the anterior glenoid through the subscapularis using a screw. From this mishap was born the operation which now bears his name.[15]
Anatomical Considerations
The glenohumeral joint has six degrees of freedom with minimal bony constraint that provides a large functional range of motion. It thus renders this diarthrodial joint particularly vulnerable to instability. The glenohumeral joint is stabilized by dynamic and static structures. The dynamic stabilizers include the rotator cuff, the long head of the biceps, and the deltoid. The static stabilizers of the joint include the capsule, the glenohumeral ligaments, the labrum, negative pressure within the joint capsule, and the bony congruity of the joint. The superior glenohumeral ligament functions primarily to resist inferior translation and external rotation of the humeral head in the adducted arm. The middle glenohumeral ligament functions primarily to resist external rotation from 0 degree to 90 degrees and provides anterior stability to the moderately abducted shoulder. The inferior glenohumeral ligament is composed of two bands, anterior and posterior, and the intervening capsule. The primary function of the anterior band of the inferior glenohumeral ligament is to resist anteroinferior translation.[16]
Prevalence
The glenohumeral joint is the most commonly dislocated large joint of the body, affecting approximately 1.7% of the general population.[17]
In greater than 90% of cases, the instability is anterior, has a traumatic origin, and occurs in young athletes involved in contact sports.[18][19]
Ongoing sports participation in this population is associated with a high recurrence rate.[20]
Pathoanatomy and biomechanics
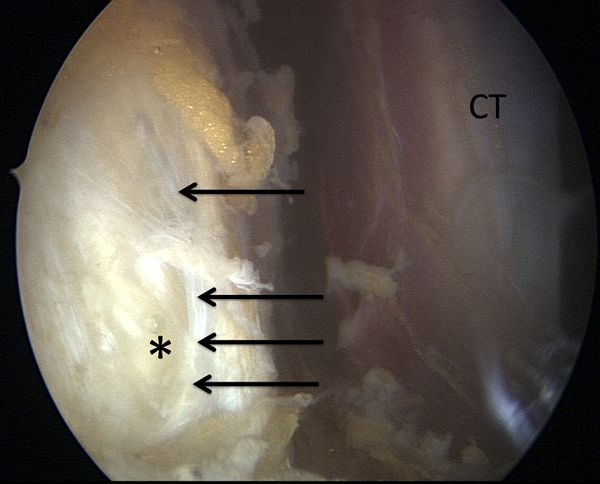
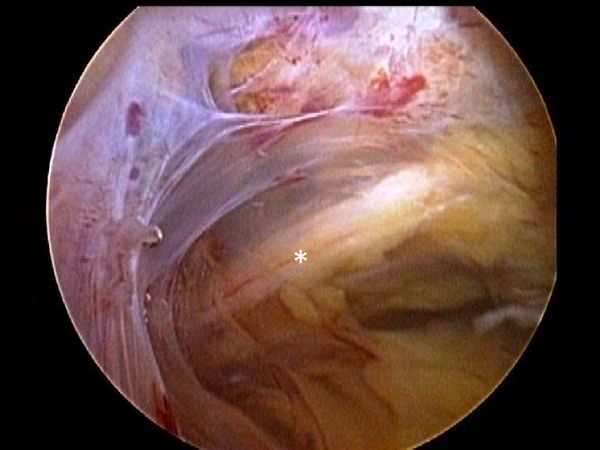
Anterior shoulder instability usually occurs with an anteriorly directed force applied to an abducted and externally rotated arm, or from a direct blow. During an anterior dislocation, many of the passive and active stabilizers may be damaged. The glenoid labrum, the glenohumeral ligaments, and the glenohumeral joint capsule, representing the soft tissue passive stabilizers will be injured; an avulsion of the anterior labrum, the classic Bankart lesion (Figure) or its variations (glenolabral articular disruption (GLAD), Perthes, anterior labroligamentous periosteal sleeve avulsion (ALPSA)) is almost invariably present,11,22,23 although it does not produce instability in isolation.[21][22][23][24]
The anteroinferior glenohumeral ligaments and the capsule can be detached from the glenoid rim, and a plastic deformation of the glenohumeral ligaments or an HAGL lesion (Figure) are other common features.[25]
The plastic deformation of these structures becomes progressively more severe with subsequent episodes.[26][27][28]
The middle glenohumeral ligament functions to limit both anterior and posterior translation of the arm at 45 degrees of abduction and 45 degrees of external rotation whereas the inferior glenohumeral ligament resists translation of the arm in greater degrees of abduction.[29]
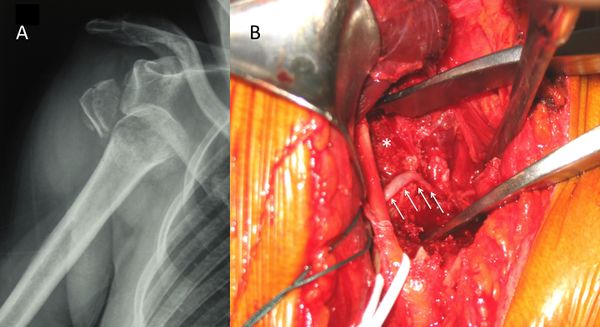
In addition to progressive soft tissue injury, recurrent dislocations can facilitate bony injury. Bony lesions are frequent in recurrent cases and may include defects of the glenoid (bony Bankart or beveling of the anterior glenoid resulting in loss of glenoid concavity), impaction of the posterolateral humeral head (Malgaigne lesion), or even coracoid or proximal humerus fractures (Figure).[30][31][32]

Given that the average glenoid diameter is about 24 mm, a 6 mm-wide or larger fragment of the glenoid will typically equate to a 25% or more of the articular surface and is considered a large bony fragment.[33][34]
Such significant glenoid bone loss can be viewed arthroscopically as an inverted pear configuration. All Malgaigne lesions are by definition engaging lesions (since it has engaged at least once). Thus, the notion of “engaging” versus “non-engaging” can lead to significant confusion. Some have proposed that the important lesions are those that engage in the 90-90 position.
Finally, the active restraint, mainly a lesion of the rotator cuff above the age of 40, will complete this complex situation.[35][36]
The glenohumeral joint is stabilized by a so-called “concavity compression” principle with the rotator cuff pulling the humeral head into the glenoid concavity and therefore ensuring stability through counteracting decentering translational forces.[37][38][39]
Natural History and Risk Factors of Dislocation or Recurrences
To understand the natural history of instability and its importance for the appropriate management of this pathology, the following questions should be answered: What happens in the shoulder after the first dislocation? Which structures suffer damage? Who are the patients at higher risk of recurrence? How does the disease evolve without treatment? Will surgical treatment avoid future negative outcomes and prevent degenerative joint disease? Who should we treat and when?[40]
80% of anterior-inferior dislocations occur in young patients. Recurrent instability is common and multiple dislocations are the rule. Instability is influenced by a large number of variables, including age of onset, activity profile, number of episodes,delay between first episode and surgical treatment. The different risks factors are:
-Young males, (up to 100% of recurrence)[41][42]
-Practice of contact sports, forced overhead activity,
-Sport practice at a competitive level,[43]
-Bony impairment,
-Concomitant hyperlaxity.[44]
Natural History
Classification
Instability can be classified as primary or recurrent. The latter can be further classified as dislocation, subluxation, apprehension, or an unstable painful shoulder. In frank dislocation, the articular surfaced of the joint are completely separated. Subluxation is defined as symptomatic translation of the humeral head on the glenoid without complete separation of the articular surfaces. Apprehension is classically defined by fear of imminent dislocation in the 90-90 position. This could correspond to an instability phenomena or a persistent fear after a successful glenohumeral stabilization (please refer to Apprehension chapter).[45]
The unstable painful shoulder presents as pain only (as opposed to a sense of instability) during an apprehension maneuver at clinical examination.[46][47]
The majority of these patients has a history of trauma, but simply do not report a clear history of trauma. Careful preoperative and/or arthroscopic examination will show that the majority of these patients also have evidence of instability (i.e. labral tear, glenoid fracture, or Malgaigne (Hill-Sachs) lesion)
Five types of traumatic anterior dislocation have been described. The subcoracoid dislocation has an antero-inferior direction and is the most common. Other types, including subglenoid, subclavicular, retroperitoneal, and intrathoracic are rare and usually associated with severe trauma.[48][49]
Osseous defects of the anterior glenoid rim can be classified into three types according to their pathomorphology. In particular, acute (type I) and chronic glenoid rim defects (type II and III) are differentiated, which are provoked either by an acute glenoid fracture or recurrent shoulder dislocations with subsequent erosion of the glenoid rim. Type I lesions are further divided into bony Bankart lesions (type Ia), solitary glenoid rim fractures (type Ib) and multifragmented glenoid rim fractures (type Ic). In most cases, type I glenoid defects can sufficiently be reconstructed by mobilization and anatomical refixation of the fragment.
In cases of complex multifragmented glenoid rim fractures (type Ic), however, it may be necessary to resect the fragments and augment the glenoid defect. Type II defects include chronic fragment-type of lesions that are characterized by an extra-anatomically consolidated or pseudarthrotic fragment of insufficient dimensions for a defect reconstruction due to resorption processes. A bony glenoid augmentation may be indicated, depending on the dimensions of the glenoid defect and the remaining fragment. Erosion-type of defects (type III) are predominantly observed in patients with recurrent anterior shoulder dislocations. These usually develop on the basis of a glenoid fracture with subsequent resorption of the fragment, or as a result of chronic abrasion of the anterior glenoid rim. If the bone loss adopts substantial dimensions, mere soft-tissue stabilization procedures are not sufficient in re-establishing stability.
Clinical Presentation and Essential Physical Examination
The history should document age, hand dominance, occupation, participation in sporting activities, initial mechanism of the injury, the position of the arm (extension, abduction, and external rotation favors anterior dislocation), how long the shoulder stays out, the method of reduction, the number of recurrences (frank dislocation vs subluxation), and the effectiveness of a previous nonoperative or operative treatment. The diagnosis of recurrent traumatic anterior glenohumeral instability is usually made easily on the basis of the history, radiographs, and a positive apprehension sign. However, when collision athletes are seen, care should be taken because they may not experience clear dislocation or subluxation and only complain of pain or weakness.
A comprehensive physical examination is essential. The aim is to define the direction of instability, the presence of an associated pathologic hyperlaxity, and to exclude neurological and rotator cuff impairment. Passive and active glenohumeral range of motion should be assessed. Rotator cuff examination includes strength tests such as belly-press, bear hug, Jobe tests and strength in external rotation again resistance (please refer to Rotator Cuff Pathology/Rotator cuff complete lesion). Tests for anterior and superior labral lesions are not systematically perform as they have a poor sensitivity and specificity.[50]
The neurovascular status of the upper extremity is assessed, particularly with regard to the axillary nerve since there is a high incidence of injury to this nerve with traumatic instability (Figure).
Laxity is a normal, physiologic and asymptomatic finding, that corresponds to translation of the humeral head in any direction to the glenoid.[51]
Laxity is assessed with the sulcus sign, anterior-posterior drawer, hyperabduction tests, and external rotation elbow at side. The two former tests are only qualitative and are not routinely performed by the authors. Hyperlaxity is constitutional, multidirectional, bilateral and asymptomatic. Hyperlaxity of the shoulder is probably best defined as external rotation elbow at the side equal or greater than 85 degrees.[52]
This non-pathological finding is a risk factor for instability but does not by itself demand treatment unless there is clear pathological laxity. Pathological laxity of the inferior glenohumeral ligament is observed when passive abduction in neutral rotation in the glenohumeral joint is above 105 degrees, there is apprehension above 90 degrees of abduction, or if a difference of more than 20 degrees between the two shoulders is noted.[53][54]
For apprehension the patient is initially invited to demonstrate his or her functional problem to the examiner (no-touch examination). This examination alone, coupled with a good history, often provides the information needed. However, if the direction of the instability remains unclear, the apprehension (crank) test, an abducted and externally rotated position suggestive of anterior instability is performed. Fear of dislocation or a feeling of anterior pain is considered positive for damage to the anterior capsulolabral complex, which should be relieved with posterior translation of the humerus (relocation maneuver). To summarize, the physical examination demonstrates instability if the apprehension test is positive, multidirectional hyperlaxity when the external rotation at side is equal or above 85 degrees, and a pathological laxity of the inferior glenohumeral ligament if the hyperabduction test is positive.
Apprehension
Apprehension can be difficult to diagnose pre- or post-operatively, as it seems more complex than a pure mechanical problem of the shoulder. Although clinical definition seems to be well established, its underlying pathologic mechanism remains unclear. This may explain the wide reported range (3% to 51%) of patients with ongoing apprehension or who will avoid any shoulder movement after an open or arthroscopic stabilization, despite a clinically stable joint.[54][55][56]
Failure to recognize and adequately address this issue may result in poor outcome and lead to unnecessary surgery or even revision. Furthermore, identifying this condition may allow establishing adequately targeted rehabilitation programs.
Definition
An important aspect to incorporate in dislocation management is apprehension, defined as anxiety and motor resistance in patients with a history of anterior glenohumeral instability. Clinically, apprehension sign is defined as fear of imminent dislocation when placing the arm in abduction and external rotation, and should be distinct from mere pain which can be related to inflammation, stiffness and other shoulder pathologies.[57][58]
Proprioception, as defined by Charles Scott Sherrington, is the sense of the relative position of neighboring parts of the body and strength of effort being employed during movement.[59]
It is distinct from exteroception, by which one perceives the outside world, and interoception, by which one perceives pain, hunger, or the movement of internal organs. The brain integrates information from proprioception and from the vestibular system into its overall sense of body position, movement, and acceleration. Kinesthesia refers either to the brain's integration of proprioceptive or vestibular inputs.
“Localization” of Apprehension
The pathogenesis of apprehension is not fully understood. Theoretically, apprehension could be related to:
1) Brain changes induced by dislocations[60][61][62][63]
2) Peripheral neuromuscular lesions consecutive to dislocation affecting proprioception[64]
3) Persistent mechanical instability consisting in micro-motion[65]
Brain
Fear, anxiety and anticipation of situations that could lead to a dislocation are essential cognitive processes in shoulder apprehension. Functional magnetic resonance imaging (fMRI) measures brain activity by detecting changes associated with blood flow.[66]
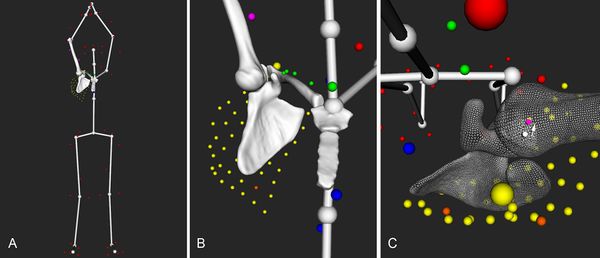
When exploring neuronal connections and cerebral changes induced by shoulder dislocation, research revealed that several cerebral areas are modified, representing the different aspects of shoulder apprehension. Specific reorganizations are found in apprehension-related functional connectivity of the primary sensory-motor areas (motor resistance), dorsolateral prefrontal cortex (cognitive control of motor behavior), and the dorsal anterior cingulate cortex/dorsomedial prefrontal cortex and anterior insula (anxiety and emotional regulation) (Figure).[67]
Those regions are involved in the cognitive control of motor behavior. Hence, there is motor control anticipation and muscular resistance (protective reflex mechanism), in order to avoid shoulder movement that could lead to dislocation.[68]
Fractional anisotropy, representing white matter integrity, is increased in the left internal capsule and partially in the thalamus in patients compared to healthy controls. Fractional anisotropy correlated positively with pain visual analog scale (VAS) scores (p < .05) and negatively with simple shoulder test (SST) scores (p < .05).[69]
This suggests an abnormal increased axonal integrity and therefore pathological structural plasticity due to the over-connection of white matter fibers in the motor pathway. These structural alterations affect several dimensions of shoulder apprehension as pain perception and performance in daily life.
Shoulder stabilization could allow the brain to partially “recover”. Patients with shoulder apprehension underwent clinical and functional magnetic resonance imaging (fMRI) examination before and one year after shoulder stabilization surgery. Clinical examination showed a significant improvement in postoperative shoulder function compared with preoperative. Coherently, results showed decreased activation in the left pre-motor cortex postoperatively, demonstrating that stabilization surgery induced improvements both at the physical and at the brain level, one year postoperatively (Figure). Most interestingly, right–frontal pole and right-occipital cortex activity is associated with good outcome in shoulder performance.[70]
Peripheral Neuromuscular Lesion
During a traumatic dislocation, there are a disruption of the shoulder tendinomuscular (in 10% of cases) and peripheral nerve lesions (in 14% of cases).[71]
However, this does not account for subclinical neurologic damage that may be much more preponderant. Capsuligamentous structures surrounding the glenohumeral joint are richly innervated with proprioceptors and therefore play an important sensorimotor role in addition to their primary mechanical stabilizising function. Thus, when considering the extensive and frequent damage to these structures after shoulder dislocation (Figure), there is bound to be an important loss in glenohumeral proprioception.[72][73]
The latter plays a significant role in stabilization of a normal healthy shoulder and after any shoulder injury by contributing to motor control.[74]
Surgical stabilization has been shown to help proper healing of these structures and thus restoring proprioception of the glenohumeral joint.[75]
Glenohumeral Joint
The third etiologic factor for apprehension is persistent micro-motion in the glenohumeral joint despite a clinically stable shoulder, satisfactory radiographic results, and no new episode of subluxation or dislocation. Shoulder dislocation causes damage to the capsuloligamentous complex in 52% of the cases, and the glenoid labrum in 73% of the cases.[76][77]
The plastic deformation of these structures becomes progressively worse with subsequent episodes.The plastic deformation of these structures becomes progressively worse with subsequent episodes. In addition to progressive soft tissue injury, recurrent dislocations induce bony lesions, which may involve the glenoid (bony Bankart), the posterolateral humeral head (Malgaine), or both. Severity of apprehension, quantified as the moment at which it appears during the course of abduction and external rotation, seems to be correlated to the extent of bone loss. Capsular redundancy has also been recognized as a risk factor for ongoing apprehension after surgical stabilization and Ropars et al. found a significantly decreased apprehension in patients with associated capsulorraphy to Latarjet procedures, compared with patients with Latarjet and no capsular reconstruction.[78]
However, these changes may be very subtle and therefore not detectable on standard clinical magnetic resonance imaging (MRI) in neutral position. This has been described by Patte et al. in non-operated patients and popularized under the name of "unstable painful shoulder".[79][80]
This micro-motion may yet still be present after surgical stabilization. Shoulder stabilization may thus only prevent new episodes of dislocation, rather than actually truly stabilizing the shoulder.[81][82]
A study described glenohumeral translation in patients with traumatic anteroinferior instability and subsequently analyzed the effect of glenohumeral stabilization on this translation. For all movements, the authors recorded humeral head position of the contralateral and ipsilateral shoulders in relation to the glenoid center pre- and 1 year post-operatively. They observed an anterior translation of the humeral head (Figure), especially during flexion and abduction movements (p < .05 and p < .05, respectively). One year after surgery, all patients had a clinically stable shoulder and none presented with a new episode of dislocation or subluxation.
However, anterior translation of the humeral head was not significantly reduced and remained close to preoperative values confirming that shoulder stabilization does not stabilize the shoulder but uniquely prevents further dislocation. These findings have several important implications. First, it may explain residual pain, apprehension, and impossibility to return to sport at the same level as reported in other studies. Second, persistent abnormal motion between the glenoid and the humeral head might be the underlying cause of dislocation arthropathy that is observed with a prevalence of 36%. Repeated sliding of the humeral head against the glenoid associated with degenerative changes of cartilage properties and decreased biological healing potential related to aging, could lead to a vicious circle of extensive cartilage damage.[83]
Scores
Rowe
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
Walch-Duplay
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
WOSI
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
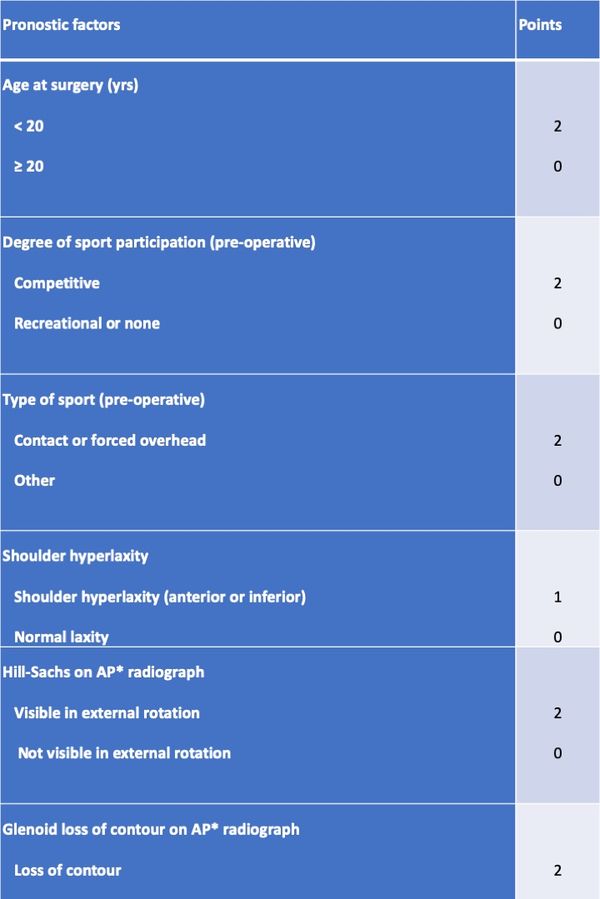
ISIS
Boileau et al. proposed a simple 10-point scale scoring system (instability severity index score (ISIS)) based on factors derived from a pre-operative questionnaire, physical examination, and anteroposterior radiographs to determine the risk of treatment failure following isolated arthroscopic Bankart repair (Table). In this model an ISIS of 3 or less was associated with a 5% rate of recurrence, a of 4 to 6 was associated with a 10% rate of recurrence, and an ISIS over 6 was associated with a 70% rate of recurrence. Although it has imperfections, this score, validated since, has merit to easily remind the clinician of factors that are important to consider when evaluating a patient.[84][85]
Table: The instability severity index score is based on a pre-operative questionnaire, clinical examination, and radiographs.
Essential Radiology
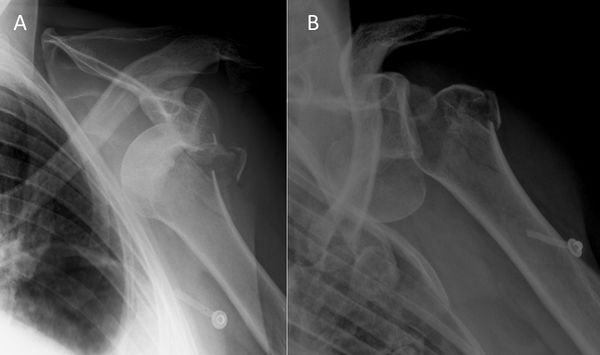
Radiographic evaluation is based on whether the dislocation is acute or chronic.
Acute Dislocation
Three views plain radiographs, including true anteroposterior of the glenohumeral joint, scapular Y (scapular lateral), and Velpeau axillary views are the mainstay of imaging in the setting of traumatic anterior instability[86]
The latter view is crucial to obtain, as the two first alone do not allowed to exclude a dislocation. The goal is to confirm the direction of dislocation and to evaluate associated lesions. One reduced, further imaging studies in the setting of an associated fracture (computed tomography (CT)), suspicion of rotator cuff injury (ultrasonography or magnetic resonance imaging (MRI)), or vascular impairment (injected CT) may be warranted.
Preoperative Planning in Case of Recurrent Dislocation
The first step is to analyze, if available, plan radiographs with the shoulder out of joint to confirm the direction of instability. Plain radiographs including anteroposterior in neutral, internal and external rotations, scapular Y and Bernageau views are then obtained.[87]
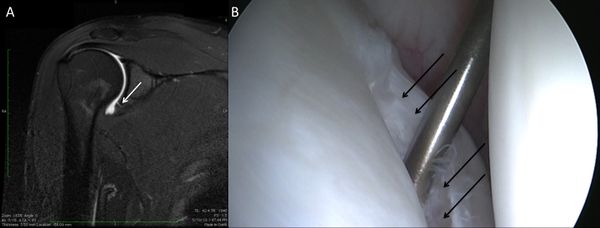
Bone loss, static instability, post-dislocation arthropathy, and coracoid non-union (if a Latarjet or a Bristow procedures are planned) have to be estimated. Magnetic resonance imaging (MRI) arthrogram is useful to assess for soft tissue such as an anterior labral tear (Figure).
Associated intra-articular pathology such as SLAP, HAGL, and rotator cuff lesions or a paralabral cyst are also assessed (Figure).
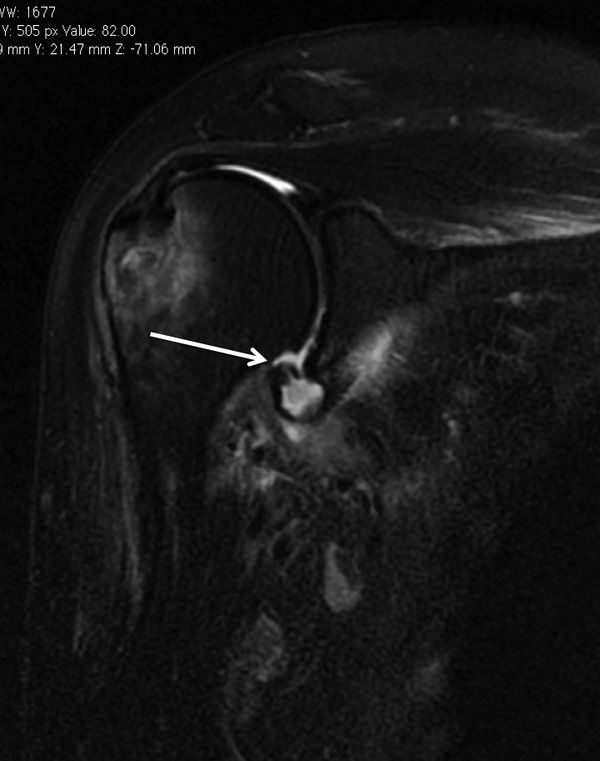
The evaluation is completed by a 3D computed tomography (CT) arthrogram in the setting of recurrent instability in which there is primary concern for bone loss. The extent of both glenoid bone loss and Hill-Sachs lesions are best assessed by computed tomography (CT) scan and are used to determine the need for a bony procedure as opposed to arthroscopic Bankart repair (Figures).

Treatments
The degree, nature and combination of injuries induced by traumatic glenohumeral instability are highly variable. Damage to the bony and soft tissue stabilizers of the shoulder, as well as neurologic impairment, must be detected and analyzed in order to provide the patient with the most adequate treatment option. This new knowledge should be applied to rehabilitation therapy and surgical stabilization techniques. As the current stabilization techniques do not seem to prevent residual glenohumeral micro-motion, it remains to be determined which factors help to minimize this phenomenon, whether it is, the increase in the anteroposterior diameter of the glenoid with a bone graft, the sling effect provided by the conjoined tendon or the long head of the biceps, the capsulorraphy, the repaired labrum or the remplissage.[88][89][90][91]
Methods of Reduction
Around 400 BC, Hippocrates, the father of Western medicine, introduced the traction method to reduce the shoulder. The patient lay supine whilst the physician standing on the patient's affected side held the arm and applied traction. The stockinged foot of the physician placed in the axilla served as counter traction. This technique was detailed in the Hippocratic Corpus, and as it remained the primary medical text for centuries so did the method. Similar technique of reduction was re-introduced in the 1870 as a painless technique by Theodor Kocher, but is now obsolete because of the likelihood of serious complications.[92]
Conservative (Nonoperative) Treatment
Heading towards a better understanding of the complex and multifactorial origins of glenohumeral instability and apprehension, postoperative management may in turn also be improved, notably in challenging cases of patients with persistent apprehension, despite a clinically stable shoulder. Knowing that shoulder apprehension could be the result of ongoing cerebral abnormalities or residual micro-motion may avoid costly series of onerous investigations, useless physiotherapy sessions or even re-operations. Furthermore, this perspective offers a new angle of a therapeutic approach that differs from conventional manual rehabilitation methods centered on the glenohumeral joint itself. If persistent apprehension or micro-motion is detected, growing research evidence supports the use of a multidisciplinary approach including:
1) A "reafferentation" (reconveying and connecting the neurological peripheral input to the cortex)89 of the shoulder particularly focused on proprioceptive work,69 which has been proved to lead to superior neuromuscular control than strengthening alone.[93][94][95]
2) A biofeedback therapy where the patient directly visualizes his abnormal response to a negative stimulus on fMRI or electroencephalogram, and can thereby actively correct it. This treatment modality has already shown to improve shoulder control and performance in various settings,[96][97][98]
3) a cognitive behavioral approach to decondition this pathological residual apprehension by making them realize residual apprehension does not necessarily lead to recurrent instability with gradual exposition that has already shown successful results in the treatment of kinesiophobia,94-96 a condition based on a re-injury fear-avoidance model initially described in low-back pain,97 further popularized in sports medicine98 and various upper limb conditions.[99]
4) Electric stimulation of hypoactive rotator cuff and periscapular muscles.[100]
Treatment of Acute First Traumatic Dislocations
The first step, whenever possible, is to obtain a complete set of radiographs before attempting a reduction. This will allow an assessment of the type of dislocation and associated bone injuries. Attempting to reduce a fracture dislocation can have troublesome clinical and legal consequences (Figure).
Exceptions are an impossibility to have reasonably fast access to radiology or a patient with neurological impairment. Because of the possible association of nerve injuries and, to a lesser extent, vascular injuries (Figure), an essential part of the physical examination is an assessment of the neurovascular status of the upper extremity before reduction.[101][102]
They are numerus appropriate methods of reduction that have been described. The second step is to use the technique of closed reduction which is mastered by the doctor who will perform the maneuver. The glenohumeral joint should be reduced as gently and expeditiously as possible. In the case of fracture dislocation, the reduction is best performed under general anesthesia to have adequate muscle relaxation. After reducing the dislocation, plain radiographs are obtained to verify the adequacy of the reduction.
Results concerning conservative treatment are still debatable. A stable shoulder is obtained at ten years in only half of patients with conservative treatment.[103]
However, recurrence rate is highly dependent on age and activity of the patient; studies have reported a 72% to 95% recurrence in patients under 20 years of age, and 70% to 82% recurrence between the ages of 20 and 30 years, and only 30% in those over 30 years of age.[104][105][106]
Many patients above the age of 30 would consequently undergo unnecessary surgery if proposed after the first dislocation. Conservative treatment after the first traumatic anterior dislocation may be thus recommended for patients who are not actively engaged in sports, above the age of 30 years old, with a low functional demand, with an associated humeral fracture, or for the athlete with an in-season shoulder dislocation. For the latter situation, athletes are allowed to attempt to return to competition provided there is enough time left in the season to permit adequate rehabilitation with progression to sport-specific drills.
Rehabilitation, including return of range of motion and strengthening of dynamic stabilizers may facilitate return to sport within several weeks. Motion-limiting braces that prevent extreme shoulder abduction, extension, and external rotation are often prescribed as it may reduce the risk of recurrence. However, such braces are not well-tolerated in patients who must complete certain overhead tasks such as throwing. Moreover, a second in-season shoulder dislocation should lead to removal from sport and proceeding with stabilization so as to avoid further glenohumeral damage.
A number of studies have compared nonoperative treatment and arthroscopic stabilization. Overall, these studies report a sevenfold reduction in the risk of recurrent instability after arthroscopic stabilization, when compared with nonoperative treatment for the first-time dislocator.[107]
A Cochrane review concluded that early surgical intervention is warranted in young adults aged less than 30 years engaged in highly demanding physical activities.[108]
Consequently, for patients who are actively engaging in a collision or contact or overhead sport, who risk their life in case a new dislocation (e.g. firemen, proponents of extreme sports like base jumping, and climbing), with associated static anterior subluxation, an interposed tissue or a nonconcentric reduction, or patients with rotator cuff avulsion, conservative measures are usually inadequate and prompt surgery is indicated.
Surgical (Operative) Treatment
Recurrent dislocation is not trivial. Each episode creates new lesions and increases the risk of developing dislocation arthropathy. The concept of early operative surgical management of the first-time dislocator has consequently been introduced to address the high recurrence rate in the young athletic population. A surgery should be proposed, as having the ultimate aim to achieve a pain-free stable shoulder while preserving range of motion. The surgical approach is based on the extent of bone loss and patient-specific risk factors for recurrence.
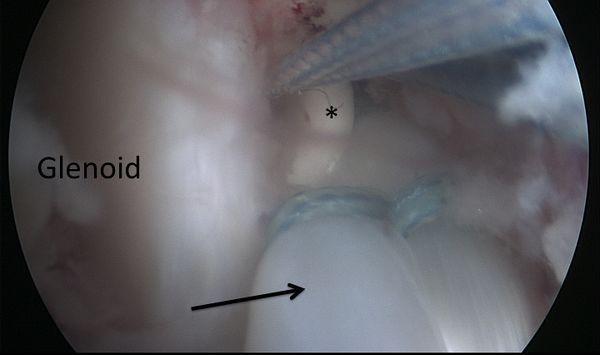
Bankart and Associate Repairs
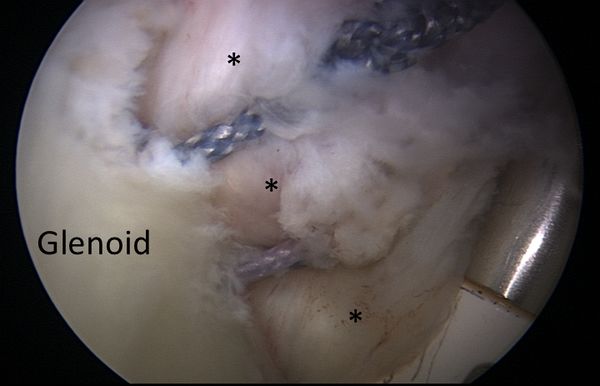
The aim of a Bankart repair is to restore anatomy by reattaching the labrum to the glenoid (Figure) and tighten the inferior glenohumeral ligament by shifting from inferior to superior. Several technical factors are also important to success. It is important to place anchors at the margin of the articular surface (as opposed to the glenoid neck) to allow recreation of the labral bumper. The surgeon must be sure to obtain a proper inferior to superior shift of the capsule (Neer’s modification). Although this surgery can be performed in an open manner, the advantage of an arthroscopic approach is that it preserves the subscapularis and allows assessment of associated pathology. The literature demonstrates that patients with low risk of recurrence will benefit from either an anatomic open or arthroscopic repair with an acceptable rate of recurrence.[109]
HAGL (Humeral Avulsion of the Glenohumeral Ligaments) lesions are uncommon causes of anterior instability. There are 3 variants of HAGL lesions: 1. Avulsion from bone 2. Capsular split 3. Combined bone avulsion and capsular split. These lesions can be can be addressed by repair or more easily by a Latarjet.
Remplissage
Remplissage has been described by Connoly123 and may be used as an adjunct to arthroscopic Bankart repair in the setting a of large Malgaigne (Hill-Sachs) lesion with glenoid bone loss of <25%.[110]
This technique consists of a posterior capsulodesis and infraspinatus tenodesis that fills the Malgaigne lesion. The purpose is to render the Malgaigne lesion extra-capsular, avoiding its engagement. Wolf et al. and Boileau et al. presented encouraging mid- to long-term results of arthroscopic remplissage and concomitant anterior Bankart repair.[111][112]
Surgical Technique
The arthroscope can typically remain in the posterior portal because the 70 degrees angle enhances appropriate visualization. Depending on patient anatomy, the arthroscope can be switched to the anterolateral portal to obtain another view of the defect. A spinal needle is centered over the Malgaigne (Hill-Sachs) lesion, and an accessory posterolateral portal is created 2 fingerbreadths lateral to the posterior viewing portal to allow orthogonal insertion of suture anchors. The use of a cannula is optional. A shaver is used to abrade the Malgaigne (Hill-Sachs) lesion. Two anchors are inserted in the valley of the defect adjacent to the articular margin, 1 superior and 1 inferior. If used, the cannula is at this point retracted into the subdeltoid space. A curved penetrating grasper is used to retrieve the inferior anchor suture, followed by a straight penetrating grasper for the superior anchor suture. The humeral head is reduced, and the inferior sutures are tied in mattress fashion in the subdeltoid space, followed by the superior sutures, to complete the remplissage.
Subscapularis Tendon Augmentation or Capsular Reconstruction
When traditional arthroscopic Bankart repair is not possible due to severe capsulolabral deficiency, different types of open or arthroscopic subscapularis tendon augmentation or capsular reconstruction have been described.[113][114][115][116]
Surgical technique
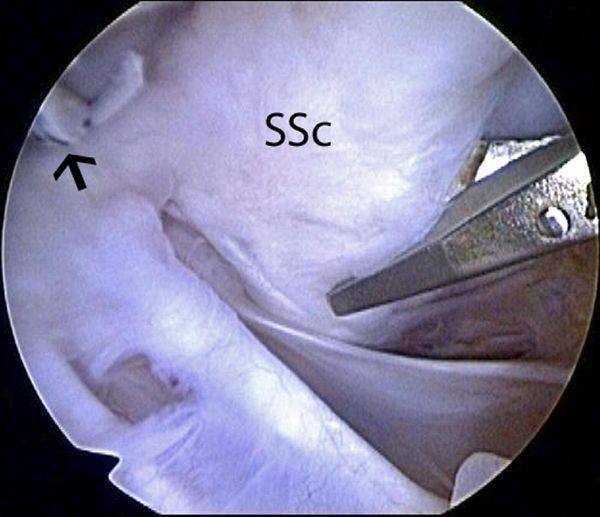
A standard diagnostic arthroscopy is performed with a 30 degrees arthroscope, viewing through a posterior portal with a pump maintaining pressure of 50 mm Hg. The labrum is inspected in its entirety. An anterior portal is established just above the lateral half of the subscapularis and medial to the sling of the biceps, by use of an 18-gauge spinal needle with an outside-in technique. An anterosuperolateral portal is similarly established off the anterolateral border of the acromion. This portal should be placed so that it provides a 45 degrees angle of approach to the superior glenoid. The arthroscope is placed in the anterosuperolateral portal, and the anterior labrum is more thoroughly inspected. The remaining capsulolabral sleeve is dissected from the glenoid neck with an arthroscopic elevator until the subscapularis muscle is visible deep to the cleft. A 2- to 3-mm strip of articular cartilage is removed along the glenoid rim with a ring curette, creating an enhanced bone bed for capsulolabral repair. A capsulolabral repair is performed inferiorly with whatever good tissue remains. An anteroinferior anchor is placed. After placement of this anchor, if there is insufficient capsulolabral tissue to create the desired “bumper” along the anterior glenoid rim, the surgeon must consider various reconstructive options, including a split subscapularis tendon flap.
Augmentation With Split Subscapularis Flap
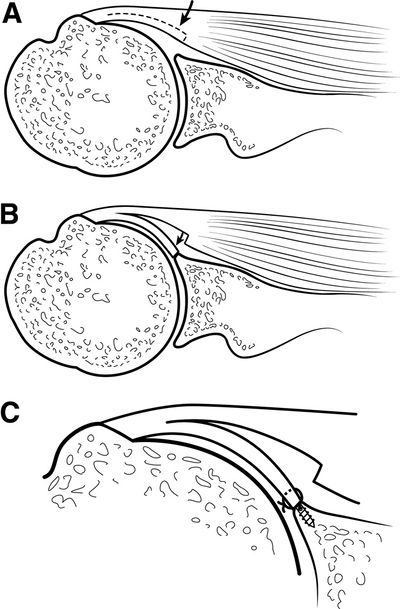
To augment the capsulolabral deficiency, a flap of the posterior portion of the superior half of the subscapularis tendon is mobilized and undergoes tenodesis to the anterior glenoid. This flap is created in a “trapdoor” fashion such that the capsular surface of the subscapularis tendon is reflected from medial to lateral as a separate lamina while the outer surface in left unaltered. By use of arthroscopic scissors introduced through the anterior portal, a longitudinal incision through one-half the thickness of the subscapularis is created in the superior half of the tendon (Figure).
Care is taken not to violate the full thickness of the subscapularis. The subscapularis flap dissection progresses from medial to lateral until the leading medial edge of the flap is mobile enough to reach the anterior glenoid. After mobilization of the subscapularis tendon flap, additional suture anchors are placed on the previously prepared glenoid strip at the 3-o'clock and 4-o'clock positions. Sutures from the anchor are passed through the subscapularis flap and tied as described previously. This completes the augmentation with a split subscapularis tendon flap (Figure).
Postoperatively, the patient's extremity is placed in a sling for 6 weeks. At the end of 6 weeks, stretching exercises are commenced with full forward flexion allowed and external rotation to half that of the contralateral shoulder. The goal is to achieve half the external rotation of the normal side at 3 months postoperatively. Strengthening is delayed until 4 months postoperatively because this is usually a last-resort salvage procedure. Return to full activities is delayed until 1 year postoperatively.
Dynamic Anterior Stabilization (DAS)
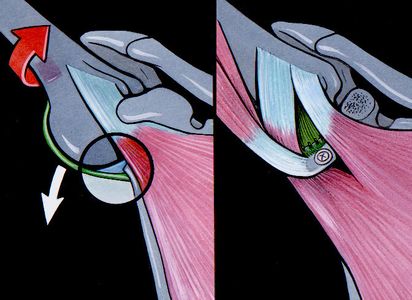
Dynamic anterior stabilization transfers the long head of the biceps to the anterior glenoid margin, thereby creating a “sling effect” (Figure).
The dynamic anterior stabilization technique provides decreased anterior glenohumeral translation in cases of Bankart lesions with limited anterior bone loss (<20%)[117]
In comparison with isolated Bankart repair it is able to stop the anterior translation less anterior and therefore reduces the risk of a conflict between the humeral head and the anterior margin of the glenoid. It is also easier and safer than arthroscopic Latarjet. Moreover, it does not require screws nor traction of the coracoid process, and should consequently reduce the risks of neurologic damage. Furthermore, the procedure can be performed with only 3 small incisions (Video), as it does not require coracoid transfer, which eliminates risks of nerve dissection, graft overhang and cortical resorption, hence reducing the probability for dislocation arthroplasty. Lastly, the pectoralis minor remains intact, which would avoid scapular dyskinesis. The potential drawbacks of the dynamic anterior stabilization are that it relies on the long head of biceps tendon, which has smaller diameter than the conjoint tendon, and could therefore have a weaker “sling effect” than that of the standard Latarjet. Also, there are, like in the Latarjet procedure, the risks of biceps pain, and secondary iatrogenic factors. Furthermore, in cases with larger bone defects (≥ 20 %) there is a relevant posterior and inferior shift of the humeral head in relation to the glenoid, when the arm is brought in the ABER position.(reference to be completed) Indications and limitations are yet to be defined and it is recommended that future studies are carried out with a more long-term follow-up.
Preoperative Patient Positioning
The operation, illustrated in the video, is performed in the semi-beach chair position under general anesthesia with an interscalene block. An examination under anesthesia is performed before prepping and draping the arm.
Initial Exposure and Portal Placement
An intra-articular approach is used through a standard posterior portal (soft spot), a standard diagnostic arthroscopy is performed with a 30-degree arthroscope and a pump maintaining pressure at 60 mm Hg. Antero-lateral and anterior portals are then established by an outside-in technique using a spinal needle as a guide. The rotator interval is opened, and the internal structures (glenoid defects, humeral defects, etc.) are further assessed with a probe.
Anterior Glenoid Preparation
From a lateral viewing portal, the labrum, if necessary, is detached from the glenoid, and a suture is passed around the labrum and pulled through the posterior portal to increase access for preparation of the anterior glenoid (Figure). The glenoid neck is cleaned from soft tissues at around 3 o’clock with a burr.

Addressing the Long Head of Biceps and Subscapularis Split
The long head of biceps is then tenotomized and the biciptal groove is opened laterally and distally to avoid detaching the subscapularis (Figure).
The biceps is then exteriorized, and secured 20 mm from the proximal tendon. From a lateral viewing portal the subscapularis is exposed on three sides, together with the lateral margin of the conjoint tendon. Three options exist to create a split in the middle of the subscapularis above the junction of the superior two-thirds used in the standard Latarjet procedure: From a lateral viewing portal, either a switching stick (Wissinger Rod) can be passed across the glenohumeral joint through a posterior approach at the level of the inferior glenoid (Figure), an outside-in approach can be used or simply by passing through the subscapularis muscle with a suture passer, by grabbing the sutures that secure the biceps and pulling the biceps through the tendon.
The switching stick is now found in the retrocoracoid space and maintained lateral to the conjoint tendon to avoid damaging the nerve plexus. The probe is then introduced through the anterior portal to complete the split.
Long Head of Biceps Tenodesis to Anterior Glenoid
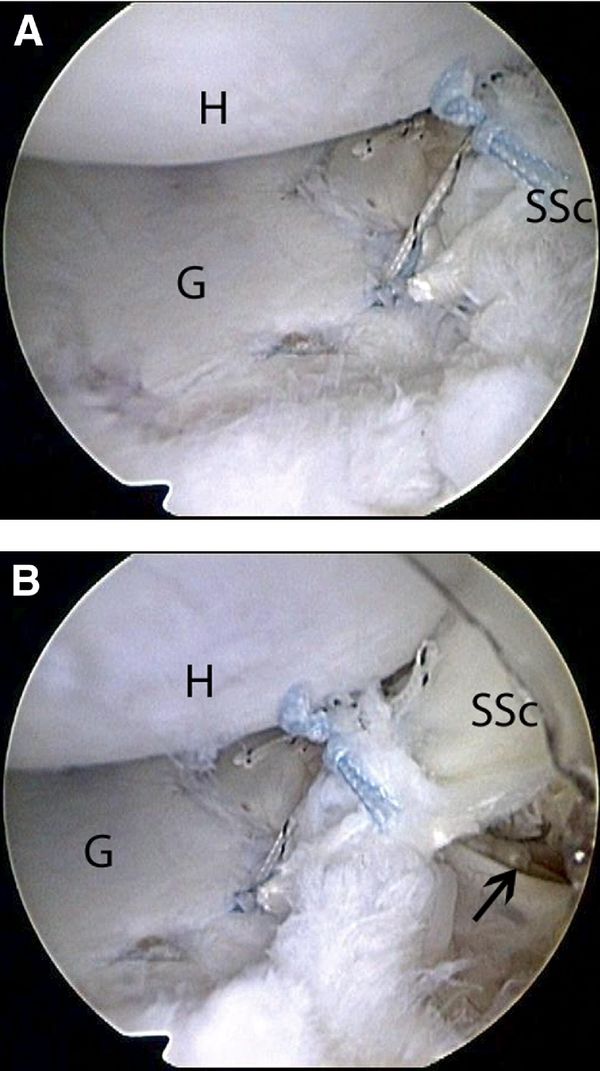
A drill is then used to prepare a hole at 3 o'clock from anterior to posterior within the neck of the glenoid, 2.0 cm deep, depending on the length of the interference screw. The LHB tendon is then passed through the subscapularis split into the pre-drilled hole, to establish the “sling effect”, and fixed using a tenodesis screw (Figure).
Labral Repair
With the arthroscope through the posterior portal, a standard Bankart repair is performed using 2-3 suture anchors. The anchors are placed on the glenoid rim at 3, 4, and 5 o’clock to enable the retention of the capsulo-ligamentous structures and to re-establish the labral damper effect (Video and Figure).
Postoperative Rehabilitation
Patients are instructed to wear a simple sling for 10 days encouraging rest and reducing the risk of post-operative hematoma formation. Rehabilitation with self-mobilization in elevation and external rotation is allowed from day 0. At 10 days, activities of daily living are allowed and self-mobilization in elevation and external rotation continued. Return to low-risk sports (eg, jogging, cycling, and swimming) is allowed at 6 weeks, and high-risk (throwing and collision) sports at 3 months only after satisfactory clinical and radiographic evaluations confirm satisfactory healing of the coracoid graft. Initially, no physiotherapy is recommended.
Bony procedures
In the setting of glenoid bone loss ≥20% of the glenoid diameter an arthroscopic Bankart repair has an unacceptably high rate of recurrence. Burkhart and DeBeer reported a 4% recurrence rate for arthroscopic Bankart repair when glenoid bone loss was <25%. However, with glenoid bone loss ≥25%, the recurrence rate was 67% with an arthroscopic approach. They subsequently recommended a bony procedure procedure in the population with substantial glenoid bone loss.[118]
Treatment is based on patient factors and associated pathology as previously discussed. In general, for patients under the age of 30, primary stabilization following a first traumatic anterior instability episode is offered. Such patients are counseled on the natural history or anterior instability and the potential for subsequent injury. For the majority of patients over the age of 30, nonoperative treatment is advised with standard sling immobilization for three weeks followed by progressive strengthening and return to activities. For such patients with persistent weakness or recurrent instability a magnetic resonance imaging (MRI) or MRI arthrogram is obtained to evaluate for an associated rotator cuff tear and stabilization is performed.
In consideration of the current literature, the following indications for osseous reconstruction procedures of the glenoid concavity can be recommended: - Substantial erosion-type defects (type IIIb), which constitute the instability-associated main pathology. - Chronic fragment-type defects (type II), where the glenoid area and concavity cannot be reconstructed by mobilization and refixation of the fragment. - In the rare patient with an acute, non-reconstructible, multifragmented glenoid fracture (type Ic). - In cases of revision surgery, e.g. after failed soft-tissue stabilization, a glenoid augmentation procedure is recommended also for smaller bony defects (type IIIa).
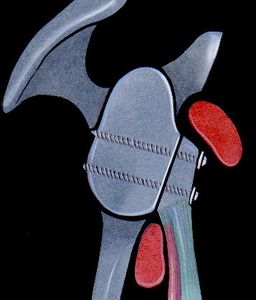
Latarjet
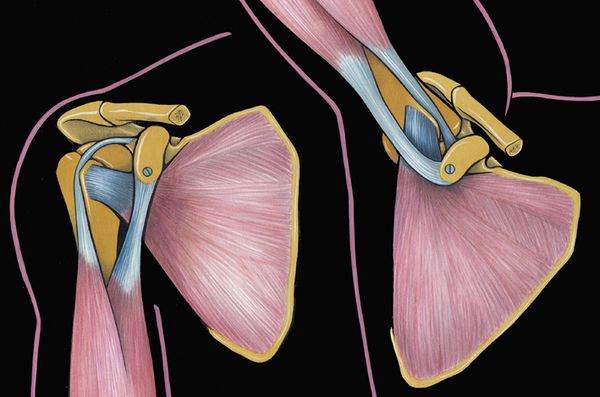
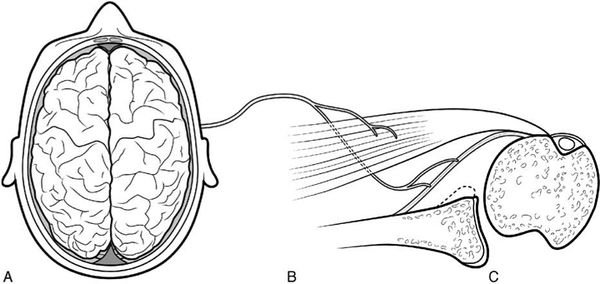
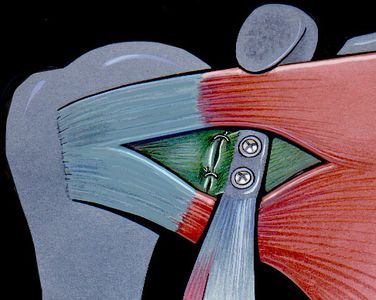
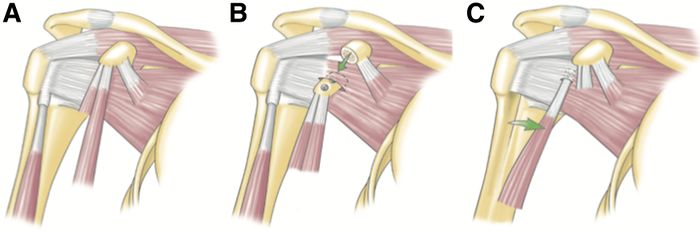
In 1954, Latarjet reported a coracoid transfer procedure in which the inferior aspect of the coracoid was secured to the anterior glenoid. The excellent stability of this procedure is obtained by a triple effect first proposed by Patte:[119]
1) the sling effect of the conjoint tendon when the arm is abducted and externally rotated, 2), the ‘‘bony effect’’ that increases or restore the glenoid anteroposterior diameter (Figure), and 3) the retensionning of inferior capsule to the stump of coracoacromial ligament, rending the coracoid extra-articular.
| A | B | C |
|---|
Figure. 28 Illustration of the three effects A) the sling effect, B) the bony effect and C) the retensioning of the capsule. Courtesy of Gilles Walch.
References
- ↑ Iqbal S, Jacobs U, Akhtar A, Macfarlane RJ, Waseem M. A history of shoulder surgery. Open Orthop J 2013;7:305-9.
- ↑ Hussein MK. Kocher's method is 3,000 years old. J Bone Joint Surg Br 1968;50:669-71.
- ↑ Celsus A. De Medicina.
- ↑ Hippocrates. Corpus Hippocraticum—De articulis.
- ↑ Malgaigne J. Traité des fractures et des luxations. Paris: J.-B. Baillière; 1855.
- ↑ Broca A, Hartmann H. Contribution à l'étude des luxations de l'épaule (luxations anciennes et luxations récidivantes). Bull Soc Anat 1890;4:416-23.
- ↑ Perthes G. Ueber Operationen beihabitueller Schulterluxation. Dtsch Z Chir 1906;85:199–227.
- ↑ Bankart AS. Recurrent or Habitual Dislocation of the Shoulder-Joint. British medical journal 1923;2:1132-3.
- ↑ Eden R. Zur Operation der habituellen Schulterluxation unter Mitteilung eines neuen Verfahrens bei Abriss am inneren Pfannenrande. Dsch Z Chir 1918;144:269.
- ↑ Hybinette S. De la transplantation d’un fragment osseux pour remédier aux luxations récidivantes de l’épaule. Acta Chir Scand 1932:411-45.
- ↑ Anonymous. Zentralbl Chir 1924;43:2402.
- ↑ Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir 1954;49:994-7.
- ↑ Helfet AJ. Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg Br 1958;40-B:198-202.
- ↑ Trillat A. Traitement de la luxation récidivante de l'épaule. Considérations techniques. Lyon Chir 1954:986-93.
- ↑ Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir 1954;49:994-7.
- ↑ Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res 2002:32-9.
- ↑ Romeo AA, Cohen BS, Carreira DS. Traumatic anterior shoulder instability. Orthop Clin North Am 2001;32:399-409.
- ↑ Goss TP. Anterior glenohumeral instability. Orthopedics 1988;11:87-95.
- ↑ Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med 2009;37:1750-4.
- ↑ Owens BD, Dickens JF, Kilcoyne KG, Rue JP. Management of mid-season traumatic anterior shoulder instability in athletes. J Am Acad Orthop Surg 2012;20:518-26.
- ↑ Bankart AS. Recurrent or Habitual Dislocation of the Shoulder-Joint. British medical journal 1923;2:1132-3.
- ↑ Neviaser TJ. The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy 1993;9:17-21.
- ↑ Neviaser TJ. The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy 1993;9:22-3.
- ↑ Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am 1994;76:1819-26.
- ↑ Wolf EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy 1995;11:600-7.
- ↑ Bigliani LU, Pollock RG, Soslowsky LJ, Flatow EL, Pawluk RJ, Mow VC. Tensile properties of the inferior glenohumeral ligament. J Orthop Res 1992;10:187-97.
- ↑ Habermeyer P, Gleyze P, Rickert M. Evolution of lesions of the labrum-ligament complex in posttraumatic anterior shoulder instability: a prospective study. J Shoulder Elbow Surg 1999;8:66-74.
- ↑ Urayama M, Itoi E, Sashi R, Minagawa H, Sato K. Capsular elongation in shoulders with recurrent anterior dislocation. Quantitative assessment with magnetic resonance arthrography. Am J Sports Med 2003;31:64-7.
- ↑ Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res 2002:32-9.
- ↑ Griffith JF, Antonio GE, Yung PS, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR American journal of roentgenology 2008;190:1247-54.
- ↑ Buscayret F, Edwards TB, Szabo I, Adeleine P, Coudane H, Walch G. Glenohumeral arthrosis in anterior instability before and after surgical treatment: incidence and contributing factors. Am J Sports Med 2004;32:1165-72.
- ↑ Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy 2003;19:732-9.
- ↑ Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94.
- ↑ Burkhart SS, Debeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002;18:488-91.
- ↑ Antonio GE, Griffith JF, Yu AB, Yung PS, Chan KM, Ahuja AT. First-time shoulder dislocation: High prevalence of labral injury and age-related differences revealed by MR arthrography. JMRI 2007;26:983-91.
- ↑ Itoi E, Tabata S. Rotator cuff tears in anterior dislocation of the shoulder. Int orthop 1992;16:240-4.
- ↑ Lazarus MD, Sidles JA, Harryman DT, 2nd, Matsen FA, 3rd. Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Joint Surg Am 1996;78:94-102.
- ↑ Matsen FA, 3rd, Harryman DT, 2nd, Sidles JA. Mechanics of glenohumeral instability. Clinics in sports medicine 1991;10:783-8.
- ↑ Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-20.
- ↑ Carpinteiro EP, Barros AA. Natural History of Anterior Shoulder Instability. Open Orthop J. 2017 Aug 31;11:909-918.
- ↑ Postacchini F, Gumina S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg 2000;9:470-4.
- ↑ Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am 1996;78:1677-84.
- ↑ Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7.
- ↑ Habermeyer P, Jung D, Ebert T. [Treatment strategy in first traumatic anterior dislocation of the shoulder. Plea for a multi-stage concept of preventive initial management]. Der Unfallchirurg 1998;101:328-41.
- ↑ Haller S, Cunningham G, Lädermann A, et al. Shoulder apprehension impacts large-scale functional brain networks. AJNR American journal of neuroradiology 2014;35:691-7.
- ↑ Boileau P, Zumstein M, Balg F, Penington S, Bicknell RT. The unstable painful shoulder (UPS) as a cause of pain from unrecognized anteroinferior instability in the young athlete. J Shoulder Elbow Surg 2011;20:98-106.
- ↑ Patte D, Bernageau J, Rodineau J, Gardes JC. [Unstable painful shoulders (author's transl)]. Rev Chir Orthop Reparatrice Appar Mot 1980;66:157-65.
- ↑ Patel MR, Pardee ML, Singerman RC. Intrathoracic Dislocation of the Head of the Humerus. J Bone Joint Surg Am 1963;45:1712-4.
- ↑ Wirth MA, Jensen KL, Agarwal A, Curtis RJ, Rockwood CA, Jr. Fracture-dislocation of the proximal part of the humerus with retroperitoneal displacement of the humeral head. A case report. J Bone Joint Surg Am 1997;79:763-6.
- ↑ Cook C, Beaty S, Kissenberth MJ, Siffri P, Pill SG, Hawkins RJ. Diagnostic accuracy of five orthopedic clinical tests for diagnosis of superior labrum anterior posterior (SLAP) lesions. J Shoulder Elbow Surg 2012;21:13-22.
- ↑ Gerber C, Terrier F, Ganz R. The Trillat procedure for recurrent anterior instability of the shoulder. J Bone Joint Surg Br 1988;70:130-4.
- ↑ Walch G, Agostini JY, Levigne C, Nove-Josserand L. [Recurrent anterior and multidirectional instability of the shoulder]. Rev Chir Orthop Reparatrice Appar Mot 1995;81:682-90.
- ↑ Gagey OJ, Gagey N. The hyperabduction test. J Bone Joint Surg Br 2001;83:69-74.
- ↑ 54.0 54.1 Hovelius L, Rahme H. Primary anterior dislocation of the shoulder: long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc 2016;24:330-42.
- ↑ Hovelius L, Vikerfors O, Olofsson A, Svensson O, Rahme H. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J Shoulder Elbow Surg 2011;20:1095-101.
- ↑ Lädermann A, Lubbeke A, Stern R, Cunningham G, Bellotti V, Gazielly DF. Risk factors for dislocation arthropathy after Latarjet procedure: a long-term study. International orthopaedics 2013;37:1093-8.
- ↑ Jobe FW, Kvitne RS, Giangarra CE. Shoulder pain in the overhand or throwing athlete. The relationship of anterior instability and rotator cuff impingement. Orthop Rev 1989;18:963-75.
- ↑ Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. The Journal of bone and joint surgery American volume 1981;63:863-72.
- ↑ Sherrington C. The Integrative Action of the Nervous System. New York: Charles Scribner's Sons; 1906.
- ↑ Haller S, Cunningham G, Lädermann A, et al. Shoulder apprehension impacts large-scale functional brain networks. AJNR American journal of neuroradiology 2014;35:691-7.
- ↑ Cunningham G, Zanchi D, Emmert K, et al. Neural Correlates of Clinical Scores in Patients with Anterior Shoulder Apprehension. Medicine and science in sports and exercise 2015;47:2612-20.
- ↑ Zanchi D, Cunningham G, Lädermann A, Ozturk M, Hoffmeyer P, Haller S. Structural white matter and functional connectivity alterations in patients with shoulder apprehension. Sci Rep 2017;7:42327.
- ↑ Zanchi D, Cunningham G, Lädermann A, Ozturk M, Hoffmeyer P, Haller S. Brain activity in the right-frontal pole and lateral occipital cortex predicts successful post-operatory outcome after surgery for anterior glenoumeral instability. Sci Rep 2017;7:498.
- ↑ Atef A, El-Tantawy A, Gad H, Hefeda M. Prevalence of associated injuries after anterior shoulder dislocation: a prospective study. International orthopaedics 2015.
- ↑ Lädermann A, Denard PJ, Tirefort J, et al. Does surgery for instability of the shoulder truly stabilize the glenohumeral joint?: A prospective comparative cohort study. Medicine (Baltimore) 2016;95:e4369.
- ↑ Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A. Neurophysiological investigation of the basis of the fMRI signal. Nature 2001;412:150-7.
- ↑ Haller S, Cunningham G, Lädermann A, et al. Shoulder apprehension impacts large-scale functional brain networks. AJNR American journal of neuroradiology 2014;35:691-7.
- ↑ Cieslik EC, Zilles K, Caspers S, et al. Is there "one" DLPFC in cognitive action control? Evidence for heterogeneity from co-activation-based parcellation. Cereb Cortex 2013;23:2677-89.
- ↑ Zanchi D, Cunningham G, Lädermann A, Ozturk M, Hoffmeyer P, Haller S. Structural white matter and functional connectivity alterations in patients with shoulder apprehension. Sci Rep 2017;7:42327.
- ↑ Zanchi D, Cunningham G, Lädermann A, Ozturk M, Hoffmeyer P, Haller S. Brain activity in the right-frontal pole and lateral occipital cortex predicts successful post-operatory outcome after surgery for anterior glenoumeral instability. Sci Rep 2017;7:498.
- ↑ Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am 2012;94:18-26.
- ↑ Antonio GE, Griffith JF, Yu AB, Yung PS, Chan KM, Ahuja AT. First-time shoulder dislocation: High prevalence of labral injury and age-related differences revealed by MR arthrography. JMRI 2007;26:983-91.
- ↑ Atef A, El-Tantawy A, Gad H, Hefeda M. Prevalence of associated injuries after anterior shoulder dislocation: a prospective study. Int Orthop. 2016 Mar;40(3):519-24.
- ↑ Fyhr C, Gustavsson L, Wassinger C, Sole G. The effects of shoulder injury on kinaesthesia: a systematic review and meta-analysis. Man Ther 2015;20:28-37.
- ↑ Myers JB, Lephart SM. Sensorimotor deficits contributing to glenohumeral instability. Clin Orthop Relat Res 2002:98-104.
- ↑ Liavaag S, Stiris MG, Svenningsen S, Enger M, Pripp AH, Brox JI. Capsular lesions with glenohumeral ligament injuries in patients with primary shoulder dislocation: magnetic resonance imaging and magnetic resonance arthrography evaluation. Scandinavian journal of medicine & science in sports 2011;21:e291-7.
- ↑ Antonio GE, Griffith JF, Yu AB, Yung PS, Chan KM, Ahuja AT. First-time shoulder dislocation: High prevalence of labral injury and age-related differences revealed by MR arthrography. JMRI 2007;26:983-91.
- ↑ Ropars M, Cretual A, Kaila R, Bonan I, Herve A, Thomazeau H. Diagnosis and treatment of anteroinferior capsular redundancy associated with anterior shoulder instability using an open Latarjet procedure and capsulorrhaphy. Knee Surg Sports Traumatol Arthrosc 2016;24:3756-64.
- ↑ Patte D, Bernageau J, Rodineau J, Gardes JC. [Unstable painful shoulders (author's transl)]. Rev Chir Orthop Reparatrice Appar Mot 1980;66:157-65.
- ↑ Boileau P, Zumstein M, Balg F, Penington S, Bicknell RT. The unstable painful shoulder (UPS) as a cause of pain from unrecognized anteroinferior instability in the young athlete. J Shoulder Elbow Surg 2011;20:98-106.
- ↑ Singer GC, Kirkland PM, Emery RJ. Coracoid transposition for recurrent anterior instability of the shoulder. A 20-year follow-up study. J Bone Joint Surg Br 1995;77:73-6.
- ↑ Lädermann A, Tirefort J, Zanchi D, Haller S, Charbonnier C, Cunningham G. Shoulder Apprehension: a Multifactorial Approach. EFORT Open Rev. 2018 24;3(10):550-557
- ↑ Lädermann A, Denard PJ, Tirefort J, et al. Does surgery for instability of the shoulder truly stabilize the glenohumeral joint?: A prospective comparative cohort study. Medicine (Baltimore) 2016;95:e4369.
- ↑ Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7.
- ↑ Rouleau DM, Hebert-Davies J, Djahangiri A, Godbout V, Pelet S, Balg F. Validation of the instability shoulder index score in a multicenter reliability study in 114 consecutive cases. Am J Sports Med 2013;41:278-82.
- ↑ Bloom MH, Obata WG. Diagnosis of posterior dislocation of the shoulder with use of Velpeau axillary and angle-up roentgenographic views. J Bone Joint Surg Am 1967;49:943-9.
- ↑ Bernageau J, Patte D, Debeyre J, Ferrane J. [Value of the glenoid profile in recurrent luxations of the shoulder]. Rev Chir Orthop Reparatrice Appar Mot 1976;62:142–7.
- ↑ Lädermann A, Bohm E, Tay E, Scheibel M. Bone-mediated anteroinferior glenohumeral instability : Current concepts. Der Orthopade 2018.
- ↑ Collin P, Lädermann A. Dynamic Anterior Stabilization Using the Long Head of the Biceps for Anteroinferior Glenohumeral Instability. Arthrosc Tech 2018;7:e39-e44.
- ↑ Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg 2011;20:S61-9.
- ↑ Ropars M, Cretual A, Kaila R, Bonan I, Herve A, Thomazeau H. Diagnosis and treatment of anteroinferior capsular redundancy associated with anterior shoulder instability using an open Latarjet procedure and capsulorrhaphy. Knee Surg Sports Traumatol Arthrosc 2016;24:3756-64.
- ↑ Kocher E. Eine neue Reductionsmethode für Schulterverrenkung. Berlin Klin 1870;7:101-5.
- ↑ Horvat JC. [Reconstruction of the spinal cord and its motor connections using embryonal nervous tissue transplantation and peripheral nerve autotransplantation. A study in the adult rat]. Neurochirurgie 1991;37:303-11.
- ↑ Salles JI, Velasques B, Cossich V, et al. Strength training and shoulder proprioception. J Athl Train 2015;50:277-80.
- ↑ Fyhr C, Gustavsson L, Wassinger C, Sole G. The effects of shoulder injury on kinaesthesia: a systematic review and meta-analysis. Man Ther 2015;20:28-37.
- ↑ deCharms RC, Maeda F, Glover GH, et al. Control over brain activation and pain learned by using real-time functional MRI. Proceedings of the National Academy of Sciences of the United States of America 2005;102:18626-31.
- ↑ Antunes A, Carnide F, Matias R. Real-time kinematic biofeedback improves scapulothoracic control and performance during scapular-focused exercises: A single-blind randomized controlled laboratory study. Hum Mov Sci 2016;48:44-53.
- ↑ Huang HY, Lin JJ, Guo YL, Wang WT, Chen YJ. EMG biofeedback effectiveness to alter muscle activity pattern and scapular kinematics in subjects with and without shoulder impingement. J Electromyogr Kinesiol 2013;23:267-74.
- ↑ Das De S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am 2013;95:76-81.
- ↑ Moroder P, Minkus M, Bohm E, Danzinger V, Gerhardt C, Scheibel M. Use of shoulder pacemaker for treatment of functional shoulder instability: Proof of concept. Obere Extrem 2017;12:103-8.
- ↑ de Laat EA, Visser CP, Coene LN, Pahlplatz PV, Tavy DL. Nerve lesions in primary shoulder dislocations and humeral neck fractures. A prospective clinical and EMG study. J Bone Joint Surg Br 1994;76:381-3.
- ↑ Brown FW, Navigato WJ. Rupture of the axillary artery and brachial plexus palsy associated with anterior dislocation of the shoulder. Report of a case with successful vascular repair. Clin Orthop Relat Res 1968;60:195-9.
- ↑ Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am 1996;78:1677-84.
- ↑ te Slaa RL, Brand R, Marti RK. A prospective arthroscopic study of acute first-time anterior shoulder dislocation in the young: a five-year follow-up study. J Shoulder Elbow Surg 2003;12:529-34.
- ↑ Postacchini F, Gumina S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg 2000;9:470-4.
- ↑ Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am 2006;88:2326-36.
- ↑ Murray IR, Ahmed I, White NJ, Robinson CM. Traumatic anterior shoulder instability in the athlete. Scandinavian journal of medicine & science in sports 2013;23:387-405.
- ↑ Handoll HH, Almaiyah MA, Rangan A. Surgical versus non-surgical treatment for acute anterior shoulder dislocation. The Cochrane database of systematic reviews 2004:CD004325.
- ↑ Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy 2013;29:920-33.
- ↑ Connoly J. Humeral head defects associated with shoulder dislocations. American Academy of Orthopaedic Surgeons Instructional course lectures: Mosby; 1972:42-54.
- ↑ Boileau P, O'Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am 2012;94:618-26.
- ↑ Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg 2014;23:814-20.
- ↑ Denard PJ, Narbona P, Lädermann A, Burkhart SS. Bankart augmentation for capsulolabral deficiency using a split subscapularis tendon flap. Arthroscopy 2011;27:1135-41.
- ↑ Maiotti M, Massoni C, Russo R, Schroter S, Zanini A, Bianchedi D. Arthroscopic Subscapularis Augmentation of Bankart Repair in Chronic Anterior Shoulder Instability With Bone Loss Less Than 25% and Capsular Deficiency: Clinical Multicenter Study. Arthroscopy 2016.
- ↑ Maiotti M, Russo R, Zanini A, Schroter S, Massoni C, Bianchedi D. Arthroscopic Bankart repair and subscapularis augmentation: an alternative technique treating anterior shoulder instability with bone loss. J Shoulder Elbow Surg 2016;25:898-906.
- ↑ Russo R, Della Rotonda G, Cautiero F, et al. Arthroscopic Bankart repair associated with subscapularis augmentation (ASA) versus open Latarjet to treat recurrent anterior shoulder instability with moderate glenoid bone loss: clinical comparison of two series. Musculoskelet Surg 2016.
- ↑ Mehl J, Otto A, Imhoff FB, Murphy M, Dyrna F, Obopilwe E, Cote M, Lädermann A, Collin P, Beitzel K, Mazzocca AD. Dynamic Anterior Shoulder Stabilization With the Long Head of the Biceps Tendon: A Biomechanical Study. Am J Sports Med. 2019 May;47(6):1441-1450.
- ↑ Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94.
- ↑ Patte D, Debeyre J. Luxations récidivantes de l’épaule. Tech Chir Orthop Paris: Encycl Med Chir 1980:44–52.