Difference between revisions of "Shoulder:Rotator Cuff Pathology/Thickness Rotator Cuff Tears/Posterosuperior Rotator Cuff Tears and Associated Pathologies"
| Line 49: | Line 49: | ||
Supraspinatus is an external rotator.<ref>Inman VT, Saunders M, Abbott, MC. Observations on the function of the shoulder joint. J Bone Joint Surg Br. 1944;1(26):1-30</ref> It also initiates abduction in conjunction with deltoid, serrates anterior and infraspinatus. The following tests are consequently not specific for the supraspinatus but are sensitive due to antalgique reflex. Superior rotator cuff insufficiency, present in complete tears, is usually associated with a positive Jobe manoeuver (empty can)(Figure) and decreased strength in external resistance elbow at the side (Figure).<ref>Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med 1982;10:336-9.</ref> | Supraspinatus is an external rotator.<ref>Inman VT, Saunders M, Abbott, MC. Observations on the function of the shoulder joint. J Bone Joint Surg Br. 1944;1(26):1-30</ref> It also initiates abduction in conjunction with deltoid, serrates anterior and infraspinatus. The following tests are consequently not specific for the supraspinatus but are sensitive due to antalgique reflex. Superior rotator cuff insufficiency, present in complete tears, is usually associated with a positive Jobe manoeuver (empty can)(Figure) and decreased strength in external resistance elbow at the side (Figure).<ref>Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med 1982;10:336-9.</ref> | ||
| − | [[File:Jobe test.mov|thumb|Jobe test | + | [[File:Jobe test.mov|thumb|The Jobe test is performed by placing the patient's arms at 90 degrees of abduction within the scapular plane, maximally internally rotating the arms and resisting further abduction by the patient. A positive test occurs with localized pain to the affected arm.]] |
[[File:cuff104_2.jpg|thumb|Testing of the strength in external resistance elbow at the side.]] | [[File:cuff104_2.jpg|thumb|Testing of the strength in external resistance elbow at the side.]] | ||
Revision as of 07:30, 18 September 2020
Contents
- 1 Bullet Points
- 2 Key Words
- 3 Biomechanics of the Posterosuperior Rotator Cuff
- 4 Clinical examination
- 5 Imaging
- 6 Classification
- 6.1 Type A: Bony Involvement
- 6.2 A.3 Tuberosity Insufficiency
- 6.3 Surgical Technique
- 6.4 Type B: Full Thickness Tendon Lesion
- 6.4.1 B1: Lateral tendinous disruption
- 6.4.1.1 Size of Tendon Lesion
- 6.4.1.2 Tendon Retraction
- 6.4.1.3 Tear Pattern
- 6.4.1.4 Releases for the Rotator Cuff
- 6.4.1.5 Double-Row Versus Single-Row Cuff Repair
- 6.4.1.6 Margin Convergence
- 6.4.1.7 Load Sharing Rip Stop Construct
- 6.4.1.8 Massive Posterosuperior Rotator Cuff Tears
- 6.4.1.9 Definition and Classification of Massive Rotator Cuff Tears
- 6.4.1.10 Rotator Cuff Incarceration in the Glenohumeral Joint
- 6.4.1.11 Suprascapular Nerve Neuropathy and Massive Rotator Cuff Tear
- 6.4.2 Treatment Options for Massive Rotator Cuffs
- 6.4.3 B2: Medial Tendinous Disruption
- 6.4.1 B1: Lateral tendinous disruption
- 6.5 B3: Tendon to Tendon Adhesion: “Fosbury Flop Tear”
- 6.6 Type C: Musculotendinous Junction Lesion
- 6.7 Type D: Muscle Insufficiency
- 7 Irreparable Rotator Cuff Tears
- 8 What would Codman have thought about this?
- 9 References
Bullet Points
- The rotator cable explains why patients with most rotator cuff tears can maintain active forward flexion, and also why even after only a partial rotator cuff repair, good functional results can be achieved.
- The most important negative prognostic factor is high-grade fatty infiltration of the rotator cuff muscle bellies (grade 3 or 4 fatty infiltration).
- The tangent sign is an indicator of advanced fatty infiltration and is a predictor of whether a rotator cuff tear will be reparable.
- Full thickness disruption of the lateral tendon stump (B1) is the most frequent type of rotator cuff lesion, comprising approximately 90% of all surgically treated lesions.
- Musculotendinous junction lesions (C-type) or rare and characterized by an edema of the muscle belly. They are associated to calcific deposit (infraspinatus) or trauma (supraspinatus). Unrepaired, grade III lesions lead rapidly to grade 4 fatty infiltration of the muscle.
- Tendon retraction is classified according to Patte. Overreduction and lateral transposition of the tendon over the greater tuberosity may be unphysiological.
- Massive rotator cuff has different definitions in the literature, each having potential benefits or drawbacks.
- Massive rotator cuff tears comprise approximately 20% of all cuff tears and 80% of recurrent tears.
- The classification of Collin not only subclassifies massive tears but has also been linked to function, particularly the maintenance of active elevation.
- Non-surgical treatment is effective in patient with massive rotator cuff if the tear involves less than three tendons and do not involves the subscapularis (D-type).
- Biomechanical testing has consistently demonstrated the superiority of double-row constructs over single-row. However, there is no obvious difference clinically.
- There is actually no support for routine suprascapular nerve release when massive rotator cuff repair is performed.
- Functional outcome improved after revision rotator cuff repair and 70% or more of patients were satisfied or very satisfied. However, the prevalence of persistent defect (retear or non-healing) is 28% at six months and 40% at two years.
- Rotator cuff are irreparable when associated to true pseudoparalysis with the presence of lag signs (external rotation lag, drop, dropping, hornblower signs), femoralization of the humerus or acetabulization of the acromion, grade 3 or 4 fatty infiltration and tangent sign.
- The current literature does not support the initial use of complex and expensive techniques in the management of posterosuperior irreparable rotator cuff tears.
Key Words
Shoulder arthroscopy; Rotator cuff lesion; Partial repair; Tear pattern; Classification; Massive; Reparable and non-repairable; Irreparable; Imaging; Recurrent; Failed; Revision surgery; Open and arthroscopic approach; Conservative or non-operative treatment; Physiotherapy; Functional outcomes; Prognostic factors; Latissimus dorsi transfer; Subacromial spacer interposition; Balloon; Biceps tenotomy; Superior capsular reconstruction; Reverse arthroplasty; Magnetic resonance imaging (MRI) arthrography (MRA); Fosbury flop tear; New tear pattern; FUSSI; SAM.
Biomechanics of the Posterosuperior Rotator Cuff
A primary function of the rotator cuff is to work synergistically with the deltoid to maintain a balanced force couple about the glenohumeral joint. A force couple is a pair of forces that act on an object and tend to cause it to rotate. For any object to be in equilibrium, the forces must create moments about a center of rotation that are equal in magnitude and opposite in direction. Coronal and transverse plane force couples exist between the subscapularis anteriorly and infraspinatus and teres minor posteriorly. The rotator cuff force across the glenoid provides concavity compression, which creates a stable fulcrum and allows the periscapular muscles to move the humerus around the glenoid.
The rotator cable is a thickening of the rotator cuff that has been likened to a suspension bridge in which force is distributed through cables that are supported by pillars (the anterior and posterior attachments). The anterior rotator cable attachment bifurcates to attach to bone just anterior and posterior to the proximal aspect of the bicipital groove. The posterior attachment comprises the inferior 50% of the infraspinatus. With small central tears the cable attachments often stay intact and forces are transmitted along the rotator cable. The rotator cable also explains why patients with most rotator cuff tears can maintain active forward flexion, and also why even after only a partial rotator cuff repair, good functional results can be achieved.[1]
However, in the setting of massive rotator cuff with rotator cable disruption and non-compensation by other humeral head stabilizers (i.e pectoralis major and latissimus dorsi), the moments created by the opposing muscular forces are insufficient to maintain equilibrium in the coronal plane, resulting in altered kinematics, instability, and ultimately in pseudoparalysis. Interestingly, only few patients with an irreparable rotator cuff tears developed pseudoparalysis and arthritis.This finding has at least two potential explanations. First, the subscapularis that may not be involved in these tears is the key factor of active forward flexion.[2]
Second, the rotator cable, has still an intact anterior attachment which is important for elevation. This may explain why patients can maintain active mobility, and also why even after only a partial rotator cuff repair, good functional results can be achieved.[3]
Consequently, all the conditions for an imbalance in the force couples are not always met and subsequently loss of function is only occasionally seen.
Clinical examination
Inspection
Inspection has to rule out deformation, swelling (i.e Milwaukee shoulder syndrome, Figure) or hematoma (Video).
Palpation
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
Range of Motion
The patient must be examined not only in the standing position, but also supine on a table in order to block scapulothoracic movements, and look for all amplitudes (anterior elevation, abduction, internal rotation and external rotation elbow at the side and at 90 degrees of abduction.
Tests for posterosuperieur rotator cuff lesions lesions
Supraspinatus
Supraspinatus is an external rotator.[4] It also initiates abduction in conjunction with deltoid, serrates anterior and infraspinatus. The following tests are consequently not specific for the supraspinatus but are sensitive due to antalgique reflex. Superior rotator cuff insufficiency, present in complete tears, is usually associated with a positive Jobe manoeuver (empty can)(Figure) and decreased strength in external resistance elbow at the side (Figure).[5]
Testing of abduction strength in the champagne toast position, i.e., 30 degrees of abduction, mild external rotation, and 30 degrees of flexion, better isolates the activity of the supraspinatus from the deltoid than Jobe's “empty can” position (Figure).[6]
Infraspinatus and Teres Minor
Strength in External Rotation Elbow at the Side
Strength in external rotation elbow at the side of the supraspinatus, infraspinatus and teres minor represents approximately 10%, 70% and 20% of total external rotation strength, respectively.[7]
However, the function of the teres minor may become more important in the setting of a chronic infraspinatus tear, as its hypertrophy is commonly observed in these cases and probably compensates for external rotation weakness.
External Rotation Lag Sign
The external rotation lag sign (Figure and Video), described by Hertel, was designed to test the integrity of infraspinatus and supraspinatus tendons.[8]
The extent of internal rotation is recorded to the nearest 10 degrees degrees (10, 20, 30 and 40 degrees or above). An external rotation lag sign > 40 degrees seems to be the most reliable test for the teres minor.[9]

Drop Sign
The drop sign (Figure and Video), also described by Hertel, is designed to assess the function of the infraspinatus.

Hornblower sign
The patient is asked to bring both hands to his mouth, but is unable to do so without abducting the affected arm (Video).
Patte Test
The Patte test (Figure and Video) is the only test that allowed to analyze the muscular strength of the teres minor in case of deficient infraspinatus.[10]
Walch et al. reported a 100% sensitivity and 93% specificity with the Patte test and teres minor fatty atrophy Grade 3 or greater.[11]

A) The Patte test is performed by passively taking from a starting point of 90 degrees of abduction in the scapular plane, an elbow flexion of 90 degrees without external rotation.
B) The patient is asked to perform external rotation of the shoulder from this position against resistance. A positive Patte test is defined as external rotation power less than MRC Grade 4. Reproduce from [12], with permission.
Dropping Sign
The dropping sign of Neer had a 100% sensitivity and 66% specificity for teres minor involvement.[13][14]
Imaging
X-rays
The analysis should always begin with plain radiographic views to determine the morphology and status of the glenohumeral joint to exclude glenohumeral arthritis:
Anteroposterior True anteroposterior X-ray with the arm in neutral rotation, and the patient relaxed is obtained to evaluate the shape of the acromion and greater tuberosity, the critical shoulder angle, and the acromiohumeral distance. A decreased acromiohumeral distance < 7 mm in a standard antero-posterior radiograph indicates superior migration of the humeral head which increases the probability of finding an irreparable cuff tear. Such distance is correlated to 1) tears of the infraspinatus that mainly acts in lowering the humeral head, and 2) varying degrees of fatty infiltration.[15][16]
Nevertheless, such criteria should be interpreted with parsimony. First, it is difficult in clinical practice to obtain standardized X-rays making measurement aleatory. Second, this distance has not been associated with an inability to obtain an intra-operative complete repair of the supraspinatus (18.2% irreparable, OR = 0.55, P = 0.610).[17]
At the end of the spectrum, acetabularization of the acromion and femoralization of the humeral head are pre-operative adapting factors reflecting significant chronic static superior instability and are a contraindication for repair.
Lateral Y-view (Lamy)
Lateral Y-view (Lamy) is used to analyze the presence of a spur, the shape of the acromion on this view is less accurate to detect full-thickness rotator cuff tear.[18]
Axillary lateral
An axillary lateral view can exclude static anterior subluxation or os acromialis.
If pathology of the acromioclavicular joint is suspected, a Zanca view is additionally acquired.[19]
Ultrasound (US)
Following X-ray evaluation, advanced imaging modalities are obtained to confirm and plan treatment. Ultrasonography is an excellent cost-effective screening tool in the office but does not allow evaluation of intra-articular pathology or easy evaluation of muscle quality.
Rotator Cuff Interval
The space through which the long head of the biceps passes as it leaves the glenohumeral joint is called the rotator cuff interval. The patient position is the same as for evaluation of the long head of the biceps, with the probe being placed slightly superiorly to the bicipital groove and in the axial plane (Figure). The long head of the biceps is thus visualized with the subscapularis medially and the supraspinatus laterally, while the coracohumeral and superior glenohumeral ligaments surround it.[20]

Supraspinatus Tendon and Subacromial-Subdeltoid Bursa
The supraspinatus tendon is best visualized with the shoulder in abduction and internal rotation, by asking the patient to place the palm of their hand on their back pocket, elbow pointed backwards (Figure). In patients presenting with reduced range of motion (adhesive capsulitis for example), maximal internal rotation with the arm hanging by the side of the thorax can be sufficient. The long axis of the tendon is most useful for analyzing integrity of the tendon on the footprint (measuring approx. 2 cm medially to laterally), and is visualized by holding the probe in a tilted position (therefore not a true coronal plane but at an approx. 45 degree angle, following the line of the humerus (Figure)).
This position also allows visualization of two other structures: the subacromial-subdeltoid bursa (and the presence of excessive liquid, see below) and the humeral head along with its articular cartilage (and possible surface defects). In the axial plane (again not truly axial but at 90 degrees to the previous plane), the leading edge of the supraspinatus can be identified laterally to the biceps tendon. Moving the probe laterally will reveal the mid-portion of the tendon, with the anterior part of the infraspinatus eventually coming into view as an anisotropic and dark image (as the fibers run in a different plane).

Ultrasound image (a) with superimposed anatomy (b), patient/probe position (c), and landmarks for measurement of these two structures (d). Reproduced from Plomb-Holmes et al., with permission
Infraspinatus and teres minor tendon, glenohumeral joint, spinoglenoid notch
The infraspinatus tendon, which inserts posteriorly to the supraspinatus tendon, is best examined in its long axis by elongating it (the patient placing his or her hand on the opposite shoulder) and placing the probe on the posterior part of the patient’s shoulder (Figure). The insertion of the tendon on the humeral head can be analyzed, as well as the musculotendinous junction by sliding the probe medially. At this point, the glenohumeral joint line and posterior labrum can be visualized in thin patients, and even more medially, the spinoglenoid notch containing the suprascapular neurovascular bundle (and the possible presence of a ganglion cyst arising from the posterior labrum which can compress the bundle) (Figure). The teres minor tendon can be difficult to separate from the infraspinatus tendon; it is located inferiorly and has a similar aspect, but can be distinguished by the fact that deeper to it lies bone whereas the infraspinatus lies on articular cartilage, and its insertion is primarily muscular (vs. tendinous).
Magnetic Resonance Imaging (MRI) and Computer Tomography (CT)
Magnetic resonance imaging accurately estimates tear pattern, muscle fatty infiltration and atrophy, tendon length and retraction, and is thus obtained to plan repair or reconstructive surgeries. The muscle bellies of the rotator cuff are assessed, if available, on T1-weighted axial, coronal, sagittal views with cuts sufficiently medial on the scapula to allow proper assessment regardless of retraction. Finally, computer tomography (CT) scans are used if magnetic resonance imaging is contraindicated or if joint replacement is planned, particularly in the setting of glenoid deformity. Additionally, computer tomography (CT) scan can be conducted with intra-articular contrast to assess the cuff. It should be noted that the magnetic resonance imaging and computer tomography are not reliable to analyze the acromiohumeral distance as they are performed in lying position.
Fatty Infiltration
The most important negative prognostic factor is high-grade fatty infiltration of the rotator cuff muscle bellies (grade 3 or 4 fatty infiltration) (Figure).
Fatty infiltration is irreversible even with repair and leads to reduced function of the rotator cuff musculature.[21]
If pathology of the acromioclavicular joint is suspected, a Zanca view is additionally acquired.[22][23][24]
Atrophy
The presence or absence of supraspinatus atrophy is determined using the tangent sign of Zanetti et al. (Figure).[25]

This sign is an indicator of advanced fatty infiltration and has been reported to be a predictor of whether a rotator cuff tear will be reparable.[26][27]
An inability to obtain a complete repair of the supraspinatus is associated with a positive tangent sign (30% irreparable) versus a negative tangent sign (6.3% irreparable, OR = 6,3, P =0.0102).[28]
Supraspinatus atrophy can also be determine according to Thomazeau classification.[29]
Agreement for this classification is however fair (intra-observer kappa = 0,51 and inter-observer kappa = 0.30) and its use cannot be recommended as a criteria of reparability.[30]
Classification
Reproduced from Lädermann A, Burkhart SS, Hoffmeyer P, et al. Classification of full-thickness rotator cuff lesions: a review. EFORT Open Rev 2016;1:420-30, with permission
The rotator cuff lesions are categorized into four major groups based on involvement of the bone (Type A), tendon (Type B), musculotendinous junction (Type C) or muscle insufficiency (Type D).
Type A: Bony Involvement
While the majority of rotator cuff lesions involve the tendinous insertion, bony involvement is an important consideration. Bony involvement includes acute fractures, malunion/nonunion, and chronic bony insufficiency.
A1. Acute Bony Involvement (Fractures and Avulsions)
Isolated greater tuberosity fractures are considered uncommon, representing less than 5% of all operatively treated proximal humeral fractures.[31]
Isolated lesser tuberosity fractures are generally considered rare. Type A lesion of the greater or lesser tuberosity represent approximately 3.2% and 1.1% respectively of surgically treated rotator cuff lesions (Table). Tuberosity fractures are included in the accepted classification for proximal humeral fractures by Neer, in itself a modification of Codman’s original description. Because the greater and lesser tuberosity are the insertion site of the rotator cuff, even small tuberosity fractures or avulsions can represent substantial disruption of the rotator cuff and lead to functional impairment if displaced and left untreated. Historically, Neer proposed 10 mm of displacement as a threshold for operative intervention.[32]
However, more recent investigation has recommended that a threshold of 5 mm31 should be used.[33]
Displacement of greater than 5 mm can lead to bony impingement with loss of range of motion as well as loss of strength from compromise in the normal length–tension relationship of the rotator cuff. A traumatic mechanism is typical such as violent muscular contraction, impaction of the greater tuberosity beneath the acromion, or shearing against the anterior glenoid rim during a glenohumeral dislocation event. Thorough patient evaluation is required to make an appropriate treatment recommendation. Conservative therapy is limited to non- or minimally-displaced fractures. The ongoing development of arthroscopic techniques has led to multiple reports about arthroscopically assisted or total arthroscopic techniques in the treatment of these injuries.[34]
A.2 Tuberosity Malunion/Nonunion
Tuberosity malunion or nonunion can be a sequela of either conservative treatment or surgical treatment of acute injuries. As noted previously, displacement effectively shortens the muscle-tendon unit such that the rotator cuff cannot function properly (Figures).


Various open techniques have been described for the management of the malunion of proximal humeral fractures, including prosthetic reconstruction, open corrective osteotomy, or arthroscopic capsular release followed by takedown of the rotator cuff from the malunited proximal humerus, tuberoplasty, and then rotator cuff advancement. Although the latter technique is technically demanding, it allows preservation of the native humeral head, which is associated with a low complication rate, and avoids concerns about long-term prosthetic survival in young patients (Video).[35][36]
Operative Technique
The patient was placed in a beach chair or in a lateral decubitus position. A diagnostic arthroscopy is performed with an arthroscopic pump maintaining pressure at 50 mm Hg. The joint surfaces were inspected to rule out any incongruities. The articular side of the rotator cuff is carefully assessed with a probe searching for tears. Any capsular retraction is addressed at this point. A release of the rotator interval and superior glenohumeral ligament is performed with an electrocautery introduced from an anterior portal. This was followed by a release of the posterior, inferior, and anterior capsule 5 mm away from the labrum with an electrocautery introduced from the posterior portal while the surgeon is viewing from an anterosuperolateral portal. If still present, the intra articular part of the long head of the biceps tendon undergo either tenotomy or tenodesis. After treatment of any intra-articular pathology, such as loose body removal, attention is turned to the subacromial space.
The lateral and posterolateral gutters are cleared. ny previously placed metal hardware are removed. While the surgeon is viewing from a posterior glenohumeral portal, the tuberoplasty is initiated. The arthroscope is then moved to the subacromial space, and the rotator cuff, if necessary, is sharply elevated from its malunited footprint by use of an electrocautery. Elevation of the rotator cuff consisted of the supraspinatus and anterior half of the infraspinatus, which is the part that overlies the proximally migrated tuberosity (Video).
After elevation of the rotator cuff attachments, a burr is used to perform a tuberoplasty. The cuff is assessed for mobility and integrity and is then retensioned by advancing the cuff laterally on the greater tuberosity and performing a rotator cuff repair. The rotator cuff is advanced and repaired. A modified acromioplasty with a lateral bevel is routinely performed if not done previously.
A.3 Tuberosity Insufficiency
Tuberosity insufficiency can range from contained cystic bony defects within the tuberosity to the absence of the entire tuberosity. Cystic bony defects are often encountered during primary or revision rotator cuff repair. Such defects may be idiopathic, related to a patient's rotator cuff disease, or secondary to osteolysis from breakdown of bioreabsorbable anchors. These osseous defects reduce biological healing capacity and may decrease repair fixation strength. Bone grafting techniques are needed to address these defects.[37]
In such a situation, a simple tendon rotator repair is usually unsuccessful, as a large bony defect significantly lowers the prognosis for primary repair.[38]
One explanation might be that deltoid tension and therefore function is potentiated by the greater tuberosity, also called “deltoid wrapping”.[39]
Therefore, reconstruction of this combined bony and tendon defect may require both tendinous and bony reconstruction. In older patients, such insufficiency is most reliably addressed with reverse shoulder arthroplasty. However, reverse shoulder arthroplasty is not ideal for young patients as multiple studies have demonstrated increased complications in this patient population.[40][41]
Recently, a fresh frozen bony-tendinous allograft of the calcaneus and Achilles tendon has been proposed to address this difficult problem (Video). Long term results and larger series need to confirm this technique.[42]
Surgical Technique
Allograft Reconstruction with Calcaneum and Achilles Tendon for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity (Video). Under general anesthesia and interscalene nerve block, the patient is placed in the beach chair position, with the operative arm draped free. An open anterosuperior incision with a deltoid split is performed in order to expose the greater tuberosity defect. The long head of the biceps was already resected. The remaining posterosuperior rotator cuff was carefully dissected and the proximal humeral head is debrided. The quality of cuff tissue is usually poor (Figure).
The Achilles tendon allograft with attached calcaneus is then prepared (Figure and Video).
The calcaneus is shaped to fill proximal humeral head defect. If necessary, the Achilles tendon is then split longitudinally to decrease its thickness, with the deep layer used to reinforce the rotator cuff repair. Then, the bony portion of the allograft is secured to the humeral head with a 4 mm malleolar screw under fluoroscopic control (Figure).
The native rotator cuff was then repaired onto the bony graft with a combination of an anchor and bone tunnels in the graft. The deep split of Achilles tendon is then sewn into the native posterosuperior rotator cuff to reinforce the repair (Figures and Video).
Two years follow-up confirm bony and tendinous integration (Figures).
Postoperatively, the patient wears an abduction pillow for six weeks and is allowed to perform pendulum exercises. After six weeks the abduction pillow is discontinued and passive mobilization is allowed. Full activity return and strengthening was permitted at three months, with a progressive increase of loads.
Type B: Full Thickness Tendon Lesion
B1: Lateral tendinous disruption
Full thickness disruption of the lateral tendon stump is the most frequent type of rotator cuff lesion, comprising approximately 90.1% of all surgically treated lesions (Table). Tendinous lesions most commonly involve the posterosuperior cuff. Subscapularis tears are nevertheless found in 59% of arthroscopic rotator cuff repairs.41 However, such tears are only full-thickness in 8.7% of cases, and are rarely isolated (Table).
Size of Tendon Lesion
Classifications for tear size include measurement in centimeters or number of tendons involved. This information can be derived from arthroscopy or magnetic resonance imaging and used to offer guidance on treatment and prognosis.[43][44][45][46][47]
Once size is identified and if massive, it can be further classified according to Collin et al.[48]
Tendon Retraction
Patte devised a method of classifying tendon coronal retraction that is often used for research purposes.[49]
The retraction is due to tendon and muscle shortening that are not synchronous after tendon tear.[50]
Substance loss in the later stages of musculotendinous retraction may be because of either active shortening of the tendon substance, suggesting that overreduction and lateral transposition of the tendon over the greater tuberosity may be unphysiological.
Tear Pattern
Full-thickness posterosuperior tears come in a variety of patterns. The most common categories include crescent tears, L and reverse L-shaped tears, and U-shaped tears accounting for respectively 40%, 30% and 15% of posterosuperior rotator cuff lesions.[51]
Recognition of these tear patterns is most useful for anatomic restoration during repair. Crescent tears have good medial to lateral mobility and are amenable to a double-row repair. Longitudinal tears (L and reverse L-shaped tears, and U-shaped tears) have greater mobility in 1 plane and typically require margin convergence to achieve complete repair. Finally, massive contracted tears have also been described. These tears have limited medial to lateral and anterior to posterior mobility and typically require advanced mobilization techniques (i.e. interval slides) to achieve repair.
Releases for the Rotator Cuff
In clinical practice, rotator cuff tears may present with a wide spectrum of size and mobility. Many massive rotator cuff tears may be reparable without releases and, in contrast, some small rotator cuff tears may require releases. Release is only required if tear may not be reduced to the footprint anatomically as it would otherwise unnecessarily increase the complexity of the procedure. Releases may be divided into bursal sided releases, articular sided releases (i.e. capsular release) and interval slides.
Double-Row Versus Single-Row Cuff Repair
Biomechanical testing has consistently demonstrated the superiority of double-row constructs.[52]
Within the domain of level I mid-term and short-term studies, double-row repair (Video) showed significant better UCLA score only (American Shoulder and Elbow Surgeons (ASES), Constant, WORC, and SANE scores showed no significance). This may correlate weakly with the significant lower partial-thickness retear rates of double-row repairs. In contrary, long-term level III studies showed a direct correlation of both functional outcomes and cuff structural integrity, with significant superiority of double-row over single-row repair techniques.[53]
Margin Convergence
Margin convergence to bone can be used in L or V tears. This technique accomplishes margin convergence between the two leaves of the cuff, and at the same time it anchors the cuff to bone, providing very secure fixation. Margin convergence to bone has the mechanical strain reduction advantage of margin convergence coupled with strong fixation to bone. This provides a very secure component to the overall fixation construct.
Load Sharing Rip Stop Construct
Double- row repair is not possible in the setting of medially based tears, lateral tendon loss, or limited tendon mobility. Load sharing rip stop constructs demonstrated improved functional outcomes with reasonable healing rates in an otherwise challenging subset of rotator cuff tears.[54]
This suture technique combines the advantages of a rip stop suture tape and load sharing properties of a double-row repair and has biomechanically superior properties compared to a single-row repair (Figure and Video).[55]

Massive Posterosuperior Rotator Cuff Tears
Prevalence
Massive rotator cuff tears comprise approximately 20% of all cuff tears and 80% of recurrent tears.[56][57]
Definition and Classification of Massive Rotator Cuff Tears
Historically a massive rotator cuff tear has been described as a tear with a diameter of 5 cm or more as described by Cofield or as a complete tear of two or more tendons as described by Gerber (Figure).[58][59]
The former in particular is usually applied at the time of surgery. In an attempt to provide a preoperative MRI-based classification, Davidson et al. defined a massive tear as one with a coronal length and sagittal width greater than or equal to 2 cm.[60]
Unfortunately, these systems are vulnerable to error due to variation in patient size and arm position at the time of measurement. It is more appropriate to define the size of a tear in terms of the amount of tendon that has been detached from the tuberosities. While the Gerber definition helps account for variability in size, there are exceptions to the complete two tendons requirement and this classification does not distinguish different patterns or predict function. Additionally, in using the term “massive”, there is a connotation of difficulty and irreparability. While challenging, most massive rotator cuff tears are reparable and other factors like the tendon retraction, atrophy, arthritis, and mobilization must be considered. Thus, in addition to the number of tendons involved, some authors proposed at least one of the two tendons must be retracted beyond the top of the humeral head (i.e Patte 3 for the supraspinatus in the coronal plane).[61]
Such classification also takes advantage of 3-dimensional information on tear pattern, providing guidance on treatment technique.
Table: Different Classification of Massive Rotator Cuff Tears
Once a massive rotator cuff tear is identified, it can be further classified according to Collin et al. In this subclassification, the rotator cuff is divided into five components: supraspinatus, superior subscapularis, inferior subscapularis, infraspinatus, and teres minor (Figure).
Rotator cuff tear patterns can then be classified into 5 types: type A, supraspinatus and superior subscapularis tears; type B, supraspinatus and entire subscapularis tears; type C, supraspinatus, superior subscapularis, and infraspinatus tears; type D, supraspinatus and infraspinatus tears; and type E, supraspinatus, infraspinatus, and teres minor tears (Figure).[62]

This classification not only subclassifies massive tears but has also been linked to function, particularly the maintenance of active elevation, offering more information than the traditional six sagittal segments of Patte’s classification.
Rotator Cuff Incarceration in the Glenohumeral Joint
Case of a complete rotator cuff tendon avulsion with glenohumeral joint incarceration after significant trauma to the shoulder have been described.[63]

Suprascapular Nerve Neuropathy and Massive Rotator Cuff Tear
Recently there has been growing interest in the relationship between suprascapular neuropathy and massive rotator cuff tears. Theoretically, medial retraction of posterosuperior rotator cuff tears can place excessive traction on the suprascapular nerve.[64]
However, clinical diagnosis is beset with uncertainties as the potential symptoms of suprascapular nerve neuropathy, namely, pain, weakness, and atrophy, are inseparable from those of massive rotator cuff tear. There is actually no support for routine suprascapular nerve release when repair is performed for several reasons. First, it is clearly demonstrated that repair of repair without release leads to satisfactory results. Moreover, the prevalence of suprascapular nerve neuropathy in case of massive rotator cuff tears in a prospective study is low (2%).[65]
Treatment Options for Massive Rotator Cuffs
It should be remembered that nonoperative treatment is successful in many cases. When surgery is indicated, the primary aim is restoration of force couples and anatomic or partial repair of the rotator cuff to its footprint. However, a number of factors (refusal of the patient, biologic factors, characteristics of the tear, etc) can make these goals difficult, impossible, or unwanted to achieve. Fatty infiltration, rotator cuff retraction, and poor tendon compliance are common in patients with massive rotator cuff tears. In these situations, other approaches have been advocated, with varying degrees of success.[66]
These include physical therapy,59,60 subacromial decompression and palliative biceps tenotomy (subacromial debridement),61 muscle transfer,62 and reverse shoulder arthroplasty.63 However, there are no randomized controlled trials comparing these various options and recommendations are mainly based on retrospective case series and the surgeon’s own experiences.[67][68][69][70][71]
Conservative Treatment
Many patients with massive rotator cuff tears respond favorably to nonsurgical treatment. Nevertheless, patients must be aware that despite clinical improvement, future treatment may be impacted by progression of glenohumeral osteoarthritis and fatty infiltration as well as narrowing of the acromiohumeral distance. In a series of 19 patients with massive rotator cuff tears treated nonoperatively the average Constant score was 83% at a mean follow-up of 48 months. However, 50% of “reparable” tears became “irreparable” during this period.[72]
The mainstay of nonoperative treatment includes nonsteroidal anti-inflammatory drugs, subacromial corticosteroid injections, and physical therapy. The protocol of rehabilitation focused habitually on global deltoid reconditioning and periscapular strengthening. Although certain authors proposed that re-education of the anterior deltoid muscle to compensate for a deficient rotator cuff is the cornerstone, we attach more importance to solicitation of stabilizing muscles of the glenohumeral joint with an approach based on exercises in high position. In this position, the deltoid, which acts synergistically with the remaining rotator muscles, has no upward component and participates in the articular coaptation.[73]
In general, nonoperative management is attempted for six months before considering surgery. Younger patients (<60 years of age), however, may be immediate candidates for surgery based on the high risk for progression with conservative treatment. If after six months, symptoms have not improved, the chances of success with further nonoperative treatment decreases and operative treatment may be considered for older patients. It is unclear if it is exercise alone or exercise in combination with other interventions during the recovery process that offers the greatest benefit. In a recent prospective cohort of 45 patients suffering from pseudoparalysis with a radiographically confirmed massive rotator cuff tears, Collin and al. found after a follow-up of 48 months that the mean Constant score improved from 43 to 56 points and the mean forward flexion improved from 76 degrees to more than 160 degrees after completion of the program. They also demonstrated that effectiveness of physical therapy is related to the size and location of the lesion; if the tear involved the posterosuperior rotator cuff (B type), or only two tendons or less, most patients regained active anterior elevation that persisted for 48 months. The anterior rotator cuff is the key of anterior active elevation as only 20% of patients with MRCTs, but an intact subscapularis, develop pseudoparalysis.
Surgical (Operative) Treatment
For older patients surgery is considered when nonoperative treatment fails. Additionally, we often consider surgery as first line treatment in young patients because there is a high rate of progression with conservative treatment and for tears involving the anterior rotator cable since this area is most important to maintenance of forward elevation.
Arthroscopic Rotator Cuff Repair
The approach is to repair all of the rotator cuff that can reasonably be brought back to the tuberosities without excessive tension, and to address all potential causes of persistent pain or factors threatening the repair. The goal of a repair, even if partial, is to restore force couples and to re-establish the “suspension bridge”. In this theory, complete closure of the defect is less important than restoration of a stable fulcrum for normal shoulder kinematics. Although shoulder strength may not improve after this intervention, function is usually enhanced because of relief from pain caused by mechanical impingement. Additionally, although complete healing of massive tears is not always achievable, we believe that partial healing of the cuff may prevent secondary extension of the tear.
The Acromion and Biceps
Complete anterior acromioplasty is not advisable in the setting of a massive tear as it may lead to postoperative anterosuperior migration of the humeral head. The acromiohumeral arch is probably a component of human evolution used to compensate the deficiency of the superior rotator cuff.66 Consequently, when and how should acromioplasty should be perform is still debated.[74]
A tenotomy or tenodesis of the long head of the biceps should be perform in the setting of a massive rotator cuff tear. There is evidence suggesting that the long head of the biceps tendon may be a source of pain and contributes to the discomfort. In a large series, Walch et al. observed an increase in the Constant score from 48.4 preoperatively to 67.6 after arthroscopic biceps tenotomy. At last follow-up, 87% of patients were satisfied or very satisfied with the result. However, the acromiohumeral interval decreased by a mean of 1.3 mm during the follow-up period.[75]
Repair Techniques
Unfortunately, even if reinsertion of the tendon on the bone is achievable, it is often difficult to reliably achieve long-term healing with a structurally intact repair.[76]
In the setting of a massive tear, a double-row repair improves long-term functional outcome.68-70[77][78][79]
However, this should not be performed at the expense of over-tensioning as application of a double-row repair to a tendon with poor tendon length and excursion may lead to medial failure.[80]
Augmentation
Graft augmentation may improve healing in massive rotator cuff tears, but add significant cost and time to the procedure.[81]
The choice of graft is influenced by several factors including mechanical properties, host response and potential for ingrowth. Scaffolds provide mechanical support and have biological properties that may favorably influence cell proliferation and differentiation, hopefully improving tendon-to-bone healing. Currently, scaffolds derived from dermis, small intestinal submucosa, skin, fascia lata, and pericardium have been processed and marketed for augmentation in the repair of massive tears. Biological grafts are preferred, when compared to synthetic grafts, due to the unknown host response to synthetic grafts. An important factor in the longevity and strength of a graft is the amount of ingrowth.
Results of Primary Repairs
Results following arthroscopic repair of massive rotator cuffs have previously been reported.[82][83]
For primary repair, improvements are observed in forward flexion (132 degrees vs 168 degrees), pain (6.3 v 1.3), UCLA score, (15.7 v 30.7) and American Shoulder and Elbow Surgeons score (41.7 v 85.7) (P<.001). A good or excellent outcome is obtained in 78% of cases. Similar results are noticed after repair of type A, B and C massive rotator cuff tears.[84]
After revision repair, mean active forward elevation improves by 15 degrees, from 136.0 degrees ± 51.9 degrees (range, 30 to 180 degrees) at baseline to 151.4 degrees ± 41.5 degrees (range, 30 to 180 degrees) at final follow-up (P=.019). The mean pain score improves by 3.1 points, from 5.0 ± 2.4 points at baseline to 1.9 ± 2.3 points at final follow-up (p<.001). The mean American Shoulder and Elbow Surgeons (ASES) score improves from 45.7 ± 17.8 at baseline to 75.5 ± 20.3 at final follow-up (P<.001). The mean UCLA score also improves, from 16.7 ±4.9 at baseline to 26.4 ± 6.9 at final follow-up (P<.001). According to the UCLA score, functional results are excellent in 15% of cases, good in 35%, fair in 25%, and poor in 25%. Seventy-nine percent of the patients are satisfied, and 32 patients (60%) returned to their previous activities.[85]
Revision Rotator Cuff Repair
Introduction
Failure of tendon healing after rotator cuff repair is common, reported in approximately 20% of cases depending on tear size.[86]
Tear recurrence can be related to various factors such as: 1) inadequate strength of the initial repair construct, 2) biological failure to heal despite strong initial fixation, and 3) inappropriate post-operative rehabilitation causing structural failure of the repair.[87][88][89][90]
While functional outcome has been correlated with postoperative rotator cuff integrity78 many patients maintain a satisfactory outcome despite structural failure.[91]
The ideal treatment for a recurrent tear is thus not completely defined.
Initial Radiological Findings
The goal of imaging studies is to confirm the site of the recurrent tear. Trantalis et al. reported five patients with retearing of the cuff after double-row rotator cuff repair. All five patients had retearing medial to the medial row if sutures were placed near the musculotendinous junction of the supraspinatus.[92]
Hayashida et al. observed that the prevalence of complete retearing of the tendon after a double-row rotator cuff repair is similar around the medial anchors with a well-preserved footprint.[93]
Another point of interest is the quality of the tendon.[94]
A significant and growing number of rotator cuff repairs are performed in individuals with poor rotator cuff tissue quality. Djurasovic reported an incidence of 30% (24 on 80) of poor rotator cuff tissue quality (graded subjectively at the time of surgery).[95]
At the same time, the muscle undergoes intrinsic degeneration. After a retear, Deniz et al. found that fatty infiltration and atrophy continued to worsen significantly.[96]
However, fatty infiltration of the supraspinatus does not seem to be a determinant factor in tendon healing. Park et al. did not find significant relationship between preoperative supraspinatus fatty infiltration and postoperative tendon healing. Contrarily, it seems that fatty infiltration of infraspinatus and subscapularis are highly significant factors (P<.001).[97]
Another point is the bone quality. Oh et al. demonstrated that bone mineral density within the greater tuberosity decreases in patients with rotator cuff tears. In another retrospective study that investigated the relationship between greater tuberosity osteopenia and chronicity of rotator cuff tears, Cadet et al. found that there were significantly greater osteopenic changes in the greater tuberosity in patients with chronic retracted rotator cuff tears.[98]
However, this localized osteoporosis may not influence tendon healing. In a recent study, Park et al. did not observe after primary repair that bone mineral density influenced final results.[99]
Nevertheless, the greater tuberosity in revision cases can also be deficient due to anchor removal or perianchor cyst formation. Kim et al. observed in a retrospective case series of two hundred and nine patients bone cyst formation in 97 instances (46.4%), and these authors questioned the utility of bioabsorbable anchors because of possible interference with revision surgery. Consequent bone lysis can be noticed after trauma. Lädermann et al. reported massive bone resorption after osteosynthesis of the greater tuberosity leading to combined tendon and bony insufficiency and pseudoparalysis/pseudoparesis.
When milestones of typical post-operative recovery are not met, analysis of rotator cuff repair should be considered and a multi-modal evaluation is required. The goal of imaging studies is to confirm the site of the recurrent tear (Figure)86,92 the type of failure (e.g. in continuity), and if possible, it’s cause.[100][101][102] File:Sensitive-content.pngal, or perianchor cyst formation and (F) bony and tendinous insufficiency. Reproduced from Lädermann et al., with permission. Other points of interest are the quality of the bone (tuberosity deficiency), tendon, and muscle, and whether further surgery is feasible.[103][104]
Standard shoulder radiographs, including anteroposterior, axillary lateral and scapular Y (outlet) views, may demonstrate decreased acromiohumeral distance, glenohumeral arthritis, subacromial spurs, acetabularization of the acromion, femoralization of the humeral head, and implant or anchor migration.[105][106]
It can also be used to rule out chondrolysis, anchor migration or prominence, and acromial fracture. Among evaluation techniques, the most widely accepted reference standard is magnetic resonance imaging which allows visualization of the tendons and does not involve radiation exposure. Intra-articular contrast may be used in association with magnetic resonance imaging to increase the sensitivity for detecting a recurrent tear.[107]
Postoperative magnetic resonance imaging images are difficult to interpret; inadequate coverage of the greater or lesser tuberosity may indicate partial healing and not a recurrent full-thickness tear.[108][109][110]
Furthermore, only 10% of re-attached tendons generate a normal magnetic resonance imaging signal. Thus, a common finding is the presence of an intermediate signal within the tendon indicating granulation tissue or of a low-intensity signal produced by fibrous tissue.[111][112]
These signal changes may persist for longer than six months, due to tissue remodeling, and seem to have no clinical implications.[113][114]
Finally, the evaluation of magnetic resonance imaging scans is made difficult by the normal leakage of fluid into the subacromial space after the opening of the rotator interval and passage of instruments through the tendon, which may contain artifacts generated, for instance, by metal anchors or high-strength sutures. These factors, together with the high cost of magnetic resonance imaging, lend considerable appeal to ultrasound as a method for evaluating rotator cuff repair, even if its effectiveness is operator-dependent.[115]
Computed tomography arthrogram can also be used to aid in the identification of recurrent rotator cuff tears when neither ultrasound or magnetic resonance imaging are options.[116]
Failure after rotator cuff repair was previously believed to occur during the first three months.[117][118]
While the majority of retears do occur within the first three months, it has now been demonstrated retears can occur up to six months after repair.[119][120][121]
Recent prospective studies have confirmed that ultrasound has a high sensitivity and specificity for detecting a recurrent rotator cuff tear compared to magnetic resonance imaging.In a study comparing magnetic resonance imaging and ultrasound after rotator cuff repair, Codsi et al. found 92% agreement with a coefficient of 0.70.[122]
Similarly, Collin et al. reported that ultrasound had 80% sensitivity and 98% specificity compared to magnetic resonance imaging.[123]
Treatment
Non Surgical (Conservative) Treatment of Failed Rotator Cuff Repair
Jost et al. evaluated 20 patients with a failed rotator cuff repair at a mean follow-up of 38 months and reported that the adjusted Constant score and shoulder simple value averaged 83% and 75%, respectively.[124]
Namdari et al. demonstrated a successful outcome in 54% of patients (defined by an American Shoulder and Elbow Surgeons score of more than 80 points) and a mean 15 point improvement in the American Shoulder and Elbow Surgeons score at a mean of 52 months postoperative. Finally, the same group compared the two and ten year results for patients with known structural failures of rotator cuff repair. The average long-term American Shoulder and Elbow Surgeons score was 79 points (range, 50 to 95 points) and the average visual analog scale pain score was 2.2 points (range, 1 to 4 points); both scores were unchanged from those at two years. The average simple shoulder test score was 9.2 points (range, 6 to 12 points), and the average age-adjusted Constant score was 73 points (range, 59 to 90 points).[125]
Surgical (Operative) Treatment Revision Rotator Cuff Repair
Surgical Technique
The alarming retear rate indicates that several surgical options can be considered which must be individualized to the patient. For example, in the setting of an acute traumatic retear in a physiologically young, healthy, active and non-pseudoparalytic patient, arthroscopic revision surgery is generally recommended. Techniques to enhance mechanical fixation, such as linked load-sharing rip-stop constructs should be considered.[126]
Augmented repair using scaffold devices derived from autografts,46,119,120 allograft,121 xenograft extracellular matrix122 or synthetic matrices such as poly-l-lactide grafts123 have been used to offer a structural support of the repair during the crucial healing period and to improve healing rates. The scientific literature does not contain enough data to justify any systematic associated augmentation techniques. Tendon transfers may be used in patients without advanced glenohumeral arthritis who have significant loss of external rotation strength and maintain anterior active elevation.62,124 If the patient is young, pseudoparalytic and suffers from a combined bony and tendinous rotator cuff insufficiency, calcaneum and Achilles tendon allograft could be considered.40
Finally, whereas primary pseudoparalysis responds well to arthroscopic rotator cuff repair, persistent pseudoparalysis after a previous attempt at rotator cuff repair may be more predictably managed with reverse shoulder arthroplasty. Denard et al. reported that pseudoparalysis/pseudoparesis was reversed in the revision setting in only 43% of patients with a low rate (54%) of satisfaction.[127]
In contrast, Boileau et al. found that anterior elevation was reliably restored with reverse shoulder arthroplasty after failed rotator cuff repair and 73% of patients were satisfied.[128]
Clinical and Radiological Results After Revision Rotator Cuff Repair
The clinical results of are summarized in the Table. Overall, range of motion improved, except in one series of open rotator cuff repair.94 Functional outcome improved in all series and 70% or more of patients were satisfied or very satisfied.[129]
Table: Clinical Results of Revision RCR
Complication
The short- to intermediate-term incidence of complications, including subsequent revision surgery, after revision rotator cuff repair is relatively low, around ten percent in this review (Table). However, most studies primarily considered reoperation a complication and did not examine complications such as hematoma, hardware failure, and postoperative stiffness. The prevalence of postoperative complications is therefore probably higher than reported. The prevalence of non-healing or retear was around 40% (range, 0 to 62%) in the four studies with postoperative imaging.[130][131][132][133]
Furthermore, these tears may progress with time; Shamsudin et al. reported a prevalence of defect of 28% at six months and of 40% at two years. If revision is planned, patients have to be aware of the high prevalence of persistent structural defect. Moreover, retear rate after reoperation continues to deteriorate with time.[134][135]
Structural failure does not always result in clinical failure. Many patients with partial healing of the cuff and a residual defect will be much improved after surgery. Characteristics associated with successful and unsuccessful results after structural failure of rotator cuff repair are poorly understood. Retear or non-healing of tendons is rather frequent and surgery is rarely proposed because this condition is often well tolerated with marked clinical improvement in comparison with the preoperative state.[136]
One reason for clinical failure is probably the non-restoration of balanced force couples and the suspension bridge system of force transmission in the shoulder. The location (involvement of the subscapularis on which the rotator cable is attached) and the size (more than two tendons) are the primary determinant of rotator cuff function.
Risk Factors for Postoperative Poorer Results
Several patient-related factors appear to be associated with poorer results. The most important factor seems to be poor preoperative range of motion. Female sex and, in one study, if the surgery was performed on the dominant arm, were negatively associated with postoperative outcome.[137][138][139]
There is still controversy about certain risk factors such as age of patients. Disease-related factors included patients with a recurrent tear after the revision repair, preoperative visual analogue scale pain score greater than five, and poor preoperative range of motion. The range vary from less than 90 degrees in the studies from Denard et al. and Piasecki et al. to 140 degrees in the study of Chuang et al.[140][141][142]
The latter factor has been reported in almost all series and is probably the most important preoperative indicator. In addition, acromiohumeral distance (less than seven mm) can be associated with a satisfactory outcome.[143]
There is controversy about patients with more than one prior surgery, with one study reporting that this negatively impacted results and another study reporting that it did not.[144][145]
Operative-related factors like poor tendon quality54,88 is associated with poorer results.[146][147]
One study compared outcomes between massive and non-massive tears and did not find any significant difference in terms of post-operative anterior elevation, pain, or functional outcome.[148]
Post-revision Rehabilitation
In all studies, subjects took part in standardized rehabilitation protocols. Most studies did not allow immediate overhead passive motion. Most studies recommend sling during 6 weeks. Strengthening is delayed until six to sixteen weeks post-operatively. Full return to activity was not allowed until four to twelve months.
B2: Medial Tendinous Disruption
Disruption of the tendon medial to an intact lateral tendon stump has been reported in primary chronic and acute cases or postoperatively as a failure medial to the medial row.[149][150]
Regarding the former, it is now understood that the infraspinatus insertion is quite broad and wraps around from posterior to anterior to occupy much of the lateral greater tuberosity. Therefore, such descriptions of a lateral tendon stump remaining may, in fact, represent a torn supraspinatus with an intact infraspinatus.
Full thickness defects medial to an intact footprint of the rotator cuff can be seen following a rotator cuff repair (Figure). Trantalis et al. described 5 patients with medial failure following a double-row rotator cuff repair. Such failure results from overtensioning during repair and is very difficult to manage with revision repair. These lesions do not produce muscular edema, except in traumatic cases with important and acute retraction of the muscle and the remnant of the tendon (Figure); its origin is then either retraction (which may appear in some hours) or neurological lesions (noted after some weeks).[151]
B3: Tendon to Tendon Adhesion: “Fosbury Flop Tear”
The Fosbury flop tear occurs from a full thickness tear that has flipped upon itself and adhered medially (Figure).[152]
Prevalence
In a prospective study spanning one-year, Lädermann et al. reported five patients with full or partial-thickness rotator cuff lesions in a series of 97 (5 % incidence rate).142 Radiologically, these lesions showed a thicker than normal tendon stump on the bursal-side of the retracted supraspinatus tendon in a superomedial orientation.[153]

Additionally, patients with this lesion were also found to have an accumulation of fluid in the superomedial part of the subacromial bursa as well as adhesions between the wall of the subacromial bursa and the tendon of the supraspinatus. Since the original description, another group verified the same entity.[154]
Surgical Technique
A diagnostic arthroscopy is performed with an arthroscopic pump maintaining pressure at 50 mm Hg. The biceps is tenotomized or tenodesed. Attention is then turned to the posterosuperior rotator cuff (supraspinatus and infraspinatus tendons). The appearances of the tears are unusual with ulcerations on the bursal surface (anemone like) and what initially appeared to be a thickened lateral tendon stump (Figure and Video).

After a progressive dissection, however, medial adhesions of the bursal layer is found. A complete excavation of the rotator cuff must be performed by skeletonizing the scapular spine medially, removing any bursal leaders (false insertions into the internal deltoid fascia) laterally, and debriding the fibrofatty bursa overlying the rotator cuff. These steps allow identification of the lateral tendon stump which is reversed upon itself and scarred medially. Once identified the tendon stump is unfolded (Video) and subsequently repaired to the lateral bone bed.
B4: Tendon to Acromion Adhesion
Disruption of the lateral tendon stump can be followed by adhesion under the acromion, the coracoid process or the coracoacromial arch (Figure). These adhesions are most pronounced in revision situations, but may also be observed in primary cases, particularly in the setting of a massive contracted rotator cuff tear.[155]

Type C: Musculotendinous Junction Lesion
Isolated ruptures of the musculotendinous junction are rare in the rotator cuff, but have a dramatic impact on functional outcome. Such lesions have been observed in all muscles of the rotator cuff, affecting the infraspinatus muscle in half of cases, followed by the supraspinatus in 31% of cases, the subscapularis in 25%, and the teres minor in 19% of cases (more than one muscle is occasionally involved).[156]
These lesions can been classified into 3 stages. Grade I injuries are a muscular strain that heals without adverse sequelae. Grade II injuries are partial ruptures without tendon retraction. Grade III injuries are complete ruptures at the musculotendinous junction.146 The acute phase of these injuries are associated with severe inflammation, leading to a highly characteristic bright signal on T2 weighted magnetic resonance imaging (Figure).[157]
Edema of rotator cuff muscle with an intact tendon-bone insertion is infrequent. It has been described in cases of denervation, such as compression of the suprascapular nerve, Parsonage Turner syndrome, in other rare and non-specific conditions.[158][159]
Complete musculotendinous junction ruptures have only been described in the infraspinatus and the supraspinatus.[160][161][162]
Possible causes for musculotendinous junction infraspinatus lesion are calcific tendinitis or previous cortisone injection. On the other hand, rupture of the other muscles seem to be due to trauma or inlet impingement syndrome. There is little information about the clinical results of grade 3 musculotendinous junction lesions.
Type C with Reverse Fosbury Flop Tear
Exceptionally, a lesion of the musculotendinous junction can develop a Fosbury pattern and heals, for its tendon part, on the humerus or even coracoid process.[163]

Type D: Muscle Insufficiency
D1: Fatty Infiltration and Muscle Atrophy
One of the most important prognostic factor for rotator cuff repair is nonfunctional muscle bellies. Muscle quality is most commonly classified according to Goutallier et al. to determine the extent of injuries based upon the degree in which fat is present in the muscle. They proposed a 5 stage classification system of fatty infiltration. Additionally, they demonstrated that multiple muscles develop fatty degeneration, even if they were not directly impacted by the original lesion.[164]
With the advent of MRI, however, the classification was extrapolated to the most lateral parasagittal image on which the scapular spine was in contact with the scapular body (Y view).[165]
The mean time to tendon rupture observed for stage 2 fatty infiltration is 3 years for the supraspinatus and 2.5 years for the infraspinatus and the subscapularis when their tendons ruptured. The mean time observed to grade 3 and 4 fatty infiltration is 5, 4, and 3 years for the supraspinatus, the infraspinatus, and the subscapularis, respectively.[166]
Zanetti et al. described a radiographic tangent sign to quickly and reliably assess the presence or absence of supraspinatus atrophy on MRI. This sign is a reliable method for evaluating the presence or absence of muscle atrophy using the sagittal plane and is moreover significantly related to the level of fatty infiltration within the supraspinatus muscle.[167]
It has been reported to be a predictor of whether a rotator cuff tear will be repairable.[168]
Thomazeau et al. proposed calculating the occupation ratio of the supraspinatus muscle belly using MRI. This was calculating by comparing the supraspinatus fossa volume to total supraspinatus muscle belly volume and computing the ratio. This ratio was found to be significantly decreased in patients with repairable rotator cuff tears.[169]
Inability to obtain a complete repair of the supraspinatus was associated with a positive tangent sign (30% irreparable) versus a negative tangent sign (6.3% irreparable, OR = 6,3, P =0.0102) and with Goutallier grade 3-4 fatty infiltration of the supraspinatus (42.9% irreparable) versus grade 0-2 fatty infiltration (5.7% irreparable, OR = 11.8, P =0.001).[170]
Rotator cuff repair should thus be performed before the appearance of fatty infiltration (Stage 2) and atrophy (positive tangent sign) and as soon as possible in older patients when the tear involves multiple tendons.[171]
D2: Neurological impairment
Isolated suprascapular nerve neuropathy is a condition associated with acute and chronic shoulder girdle traction injuries, compressive lesions such as paralabral cysts and compressive ligaments, as well as large or massive rotator cuff tears (Figure). In the latter situation, the proposed mechanism involves traction of the nerve caused by retraction of the supraspinatus against its fixed points on the suprascapular and spinoglenoid notches. However, clinical diagnosis is beset with uncertainties as the potential symptoms of suprascapular nerve neuropathy, namely, pain, weakness, and atrophy, are inseparable from those of rotator cuff tear. Currently, there is no support for routine suprascapular nerve release as the prevalence of suprascapular nerve neuropathy in the setting of a massive rotator cuff tear was very low (2%) in a recent prospective study.[172]
D3: Tumors
Numerous tumors, such as an arthrosynovial cyst, intramuscular lipoma, or a calcified hematoma, can developed at the expense of the muscular tissue and cause muscular insufficiency (Figure).[173]
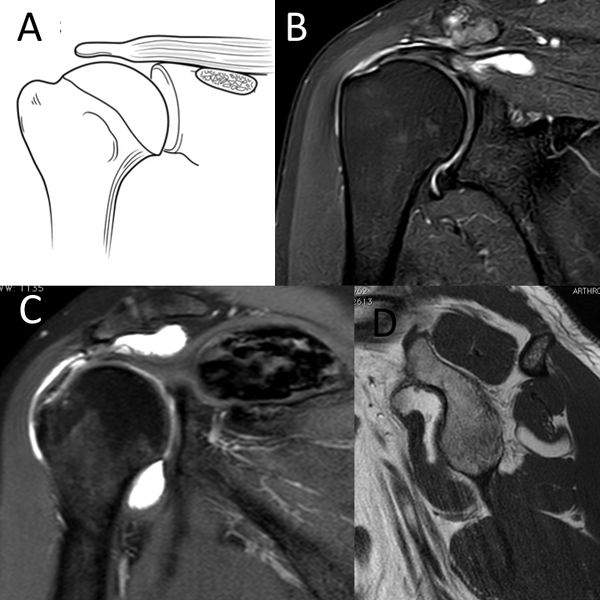
C) Coronal T2-weighted PD D) sagittal T1-weighted image demonstrating D3 rotator cuff lesion with a calcified hematoma in the supraspinatus and an intramuscular lipoma of the subscapularis, respectively. Reproduced from Lädermann et al., with permission.
These impairments can be as isolated or be associated with other rotator cuff lesions. Management may require treatment of the associated mechanical stress in addition to rotator cuff repair.
Irreparable Rotator Cuff Tears
Introduction
One of the most challenging issues in shoulder surgery is the management of symptomatic irreparable rotator cuff tears. The literature reports that 12% of posterosuperior rotator cuff tear are not repairable.[174]
The latter condition when symptomatic can be managed with several approaches without clear evidence based guidelines. For example, the same patient with a D type irreparable rotator cuff tears according to Collin et al. may be offered physiotherapy, partial repair, tendon transfer, superior capsular reconstruction, subacromial spacer (balloon), or even a reverse shoulder arthroplasty (RSA) depending on multiple factors, including, geography, surgeon experience, implants costs, etc. Moreover, even if it is reported that these surgical procedures have different indications, they are often applied to patients with similar problems indiscriminately.
Definition of an Irreparable Rotator Cuff Tears & Clinical and Imaging Findings
The definition of an irreparable rotator cuff varies widely. Furthermore, with advances in anchors, suture strength, techniques of release and repair with load-sharing rip-stop fixation, etc, the definition continues to evolve. Two situations can be faced; the first one consists of a patient who has a contra-indication to cuff repair, and the second scenario is intra-operative when a complete repair is not physically possible. While most rotator cuff tears can be repaired, some lesions are not reparable or should not be repaired. Imaging studies play a critical role in preoperative assessment, evaluation of the defects and selection of the correct treatment for an irreparable rotator cuff tears. The following clinical and radiological preoperative factors that have been clearly associated with postoperative clinical or radiological failure should be considered before attempting repair.
Clinical Examination
Pseudoparalysis was defined as a chronic inability to actively elevate the arm beyond 90 degrees with full passive forward flexion.[175]
It is nevertheless important to note that this correspond to functional limitation associated or not with an antero-superior escape and not just to pain inhibition. Several studies purport to reverse pseudoparalysis although it represents mainly pseudoparesis cases. When pain inhibition or slight stiffness limits the patient from elevating the shoulder, the limited motion is not secondary to complete cuff deficiency.[176]
Anatomically, pseudoparalysis requires the disruption of at least of rotator cable attachment which in the study of Collin et al. was found in only 2.9% of massive D-type cases. This means that pseudoparalysis of the posterosuperior rotator cuff cases involved usually the whole posterior cuff (33.3% of pseudoparalysis found in E-type irreparable rotator cuff tears).[177]
In addition to pseudoparalysis, the presence of lag signs (external rotation lag, drop, dropping, hornblower signs) is also associated with non-reparability.[178]
Treatment
Non-Surgical (Conservative) Treatment
As patients with posterosuperior irreparable rotator cuff tears do not have anterosuperior escape, many respond favorably to nonsurgical treatment which should be attempted for six months before considering surgery. If after this adequate period of time symptoms have not improved, the chances of success with further non-operative treatment decreases and operative treatment may be considered. The mainstay of non-operative treatment includes nonsteroidal anti-inflammatory drugs, subacromial corticosteroid injections, and physical therapy. Levy et al. prospectively assessed 17 patients with clinically and radiographically diagnosed irreparable rotator cuff tears that underwent an anterior deltoid training program.[179]
By 9 months, the mean Constant score improved from 26 to 63, and the forward flexion improved from 40° to 160°. In another prospective cohort of 45 patients suffering from pseudoparalysis with a radiographically confirmed D-type rotator cuff tear, Collin et al. found after a follow-up of 48 months that 14 of 15 patients had substantial improvement in active forward elevation to above 90 degrees.[180]
The protocol of rehabilitation focused habitually on a multimodal physical therapy program with global deltoid reconditioning and periscapular strengthening.[181]
Certain authors propose that reeducation of the anterior deltoid muscle to compensate for a deficient rotator cuff is the cornerstone of successful non-operative treatment.[182]
The promising results has nevertheless not been confirmed.[183][184]
Surgical (Operative) Treatment
In the absence of a gold standard surgical solution, treatment of irreparable rotator cuff tears has proven to be quite challenging, adding to the surgeon’s dilemma regarding the choice of patient and treatment option. Younger active patients (<60 years of age) with traumatic tears, may be immediate candidates for surgery based on the high risk for progression with conservative treatment. Surgical approaches have been advocated, with varying degrees of success. The surgical options include arthroscopic debridement, partial repair, biceps procedure, superior capsular reconstruction, muscle transfers, biodegradable subacromial spacer interposition, biological augmentation and reverse shoulder arthroplasty. Despite all these options, irreparable rotator cuff tears are difficult to manage and treat effectively. There are no high levels of evidence prospective trials comparing these various options and therefore recommendations are mainly based on retrospective case series, surgeon experiences, and expert opinions.
Long Head of the Biceps Tenotomy or Tenodesis +/- Partial Repair
This procedure includes biceps tenotomy or tenodesis, partial repair if evaluation has deemed the remaining tendon to be of good quality, and associated procedures such as distal clavicle resection if necessary. Tenotomy or tenodesis of the long head of the biceps should consistently be performed, as biceps tendinopathy is observed in 92% of rotator cuff lesions.[185]
There is evidence suggesting that this structure is a source of pain and contributes to the symptomatology of patients with irreparable rotator cuff tears. Walch et al. reported statistically significant improvements in the Constant score with an isolated biceps tenotomy (Constant score 48 points preoperatively to 68 points at follow-up (P < .0001)) which has been confirmed by numerous authors.[186]
The aim of this procedure is to repair all of the rotator cuff tendon that can reasonably be brought back to the tuberosities without excessive tension, and to address all potential causes of persistent pain or factors threatening the repair. The goal of a partial repair is to restore force couples, to re-establish the “suspension bridge”, and to prevent secondary extension of the tear. In this theory, complete closure of the defect is less important than restoration of a stable fulcrum for normal shoulder kinematics. Although having little effect on improvement in shoulder strength after this intervention, eliminating various pain generators usually enhances function. Although a partial cuff repair is conducted, the role of the biceps tenotomy should not be overlooked in the patient improvements observed.[187]
Acromioplasty is not advisable in the setting of an irreparable rotator cuff tears as it may lead to postoperative antero-superior migration of the humeral head. Tuberoplasty has been proposed as an alternative to classic subacromial decompression in order to preserve the integrity of the coracoacromial arch.[188]
Although the results in compensated tears and low-demand patients are promising,176 it is currently unknown if the positive effect with regards to pain relief is due to the tuberoplasty or to the concomitant performed bursectomy, synovectomy and biceps treatment. Partial repair provides good clinical outcomes, comparable to those reported with biceps sacrifice and subacromial decompression. The main purported benefit of repairing part of the cuff is its potential to slow or halt further tear progression and to increase the strength of the shoulder. All series of partial repair reported a significant improvement in functional scores, while reporting a rate of radiological repair failure around 50% (Table).[189][190][191][192][193][194][195][196]
Long-term benefit in prevention of head migration has not been demonstrated.
Table: Results of partial repair of irreparable rotator cuff tear.
Tendon Transfer
Tendon transfers have been described in the management of an irreparable rotator cuff tears, however, the outcomes reported have been inconsistent. The results of new transfers involving the lower trapezius transfers have not been well described with mainly anatomical or biomechanical data and will not be described in this review article. L'Episcopo and latissimus dorsi transfer are reported to reconstitute the posterior force couple. L’Episcopo first described the technique of transfer of the latissimus dorsi and teres major tendons in children with obstetric palsy.[197]
The procedure involves transferring both tendons laterally and posteriorly on the humerus, such that the function of the transfer changes from internal to external rotation. Boileau et al. analyzed recently 26 patients (2 with glenohumeral arthritis) and found a gain in active external rotation of 26 degrees and an improvement in adjusted Constant score from 63.6% to 86.9% (P < .001).[198]
The integrity of the remaining internal rotators are of utmost importance as patients after a L’Episcopo transfer loose significant internal rotation and may not reach the back anymore. Latissimus dorsi transfer has been initially proposed for irreparable rotator cuff tears as an open procedure to improve control of external rotation in young and high demand patients with an intact subscapularis.[199]
Namdari et al. in a review found that patients followed for mean of 46 months had a mean adjusted Constant score of 46 preoperatively compared with 73 postoperatively (p < 0.001). The mean active external rotation improved from 17 degrees to 27 degrees which is statistically significant (p < 0.001) but not clinically significant. As proposed by Gerber, isolated latissimus dorsi transfer with or without reverse shoulder arthroplasty is mainly to "restore control of external rotation in selected patients" rather than active external rotation itself.[200]
It is also important to keep in mind that the results of the open technique are superior in case of an intact or repairable subscapularis and a hypertrophic teres minor.[201][202]
In other words, latissimus dorsi transfer in D-types irreparable rotator cuff tears is efficient but only indicated in selected patients having an isolated loss of external rotation, a preserved forward elevation above 90°, an intact or repairable subscapularis an ideally a hypertrophic teres minor. Conversely, latissimus dorsi transfer gives unpredictable results in E-type latissimus dorsi transfer and potentially a L’Episcopo transfer is superior in those cases. Recently, indications and techniques have evolved and arthroscopic procedures have been proposed to hopefully limit humeral head upper migration and to restore anterior active elevation.[203]
The same group has observed in a prospective series of 25 patients with a follow-up of 12 months an improvement in mean Constant score from 44 points preoperatively to 65 postoperatively, a slight improvement (10 degrees) in external rotation but a radiological failure rate of 43%.[204]
Posterior rotator cuff insufficiency
Currently, the most commonly used transfer for an irreparable type D or E massive rotator cuff tears is latissimus dorsi transfer. The ideal candidate is a patient who has maintained active anterior elevation, but lacks control of the arm in space in external rotation (simple weakness in external rotation is not a sufficient indication for surgery), and who also has an intact subscapularis and no glenohumeral arthritis. Results are disappointing in patients with subscapularis insufficiency. In addition, results have been disappointing in the setting of preoperative teres minor tears or atrophy. Gerber et al. reported long-term results at a mean of 147 months. The mean simple shoulder value (SSV) in 46 shoulders increased from 29% preoperatively to 70%, the relative Constant score improved from 56% to 80%, and the pain score improved from 7 to 13 points (p < 0.0001 for all).[205]
However, there is no proof that latissimus dorsi transfer gives better long-term results than a simple partial rotator cuff repair. Effectively, 60% of type E massive rotator cuff tears do not lose control of the arm in external rotation. Consequently and despite large series recently published, indications for this type of surgery are rare.[206]
Superior Capsular Reconstruction
Superior capsular reconstruction with either fascia lata autograft, dermal allograft patch or long head of the biceps is a solution that could prevent superior humeral head migration and restore the shoulder muscle force couples (Video of Superior Capsular Reconstruction with Long Head of the Biceps "The Chinese Way").[207][208][209]
The superior capsule is believed to be important in maintaining humeral head depression and compensating for the dynamic effect of the rotator cuff muscles. However, the superior capsule is an inconsistent structure constituted by a confluence a various ligaments, that is in continuity in only 27% of the cases (Video that shows an L-shape left rotator cuff lesion with an intact superior capsule).[210]
No articles reported on the mid- or longer-term clinical and radiological results. Mihata et al. in a small series of 23 patients using fascia lata autograft found at a mean follow-up of 34 months an increased in forward flexion from 84° to 148° (P < .001) and external rotation increased from 26° to 40° (P < .01). Twenty patients (83%) at most recent follow-up had an intact graft without retear.[211]
Denard et al. reported in a series of 59 patients using a dermal allograft with a minimum follow-up of 1 year an increase in forward flexion from 130 degrees preoperative to 158 degrees postoperative, an improvement in American Shoulder and Elbow Surgeons (ASES) score from 44 to 78 and a 55% failure rate. In all cases, a biceps tenotomy or tenodesis was performed.[212]
Subacromial Balloon Interposition
The biodegradable spacer (balloon shape) is arthroscopically implanted between the acromion and the humeral head. The subacromial spacer has been designed to create a physical barrier between tissues in the subacromial space and keep the humeral head depressed when the rotator cuff is not efficient to facilitate deltoid action, thus permitting improvement in glenohumeral joint motion with significant pain reduction. At 5 years follow-up, a recent study on the subacromial spacer with an associated biceps tenotomy reported that 85% of the patients showed a clinically significant improvement of at least 15 points in Constant score, while 62% showed at least 25 points of improvement.[213]
Deranlot et al. described in a series of 37 patients (39 shoulders) a significant improvement of the Constant score from 45 preoperatively to 76 at a mean of 33 months follow-up. In their study, 92% of the shoulders also underwent a long head of biceps tenotomy.[214]
Biological Augmentation
These techniques involve using a graft (allo, auto, or xeno) or synthetic patch to bridge the defect in the rotator cuff and improve connection of the tendon remnant at least at the border of the original footprint. During this procedure, the torn rotator cuff tendons are released, mobilized, and undergo a partial repair. The graft is then sutured on top of the residual defect between the lateral margin of the medial fixed rotator cuff tendon and its native insertion site on the lateral footprint and humerus. A systematic review confirm that this approach improved function with a high rate of structural integrity rates on MRI at 12-month minimum follow-up.[215]
Reverse Shoulder Arthroplasty
Reverse shoulder arthroplasty has emerged as a treatment for irreparable rotator cuff tears. Two recent systematic reviews confirmed that this is a reliable procedure to improve mobility and strength, producing an improvement in pain and postoperative outcome scores.[216][217]
Moreover, reverse shoulder arthroplasty yielded benefits considered cost-effective when compared with other treatments, especially in elderly patients with irreparable rotator cuff tears.[218]
Reverse shoulder arthroplasty should be considered in older patients for whom long period of immobilization and rehabilitation is undesirable.[219]
Even if the rate of complications was high in the two above mentioned systematic reviews, a dramatic decrease has been observed with new designs and better techniques.[220]
Recently, the complication rate has been reported to be lower. However, caution should still be exercised when offering reverse shoulder arthroplasty to young patient that are often disappointed by the results.[221][222]
Conclusion
Various surgeries are proposed for similar posterosuperior irreparable rotator cuff tears and preoperative patient' clinical evaluation. There is no panacea for primary treatment and patients must be aware, in case of palliative or non-prosthetic option, of an alarming rate of structural failure (around 50%) in the short term (Table).
Table: Results of the different techniques of irreparable rotator cuff tear treatment from representative series
The initial use of complex and expensive techniques in management of posterosuperior irreparable rotator cuff tears is actually not supported. Further prospective and comparative studies with large cohort populations and long-term follow-up are necessary to establish effectiveness of expensive or complicated procedures such as SCR, biological augmentation or subacromial spacer as reliable and useful alternative treatment for irreparable rotator cuff tears.
What would Codman have thought about this?
Rupture of the supraspinatus tendon
CHAPTER V
Now that we have considered the shoulder from the anatomic and pathologic points of view, we come to the clinical study of the lesions which may be identified by special groups of symptoms as definite entities. It seems to me that the practice of medicine might be greatly simplified if an official list of clinical entities was constantly maintained by some great medical association. Our literature and our methods of medical education are greatly hampered by synonyms. McCarthy has recently pointed out in Surg. Gyn. and Obst., February, 1932, that there is great need for such a list of malignant conditions. Pathologic entities and clinical entities are not the same. Clinical entities are the practical working diagnoses on which rational treatment may be based. I feel that the Registry of Bone Sarcoma has served such a purpose so far as the nomenclature of bone tumors is concerned, and that this fact alone has done much to crystallize our working knowledge of the diagnoses and treatment of bone lesions. I shall try in this book to make a. similar list of the lesions of the shoulder which have such distinctive characters that they may be recognized clinically and given appropriate treatment. For instance, I recognize as significant clinical entities, complete rupture of the supraspinatus tendon, partial rupture of the supraspinatus tendon, calcified deposits in the tendons of the short rotators, and tendinitis of the short rotators; and I do not recognize muscular rheumatism, neuritis, or idiopathic monarticular arthritis of the shoulder, as entities of sufficient clinical frequency or importance to make them demand special forms of treatment, although these terms are much more frequently used as diagnoses on which physicians base their therapeutics. If an official list existed I would ask to have my new entities added and the old ones at least put in small type. The reader is referred to the Index.
Click for large image
CHART I
Excluding obvious diagnoses such as tumors, fractures and dislocations, most painful shoulders may be classed under the four diagnoses indicated in large type, although each entity merges into the two which adjoin it. For example, calcified deposits are probably a product of tendinitis, but if large in amount, they alter the clinical picture, both in prognosis and in the character of treatment required. If the deposits are very small, they may be negligible, and the clinical picture be that of a "frozen shoulder" due to tendinitis, lendinitis may also be confused with its other neighbor, because a "rim rent" may precipitate the inflammation which results in the frozen shoulder. In a similar way the line between partial and complete ruptures is difficult to draw; e.g., some cases of partial ruptures do not show much restriction of motion. Even complete ruptures may be confused with calcified deposits, as in Case 76, where the tendon was torn through a partially calcified area. Pathologically, too, there is some reason to believe that calcified deposits may be caused originally by small ruptures, and that the defects left after the deposits have disappeared may later lead to rupture. Nevertheless, although these entities are difficult to separate in borderline cases, typical instances are very clearly distinguished for purposes of treatment as well as in prognosis. There are also suggestive variations in sex, age, and occupation among the patients subject to these conditions.
This chapter discusses the most serious of these entities. As far as I know, I was the first writer to call attention to this lesion, and it seems to me that I can best introduce the rest of the book by reprinting here my first article, so that we may thus start at the beginning, so far as the history of this particular entity is concerned.
Reprinted from the Boston Medical and Surgical Journal, Vol. clxiv, No. 20, pp. 708-710, May 18, 1911
COMPLETE RUPTURE OF THE SUPRASPINATUS TENDON. OPERATIVE TREATMENT WITH REPORT OF TWO SUCCESSFUL CASES
In a paper on "Stiff and Painful Shoulders," published in the Boston Medical and Surgical Journal for May 31, 1906, in speaking of rupture of the supraspinatus tendon in connection with subacromial bursitis, I presupposed, on anatomic grounds, the probable symptoms of such rupture as follows:
"One theoretical symptom (since the supraspinatus is put out of action) should be the persistence of passive and loss of active abduction. I am not ready to say this as yet, however, because in most cases the pain is so great that spasm prevents even passive motion, and later adhesion takes the place of spasm. When rupture of the tendon does take place, it probably is only partial and a Y-shaped attachment still remains to perform part of the function. In a similar way, the quadriceps may extend the femur when the patella is broken if the lateral expansions of its tendon are not torn. Nevertheless, I believe that the active function of the supraspinatus is important in elevation of the arm."
Since this paragraph was written I have had two cases of complete rupture of the supraspinatus tendon on which I have operated, and in both of which I was able not only to demonstrate the existence of the anatomical lesion in conjunction with the above symptoms, but succeeded by suturing the tendon to the tuberosity in bringing about complete restoration of the function of abduction. I have also, in a number of cases, verified the clinical diagnosis of a partial rupture such as depicted in the accompanying figure, which was produced in the other articles which I have written on this subject. (The reader is referred to the articles appearing in the Boston Medical and Surgical Journal for Oct. 22 and 29, Nov. 5,12,19 and 26, and Dec. 3, 1908. The figure alluded to is not repeated here.) This partial rupture is the common lesion, and, as I have explained, the remaining portion of the tendon is competent to take up the function when the sensitiveness due to the reparative process about the point of rupture has disappeared. The curious deposits of lime salts sometimes shown in the X-ray, and spoken of by Painter and Baer, are, I believe, faulty attempts at repair of these tiny ruptures of the tendon. The following two cases are quite definite because they present complete rupture of the tendon of the supraspinatus. Therefore, the function of active abduction was almost entirely lost.
CASE 1.—Mrs. J. A. Aged fifty-two. Born in Scotland. Referred by Dr. Kent, of Dorchester, March 7, 1909. Patient had always been a healthy, hard-working woman and had practically never been sick. On Oct. 3 of the previous year, i.e., five months before I saw her, while she was hanging recently washed clothes on the line in her yard, she endeavored to toss over a heavy blanket and felt something snap in her shoulder as she threw her arm up. She felt an intense pain and her arm fell and "hung by her side for a while." She was examined later by Dr. Kent, who found no thickening or ecchymosis. An X-ray was negative. Since then she had not been able to abduct the arm and had suffered much pain at night and somewhat during the day. The symptoms were in general those which I have described as the symptoms of adherent subacromial bursitis. The following points were, however, noticeably different. (1) There was little atrophy of the deltoid, and it even appeared hypertrophied on account of the apparent swelling of the joint beneath. (2) Under the fibers of the deltoid, beneath the acromion and over the joint, there was a distinct deep fluctuation as if the whole bursa were full of fluid. (3) The ability to start abduction was absent, but when the arm was passively abducted to about 140°, the patient, by a strong contraction of the deltoid, could prevent the arm from falling for an instant, but the slightest downward pressure made it drop to the side. External rotation was about one-half the normal. Operation.—March 11, 1909. Usual incision between fibers of deltoid. Roof of bursa abnormally thick with granulation-like bodies on its under surface. Escape of straw-colored fluid, about one-half ounce. The floor of the bursa was found communicating with the joint, because practically the whole supraspinatus was torn from its insertion and retracted inwards. The biceps tendon was exposed over the articular surface, but was apparently uninjured. For about one-half inch on the lower visible portion it was bright pink; the rest of it was normal in appearance. By holding the bursa wide open, pulling down on the arm and raising the elbow from the table, the retracted end of the supraspinatus could be seen. This was caught with a tenaculum and pulled down enough to suture with four heavy silk threads to the remaining portion still attached to the tuberosity. This could not be done exactly, but was done nearly enough so that it seemed possible for repair to take place along the silk sutures. A little gap was also left on each side, which was not covered with tendon substances. It was in a sense a suture a-distance. When the operation was completed it seemed as if there was a fair possibility of the supraspinatus obtaining enough attachment to enable it to perform its function, although the base of the bursa would necessarily remain a rough instead of a smooth surface. Dr. Kent gave ether, Dr. Vincent assisting. Dr. J. J. Putnam and Dr. M. P. Smith-wick present. June 9, 1909. Looks very strong and well. Sleeps well. Arm aches at times but not much. Pain in stormy weather (after use). Gets good use out of arm and does her own work. Can button back of dress and do her own hair. Real free abduction to 135°. Fair rotation. Muscles developing well and deltoid is strong. Very much pleased with result. This patient was demonstrated to the Interurban Orthopedic Club, March 25, 1911. The arm is perfectly well and the function is perfect. The only abnormal sign is that the deltoid is unusually prominent due to the presence of joint fluid in the bursa.
CASE 2.—Mr. D. R. Aged forty. Hostler. Referred by Dr. John Homans, Dec. 21, 1910. Patient is a strong, wiry Irishman. He has always been well. About three and one-half months previously, he had been saddling a horse in the stable and while tightening the girth he felt something in his shoulder give way and he fell to the floor. There was immediate loss of power in the arm, but lie managed to finish saddling the horse without raising that arm. That night he consulted Dr. Luce, of Canton, who found no ccchymosis, but thought there was slight crepitus. An X-ray a little later was negative. The hip was also hurt by his fall, so that for some time he was more bothered by that than he was by his shoulder and he was obliged to use crutches for several weeks. At the time he presented himself to me for examination the symptoms were at first sight those of the adherent type of subacromial bursitis, but on more careful examination the same signs that were present in the previous case were demonstrable, that is, (1) Relatively slight atrophy of the deltoid and an appearance of hypertrophy. (2) Fluctuation over the region of the bursa beneath the deltoid producing a "verwblbung" of the latter. (3) The persistence of nearly normal passive abduction with no active abduction. When the arm was passively abducted, the patient by a strenuous exertion of the deltoid could hold the head of the bone on the glenoid and thus prevent the arm from falling immediately. (4) In this case a distinct depression could be felt just above the tuberosity at the point where the tendon was torn away from the latter. A definite diagnosis was made and the members of the Boston Orthopedic Club invited to examine the case and witness the operation. Operation.—Jan. 10, 1911, at the Massachusetts General Hospital. As in the previous case, when the fibers of the deltoid.and the thickened roof of the bursa were incised, there was an escape of straw-colored fluid and the bursa was found to be in communication with the true joint. The supraspinatus had retracted so far that at first it could not be seen, and one looked directly at the articular surface of the bone with the uninjured biceps tendon lying across it. With some difficulty the supraspinatus tendon was caught with a tenaculum, freed and pulled forward. It was then sutured "a-dis-tance" to the tuberosity with heavy silk prepared with paraffine after the manner of Lange. As in the previous case, the retracted tendon could not be entirely united, but enough strands of silk were put in to make it possible for the function of the tendon to be replaced. Convalescence was normal and the patient was not allowed to use the arm in abduction for three weeks, but since then has been using it with more or less freedom. He was shown to the Interurban Orthopedic Club on March 25, and the following condition noted at that time: Patient is working every day—can chop wood and do other "chores" without pain. He can easily place his hand on top of his head or behind his back. Full abduction of the humerus on the scapula is, however, weak, and although he can elevate his arm, he cannot hold it in an abducted position against a downward pull of even moderate force. The strength of the arm in other respects is excellent and the patient is well satisfied. The function of the supraspinatus is fully as good as it was in Case 1, at the same length of time after the operation. I have seen only one other case in which I have made a diagnosis of complete rupture of the supraspinatus, and as I have not been able to persuade this patient to allow me to operate, his present condition is very instructive as compared to the two cases mentioned above. In spite of the fact that the patient is a powerful man with an extremely well-developed deltoid, he is now, four years after the injury, still unable to start abduction. As in the other cases, however, when the arm is passively abducted so that the patient's deltoid acts in the same line of force as the axis of the humerus and the remaining short rotators {i.e., subscapularis, teres minor, infraspinatus), the head of the humerus obtains a fairly firm contact with the glenoid so that the weight of the arm can be held by a great effort of will on the part of the patient. The slightest pull downward on the arm, however, will overcome what little power he has, and as soon as the fulcrum on the glenoid is lost, the arm drops to the side. It will be necessary for those readers who are interested in this subj ect to refer to the articles mentioned above to thoroughly understand this one, but, best of all, they should look for themselves at dissecting-room subjects, because injuries to this tendon are so common that I have never had any difficulty in finding examples of it in a single set (20) of dissecting-room subjects. The injury, as I have explained, is usually confined to a partial rupture of not more than one-quarter to one-half inch in breadth. Such complete cases as these three which I have reported are exceptional. The smaller ruptures, which are not of sufficient mechanical importance to interfere greatly with the function of the arm, are best considered with the subacromial bursitis which they cause. It must be understood that these ruptures are beneath the serous base of the bursa, which may or may not be torn through. If it is torn through, a communication is established between the bursa and the true joint. In operating for subacromial bursitis, if on entering the bursa one finds straw-colored joint fluid, a careful search will usually demonstrate a small opening into the true joint at the point of rupture. In only one case has it seemed worth while to me to make an attempt to suture one of these small ruptures. Usually these heal satisfactorily if the inflamed portion of the bursa over them is clipped away with scissors. I am convinced, nevertheless, that suture is necessary in long-standing complete cases such as those cited above. The one which was not sutured has a decidedly impaired function and for two years was unable to work. I have never seen the tendons of the other short rotators ruptured except in conjunction with that of the supraspinatus. Twice I have seen a longitudinal split between the tendon of the subscapularis and that of the supraspinatus. (End of 1911 paper.)
FIGURE 38. RUPTURE OF THE SUBSCAPULARIS Sketch by Mr. Aitkin of a specimen found and prepared in the dissecting room by my former assistant, Dr. T. W. Stevenson. It illustrates a rupture of the subscapulars without rupture of the supraspinatus, and is instructive from several points of view. This is the only instance of an exception to the statement in the last paragraph which has come to my knowledge in the twenty-two intervening years. It gives a very good idea of how the insertion of the supraspinatus, which in this specimen was intact, normally fills the sulcus at the anatomic neck, and covers the tuberosity, thus leaving a perfectly smooth exterior contour beneath the base of the bursa. In this case the bursa has been thoroughly dissected away in order to show the superficial fibers of the tendons passing over the tuberosity and becoming continuous with the periosteum below. In Chapter X it will be shown how these fibers cover up and hold together the fragments in comminuted fractures. The figure also gives a good idea of the manner in which the supraspinatus emerges from under the coraco-acromial ligament and acromion. The lower or inner edge of the muscle has been rather sharply dissected, but in the undissected specimen this edge blended with the upper portion of the subscapularis. Below this, one sees that most of the subscapularis has been torn away from the conjoined tendinous cuff, so that the biceps tendon, running through its groove between the two tuberosities, is exposed at the left edge of the gap. Internal to the biceps tendon we see the lesser tuberosity, from most of which the subscapularis fibers have been evulsed. The knobby character of the surface of the exposed tuberosity is shown; an appearance usually found in old cases where the tuberosity is exposed by evulsion of the fibers of any of the other tendons. (See frontispiece and Fig. 40.) In other words, this knobby look is the superficial appearance of the "excrescences" or "volcanoes" spoken of on page 91, and also shown in Plate V, Fig. 1. In the upper half of the gap above the excrescences is the exposed cartilage of the joint. If this gap extended outward from the biceps tendon, instead of inward, it would represent the condition which we usually see; i.e., rupture of the supraspinatus rather than of the subscapularis. It is not unusual to find in the dissecting room extensive tears involving both tendons, but it is very unusual to find the subscapularis involved alone, as in this case. One can readily picture how easy it would be to produce such a condition as this by forcibly performing external rotation in a case of "frozen shoulder." This diagram also gives an excellent idea of the coracoid process, coraco-clavicular and coraco-acromial ligaments, as well as of the conjoined origin of the internal or short head of the biceps, and of the cornco-brachialis muscles. It also shows the insertion of the pectoralis minor, the tendon of which protrudes as a stub at the inner side of the coracoid process in this diagram.
Although it is over twenty years since the above paper was written, I have very little of importance to add or subtract from it. I followed the two cases for many years and the results continued to be satisfactory. Although the second case never had perfect function in his shoulder, he could do all sorts of farm and stable work without complaint. As he worked for a neighbor, I had frequent opportunity to observe him for over ten years. There is a point in the quoted paragraph which might cause confusion. At that time, 1906, I did not realize that the stooping posture was such a great help in testing mobility in the scapulo-humeral joint. One may get the impression, when examining a patient in the upright position, that scapulo-humeral adhesions exist, and yet in the stooping posture, positive proof will be given that the joint is movable. It is important for the reader to understand at once that scapulo-humeral passive mobility is a sine qua non for the diagnosis of a complete rupture of the supraspinatus, and that in the stooping posture this mobility is much less inhibited by pain and spasm. I did not fully appreciate this point in 1906, and even in 1911 I had hardly grasped it, and did not accent it enough in the above paper. It will be discussed later in this chapter. The only other point which I desire to correct is in the next to the last paragraph. I do not think I was justified in making such a general statement as "usually these heal satisfactorily if the inflamed portion of the bursa over them is clipped away with scissors," for I am still in doubt as to how to treat the incomplete ruptures. I have really little more than I had in 1911 to give to the profession in this book, except that repeated experience with the same signs, symptoms, operative findings and follow-up have increased my confidence in the accuracy of my former observations and opinions. During these years I have only operated upon about forty belated cases, although I have made the diagnosis over a hundred times. My results have been good but by no means perfect, because I never see these cases in their early stages, when I am sure the operations would be easy and the results entirely satisfactory. This book aims to try to teach the practicing physicians, who see the cases soon after the injury, how to recognize this lesion immediately, and to rush the patient to a competent surgeon as promptly as if the patient had a broken arm—a much less disabling accident. As in acute appendicitis, early recognition and prompt operation are of the utmost importance. The remainder of this chapter will therefore be devoted to a more detailed discussion of the symptoms.
FIGURE 39. RUPTURE OF THE SUPRASPINATUS A schematic posterior view of a case of ruptured supraspinatus, to show the posterior short rotators and the sulcus and eminence formed where rupture of the supraspinatus has occurred. The acromion has been sawed off at its base. The reader should study the frontispiece and the next figure in connection with this one.
The size of the rent in the tendon is an important factor since the degree of the severity of each symptom may vary with the extent of the rupture. It seems best to discuss first the symptoms of those cases where the rent is large, as in the two cases which I first reported and which I have called "complete." This means that at least that portion of the conjoined tendinous insertions supplied by the supraspinatus has been torn away, with or without portions of the adjacent tendons. These are the cases which should certainly have the benefit of immediate operation. I do not at present advocate operating upon incomplete cases, for it is likely that after a few months they may heal in whole or in part. On the other hand, there is good reason to believe that the complete ruptures which make an open communication between the joint and the bursa never do heal entirely unless sutured. In other words, the symptoms have had to be pretty pronounced in order to make me willing to operate. It is significant that almost invariably the rent in the tendon has been found to be larger than anticipated. I have perhaps been over-conservative in deciding to operate, but the reader must remember that I have taken the responsibility of doing an operation which is not generally practiced, and naturally I have been somewhat cautious. It is my sincere belief, however, that a small exploratory incision is harmless and that the practice of promptly making such an incision in acute, doubtful cases is to be encouraged, provided the operator has carefully studied the anatomy of the region. Almost all surgical operations which are now standard procedures had similar histories. Many human sacrifices were required to teach us not to delay when the symptoms strongly suggested appendicitis, perforated duodenal ulcers or intestinal obstruction. The fact that death occurs when we procrastinate in these serious cases has made us, in the public eye, more to blame for delay than for making negative explorations. The surgeon who does explorations on these injured shoulders might be criticized today and yet a few years hence be blamed for the failure to do them. Moreover, the laboring man with a shoulder injury has not yet been educated to dread this particular lesion as he has been to fear appendicitis.
FIGURE 40. X-RAY OF SPECIMEN SHOWN IN FRONTISPIECE Owing to the fact that it had been dissected, air has entered both the joint and the bursa, somewhat after the manner indicated in the cover design. It suggests appearances which we might see if we used air or opaque fluid injections in the bursa and joint. It shows a little irregularity on the surface of the tuberosity, which in the painting gives the appearance that I have called a " volcano "; i.e., a small eminence which has a craterlike place in its center. These little eminences are found in many old cases of ruptured supraspinatus. They may represent a productive osteitis due to irritation from contact with the acromion during elevation. The figure also shows two small caverns such as those illustrated in Plate V, Fig. 1 and Fig. 2. I am not sure just what these caverns indicate.
The account of symptoms given in my 1931 paper before the American College of Surgeons was presented in a twenty-minute talk, and while I still think it accurate, I am not satisfied with its arrangement nor with the amount of detail its time limit permitted. The immediate symptoms were not separated as they should have been from those that supervene later in the course of the disability. The early signs should have been emphasized, because success in treatment must depend largely on prompt diagnosis. It is easy enough to recognize one of these cases when atrophy has developed and the lapse of time has shown the persistent character of the lesion, but to make the diagnosis on the day of, or on the day after, an injury is quite another matter. Probably insurance records would show that 80 or 90 per cent of employees complaining of shoulder "strains," return to work within three months. Certainly we could not recommend exploratory incision of the bursa in all of these cases in order to detect perhaps 10 or even 20 per cent where the rupture would be complete. When we have learned just what to do when we find minor ruptures or tendinitis, it may become wise to make such incisions as a routine, but at present the bill for negative explorations would be far too large. I contend that it is possible to detect the severe cases.
CERTAIN CONDITIONS, SYMPTOMS AND SIGNS WHICH INDICATE COMPLETE RUPTURE OF THE SUPRASPINATUS TENDON AND WHICH SHOULD BE PRESENT WITHIN TWENTY-FOUR HOURS AFTER THE ACCIDENT.
(1) Occupation—labor. (2) Age—over 40. (3) No symptoms in shoulder prior to accident. (4) Adequate injury—usually a fall. (5) Immediate sharp, brief pain. (6) Severe pain on following night. (7) Loss of power in elevation of the arm. (8) Negative X-ray. (9) Little, if any, restriction when stooping. (10) Faulty scapulo-humeral rhythm.
(11) A tender point,
(12) a sulcus, and
(13) an eminence
(14) at the insertion of the supraspinatus,
(15) which cause a jog,
(16) a wince and
(17) soft crepitus as the tuberosity
(18) disappears under the acromion when the arm is elevated, and usually also, as it reappears during descent of the arm.
Here are eighteen conditions to be fulfilled—an especially exacting syndrome. If such a syndrome is present I do feel that not only is exploration indicated but that it should be strongly urged, for immediate suture should be a simple and successful operation. Delay means retraction of the tendon and a much more serious problem.
I feel confident that this syndrome must exist, although I admit that I have never seen one of these cases within twenty-four hours of an injury. My best way of knowing the immediate symptoms is from the accounts of the patients or of their physicians given weeks or months after the injuries. Moreover, since these same symptoms are found at varying periods from three weeks to many years after the accidents, and do not vary much with the lapse of time, either in quality or in degree, it is likely that they were present at first. In a case in which they were all typical I should be positive of the diagnosis, and should urge operation. If several of the conditions were not fulfilled, it would influence me against operation, but if there were doubt, a negative exploration, if correctly performed, is a trivial matter, although the patient must be hospitalized in case a rupture is found. If suture is done he should remain in the hospital for about ten days; if the exploration is negative he might well be discharged in twenty-four hours. These eighteen points will be discussed in more detail in numerical order.
(1) Occupation. The great majority of cases must belong to the laboring classes, for I have seen only one case in a person whose occupation did not or had not required heavy work. This suggests that overuse as well as increased liability to accident may be a contributory cause. The occupations are given serially in the following paragraph because if they were tabulated the list would not give the same impression of sequence which is presented by patients as they come for examination. On looking over these occupations the reader should contrast them with those in the following three paragraphs which are the occupations of patients who have had calcified deposits, tendinitis and partial rupture.
COMPLETE RUPTURE OP THE SUPRASPINATUS (100 Cases) Women 8%
Housewife, hostler, plasterer, street cleaner, housewife, coal-heaver, waiter, paper cutter, laborer, housewife, marble worker, currier, cooper, housewife, stationary engineer, two laborers, longshoreman, wrecker, teamster, two laborers, steamfitter, three laborers, truck driver, stock fitter, cook, stableman, painter, two laborers, truck driver, laborer, lineman, lather, farmer, three laborers, harness maker, wood molder, planer, electrician, plumber, mechanic's helper, laborer, roofer, laborer, longshoreman, riveter, two laborers, porter, cooper, two laborers, steamfitter, laborer, lather, steamfitter, laborer, stationary engineer, laborer, store clerk, carpenter, laborer, night watchman, longshoreman, laborer, taxi driver, lineman, laborer, painter, coal-heaver, laborer, foreman, truck driver, laborer, construction, painter, laborer, rubber worker, laborer, painter, laborer, carpenter, meat cutter, floor layer, stitcher, two laborers, housewife, foreman, laborer, store clerk, burnisher, teamster, laborer.
CALCIFIED DEPOSIT (100 Cases) Women 34%
Housewife, two no occupation, two physicians, chemist, physician, superintendent, two physicians, business, no occupation, business, manufacturer, architect, business, three physicians, milk delivery, supervisor, ironworker, housewife, filing clerk, physician, machinist, histologist, housewife, physician, business, no occupation, physician, no occupation, pipefitter, stenographer, no occupation, physician, garage, postman, business, waitress, musician, shipper, laborer, bookkeeper, machine tender, porter, teacher, laborer, housewife, broker, housewife, business, baker's helper, two salesmen, organist, weaver, housewife, shoemaker, forewoman, box-maker, two laborers, housewife, shoe machinist, farmer, housewife, advertising, paper mill, housewife, surgeon, real estate, advertising, housewife, machinist, boxmaker, store manager, wool handler, laborer, physician, truck driver, shoe worker, teacher, knitting mills, housewife, plasterer, laborer, shoe stitcher, clerical, physician, treasurer, investments, laborer, housewife, laborer, beauty parlor, manufacturer, salesman, manufacturer.
TENDINITIS (100 Cases) Women 58%
Two housewives, two no occupation, army officer, two housewives, carpenter, tailor, nurse, no occupation, tailor, nurse, business, P. O. clerk, secretary, three housewives, no occupation, physician, maid, coppersmith, merchant, housewife, jeweler, minister, harnessmaker, housewife, hostler, tailoress, storekeeper, priest, no occupation, photographer, housewife, professor, housewife, carpenter, starter, housewife, shoe laster, housewife, two no occupation, housewife, roofer, civil engineer, two housewives, cigar maker, judge, shoe manufacturer, no occupation, nurse, three housewives, physician, housewife, laborer, two housewives, physician, two housewives, store clerk, housewife, social worker, housewife, insurance broker, factory worker, two housewives, desk work, social worker, salesman, food checker, housewife, consulting engineer, banker, physician, invalid, two housewives, nurse, laundry, writer, surgeon, two housewives, two physicians, foreman, lawyer, grocer, executive secretary, nurse, public accountant, no occupation.
PARTIAL RUPTURE (100 Cases) Women 11%
Three laborers, farmer, carpenter, eight laborers, baker, plumber, laborer, housewife, two laborers, carpenter, housewife, painter, laborer, mechanic, garage, two laborers, writer, three laborers, physician, laborer, carpenter, teamster, laborer, carpenter, laborer, machinist, laborer, housewife, teamster, cook, stone mason, bricklayer, carpenter, three laborers, store, housewife, laborer, mechanic, housewife, store clerk, cook, machine oiler, laborer, two housewives, insurance, store, business, janitor, hoisting engineer, painter, meat cutter, three laborers, florist, two laborers, ironworker, nurse, gardener, shoe factory, clerk, plasterer, lawyer, laborer, no occupation, student, bartender, manager, housewife, laborer, foreman, bricklayer, horseman, two laborers, nurse, farmer, machinist, real estate, gardener, laborer, housewife, tailor.
Both occupation and sex are of importance in the diagnosis of shoulder conditions. Men who have done heavy labor are typical subjects for complete ruptures of the supraspinatus, and women of the so-called "leisure class," for tendinitis (frozen shoulder). Calcified deposits are more characteristic of the class who have gainful but not laborious occupations (the white collar class) ; i.e., they are not usually found in inactive people. Partial ruptures are also in the main characteristic of men of the laboring group, but they may occur in the more active and athletic members of the leisured class, both in men and in women. These observations were already made from general impressions in the course of my practice, but they are in part confirmed by the above analysis of the occupations of 400 cases. The detailed accounts which each patient has given of his or her occupation and other activities, are of even greater weight in confirming my own impressions. For instance, the term housewife may apply to a woman who does all the work and washing for a large family, or to a lady who scarcely uses her arms, or to an active wife who plays golf, sends out her washing and only occasionally uses her kitchenette. The percentage of women varies greatly in the different classes, eight per cent, eleven per cent, fifty-eight per cent and thirty-four per cent. The eight cases of complete rupture and eleven of the fifteen cases of partial rupture were women whose work was really laborious. The fifty-eight tendinitis cases were chiefly women of the leisure class and the thirty-four calcified cases were active single women or wives.
Click for large image
(2) Age. The four clinical entities also affect different age groups. Young persons below twenty-five seldom have any of these conditions. Apparently in young people the tendon is stronger than the bone in which it is inserted, and stresses, which in later life would break the tendon, cause fracture of the bone or separation of the tuberosity. Chart I shows that the four entities affect, in the main, persons in the latter half of life, and that the occurrence of tendinitis both of the calcified and uncalcified forms precedes the peaks of incidence of the ruptures, partial and complete, by about five to ten years. The curves of the two forms of tendinitis, calcified and uncalcified, have their peaks at the same period, but the rise of the curve is distinctly earlier in the calcified form. These facts suggest that injuries of the tendon prior to the thirtieth year either are rare or that the tendons are capable of normal repair. Then follows a period when repair is uncertain and is apt to be complicated by the deposit of calcium. Later even this incomplete repair fails.
WOMEN—CHART III
Click for large image
If we chart separately the male and female cases there is a marked contrast. The curve of the female cases suggests that tendinitis, both calcified and uncalcified, may be related to the menopause or to the age when the teeth begin to loosen. By comparison of the two charts we find that calcified deposits apparently occur somewhat earlier in males than in females, and their occurrence tends to diminish at the period when they are highest in the female. The contrast of Chart II and Chart III makes it very clear that the more serious forms of rupture of the supraspinatus are characteristic of the male toward the end of his laboring days. The period of life shown in all the curves is that in which the teeth are usually in decay. If these charts are made without separating the cases in four entities the contrast between the ages of males and females is even greater, so that the coincidence with the menopause is more striking.
MEN—CHART IV
Click for large image
(3) The history of a previously painless and useful arm is unreliable for two main reasons. First,—previous troubles may have been forgotten. Men of the laboring classes put up with a great deal of soreness and pain and forget it easily. Such a matter as an attack of bursitis years before, may readily be forgotten. I would rather have the history of previous troubles from a man's wife than from the man himself. I am inclined to think that in many cases where complete rupture has occurred, there may have been previous minor troubles, which might have indicated either partial rupture of a few fibers, or a "calcined deposit." However, my records do not show this, for in only nine of a hundred cases could a history of previous trouble be obtained. The second reason is that men may lie as well as forget. The statements of employer and fellow workmen are sometimes more accurate than the patient's own. Patients may conceal previous trouble to avoid losing compensation. The other shoulder should always be examined in these cases, for occasionally one finds signs of a partially ruptured tendon or of chronic bursitis there, although no complaint is made of symptoms. This would, of course, be very suggestive of preexisting disease in the injured shoulder. However, we must not forget that a rupture may occur as a bona fide injury in degenerated or diseased tendon. (4) Adequate injury seems pretty well illustrated by the following brief accounts of the accidents in twenty-one successive cases which were proved by operation, and in seventy-nine others in which the diagnosis was made but not proved.
ACCIDENTS (Operated Supraspinatus Cases)
57. "Fell taking down an old gallery." 75. "On this date (Aug. 25, 1922) he was engaged with others in hoisting lumber, when a plank slipped off the hoist and struck him in the side knocking him down." 83. "On Jan. 17th, 1923, he fell downstairs and injured his left shoulder." 88. "On Feb. 1st, 1926, while at work he was pulling a heavy case along the floor with a hook. The hook slipped and as he caught his balance he felt something snap in his shoulder accompanied and followed by intense pain." 89. " When getting off truck caught his hand in fly wheel. Cuts of hand." 96. "On April 4th, 1927, he slipped on a concrete floor and injured his left shoulder." 97. "On Nov. 8th, 1926, he was pushing a freight car with another man, using bars. His bar slipped and he fell down wrenching his left shoulder." 98. "Six weeks ago he had slipped on the ice while at work and had injured his right shoulder. He fell on his back striking his elbow, but had no bruise on the elbow. (It is probable he threw up his arm to get his balance.)" 102. "On Nov. 2nd, 1927, he was piling some 100-lb. sacks of beans with another man who stood above him and received the sacks as he threw them up. On one throw the other man failed to connect with the sack and the entire weight came on the patient's right arm. He felt something in his shoulder snap with a sharp pain." 106. "On January 20th, 1928, he was cranking his truck, which he uses to deliver cans of ice cream. The engine backfired and he felt a sharp pain in his right shoulder." 107. "On Jan. 18th, 1928, she fell on the floor of the kitchen where she works and dislocated her left shoulder." 108. "At some time in July (date uncertain) while at work he was turning a board and felt something snap in his right upper arm about the middle, in the region of the long head of the biceps. There was a sharp pain which went away in a few minutes." 112. "On March 10, 1928, he was wheeling a barrow up into a barn when he slipped and fell forward on the barrow, but did not let go of the handles." 115. "On August 21st, 1928, about 1.30 P.M., slipped and fell from piazza roof, striking the edge of the piazza floor with his right arm in abduction. Had immediate pain in shoulder and arm." 119. "Day before Thanksgiving, Nov., 1928, fell off staging three feet high. Walked backwards off." 123. "On Jan. 14th, 1929, he slipped on an icy platform and hit on his left elbow." 127. "On Oct. 17, 1929, was handling 2x4 lumber and stepped in a hole. Fell against left shoulder on pile of lumber, hitting on elbow." 128. "He slipped on the ice near a building and fell, striking the side of his right shoulder against a low step. This is what he says, but such a fall as that would probably be impossible. It is more likely that he threw his arm up as he fell." 129. "On October 24th, while piling some pipe, he was standing on a pile of pipe which rolled under his feet and he fell between two piles of pipes." 185. "He slipped on the ice and fell. After he got up, he found that he could not raise the left arm." 137. "On May 13, 1930, he had a fracture near the left elbow which healed satisfactorily and he went back to work about September 1st. On October 7th, in Andover, he fell and dislocated his left shoulder."
ACCIDENTS (Unoperated Supraspinatus Cases)
". . . he was doing some overhead work standing on a support twelve or fifteen inches high. The support slipped and he fell on his right hand and elbow, and then forward on his shoulder." ". . . he was pulling on a rope which suddenly gave way. He fell to the ground with his right arm below and behind him. He felt a sharp pain in the shoulder as if a bone had broken." ". . . he fell about ten feet while at work and injured his shoulder." ". . . he had been hit by an automobile, knocked down and taken to the Boston City Hospital. His shoulder had been injured." ". . . he was cranking his truck, and had a kick back. He thinks the handle struck him on the lower part of his upper right arm, but his shoulder was w.renched." "... when walking in a dark passageway, he stepped over some steps and in trying to save himself caught with his left arm on the wall, but kept his feet. He had a violent pain in his left shoulder but pulled himself together and went to his next job." ". .. he was struck on the left shoulder by a falling bale of hemp while at work. He was knocked down and much shaken up, but pulled himself together and continued to work the rest of the afternoon with his right hand." "Fell off wagon when unloading barrels. Hurt badly at time and went to Camb. Relief Hosp." ". . . he was lifting a barrel and something snapped in his shoulder, since which he has been unable to work." ". . . he tripped on a rolling log and fell injuring his left shoulder." ". . . he fell down some stairs and injured his right shoulder." ". . . the employee slipped on a loose plank and injured his left shoulder and right foot." ". . . he was pulling on a chain fall and something slipped in the right shoulder." ". . . he was jammed between a moving truck and the side of a building. Fortunately, he was near the corner of the building and the moving truck carried him around the corner, squeezing him from side to side as it did so. His left arm immediately became powerless." ". . . he fell from a staging and injured his right shoulder and has not yet recovered the use of it for anything requiring the function of abduction." ". . . he was filling a wagon with coal when the horses started and he fell in between the wagon and the side of the coal-pocket." ". . . he fell forward at the top of a flight of stairs and injured his shoulder as he supposed by hitting some beams." "A frame which he was moving dropped and to prevent it striking his feet stepped aside, losing his balance and falling to the floor." ". . . she felt something snap in her shoulder (left) when raising some wet clothes on a pole to put them in a laundry machine." ". . . while raking grass on a steep bank, he slipped and injured his left shoulder." ". . . as he was stepping out of a tip cart on the hub of the wheel, he slipped and fell heavily to the ground injuring his left shoulder and also his right shoulder to some extent." ". . . the employee was carrying a plank with another man, when one of the planks on which he was walking gave way, letting part of his body through the pier so that he sustained injuries to his left shoulder, arm and leg." ". . . she fell over a bag of soles and injured her right shoulder." ". . . he slipped off a plank and fell headlong to the floor, about four feet." ". . . large heavy car six or eight feet on the side. On this occasion the car skipped the track in spite of his efforts to prevent it, striking him on the left arm." ". . . he says that he was using his truck to load heavy rubber bales weighing about 350 lbs. each. He had put the edge of his truck under one such bale and reached forward with his right hand to pull the bale toward him on to the truck. As he pulled, he felt something give in his right shoulder." ". . . he was helping with other men, to pull a heavy truck, when he felt something give way in his right shoulder." "He was carrying a roll of leather and fell on the floor in the room where he usually worked." ". . . he fell from his truck and injured his left shoulder." ". . . he fell thirty feet from a staging and was badly bruised all over." ". . . he was on a lumber pile helping to load a truck. He was using a pick to drag the lumber. The pick slipped and he felt a sudden pain and something snapped in his arm at the right shoulder. His arm fell limp at his side." ". . . he slipped on some stairs and injured his left shoulder. . . ." ". . . fell among some barrels in the hold of a vessel and struck his right shoulder again." Had had previous similar accident six years ago, and never full use of arm since. ". . . while working in a meat market in Nantucket, he slipped on going out of the ice chest and injured his right shoulder." ". . . while carrying rubbish on an incline in the factory where he works, he fell and injured his right shoulder. As he says, 'it went dead immediately.'" "He was piling wool at the time, lost his balance and fell from one bale to some other bales not far below. As he fell he felt something snap in his shoulder which did not hurt him very badly at the time. . . ." ". . . slipped on ice in street." ". . . while working on a flat-car he fell and struck his right shoulder on the side of the car." "While at work in the factory in Lawrence ... he was in an elevator holding a heavy plank in both hands to steady it. One end of the plank was on the floor of the elevator and it stood vertically. Some one below started the elevator downward and then upward. As it went up it thrust the top of the plank violently against the top of the well. This shattered the heavy plank just above his hands with extreme violence and he was thrown into the corner of the car in a heap." ". . . he fell off the back of a load of straw and injured his shoulder." ". . . he again fell downstairs—only a few steps—and again injured his right shoulder." " Slipped and fell, and a box or case fell over on him." ". . . while directing some work where a floor was being replaced and the boards were up, he tripped on a beam and fell on his right side against another beam, probably breaking some ribs." ". . . he received an injury to his left shoulder when trying to move a large rock with a pitchfork. He felt something snap in his shoulder joint and suffered a sharp, severe pain at the same time." "He injured his right shoulder by falling from a truck." ". . . he was pulling some lumber off a truck and when it slid off quicker than he expected he fell backward and injured his left shoulder." ". . . he fell four feet, striking on the pavement, and inj ured his left shoulder." "... he slipped on an oily floor, and hurt his right shoulder and left shin." ". . . he fell from a staging about six feet to the floor below, and injured his right shoulder." ". . . he fell from a ladder and sustained injuries to the left shoulder and ribs." ". . . he was on a roof sawing a plank, and was standing on an extension ladder, which fell with him thirty-one feet to the ground. His right shoulder was injured, and his nose was cut" "Strap from machine fell off wheel and hit patient on right shoulder." ". . . he was working with others on a bridge in Rumford, Maine, helping to receive some cement in a frame from a bucket. In some manner, the bucket swung in the wrong direction and the patient fell from the bridge a distance of fifty feet." ". . . he was lifting a concrete block and felt something give in his left shoulder." ". . . he fell injuring his left shoulder." ". . . he had started to crank a hoisting truck when the starter began to work and the crank flew round and struck him on the right shoulder." "Slipped on ice." "Fell yesterday and sustained a contusion over outer end of right clavicle." ". . . while helping to unload a truck, a derrick knocked down a platform above him, and something, probably a heavy plank, fell on him and others working with him. He was knocked out by the blow, and cannot describe exactly the manner in which the plank struck him, but he knows it injured his shoulder and elbow and there was blood streaming down his arm." "He was pulling hard on a gunny sack, which gave way, and he fell over and thinks he struck his right shoulder." ". . . she tripped and fell on the floor at her work. She dislocated her right shoulder, bruised her knees severely and cut her face." "He was standing on stony ground swinging a sledge hammer, when he had to step back quickly. As he did so, he lost his footing and the sledge hammer, which he was swinging, carried on around his body so that his left shoulder was in an awkward position. He felt something snap in the left shoulder."
One may interpret the mechanism which produces this injury in several ways, but a sudden character is common to all of the accidents, which are generally falls. It is my belief that the rupture usually takes place from sudden elevation of the arm in attempting to regain balance, particularly if the hand is at the same time grasping a heavy object. Under these conditions a tremendous strain must be suddenly thrown on this little tendon as it attempts to quickly overcome the inertia of the arm, and perhaps, in addition, that of some heavy object held in the hand. In my first case, the woman attempted to throw a heavy, wet blanket over a clothes-line. It seems to me that this case, like a "slowed down movie," typifies the kind of strain which occurred in most of the other accidents. I believe that the even more sudden effort to regain balance during a fall caused the damage, probably before the patients struck the ground. For anatomic reasons one cannot, in falling, strike on the supraspinatus, because it is protected by the acromion. Undoubtedly, however, in some cases, the tendon may have been torn in conjunction with dislocations, because of the leverage of the humerus on the fulcrum of the acromion. This mechanism will be explained in Chapter IX.
(5) A sharp pain in the shoulder at the time of the accident is almost always spoken of, although occasionally complaint of it is not volunteered. Sometimes patients say that they have felt something actually snap and think that they have broken a bone. Sometimes they feel that something has struck them on the shoulder. It has been explained on page 9 in the chapter on anatomy that histories of striking on the head of the humerus are unreliable because the acromion intervenes, and on page 144 that in falling, the arm is usually raised before the top of the shoulder can strike the ground. Consequently it seems to me that these tendons must usually be ruptured by indirect violence or sudden efforts of the muscles to overcome the inertia of the dependent arm, especially if there is a weight as a pick or shovel in the hand at the time, or the hand grasps something to save the man a fall. Often the fall is so sudden and the man so confused that the only thing he can understand is that he has hurt his shoulder and attributes the pain to having hit something as he fell.
(6) So far as I can judge from histories, there is then usually an interim of a few hours after the acute, immediate pain has somewhat subsided before the more severe pain comes on. Often the employee does not even consult a doctor at once, but tries to work the day out, favoring his arm. Perhaps he does not report the accident to his foreman. In the evening the pain becomes worse, and later in the night intolerable. He calls the doctor, or sits up in a chair, or "walks the floor." Next day he is pretty sure to report that he cannot work, but may persuade an accommodating foreman to let him "hang around" for a day or two until he gets better. These patients usually think the injury of no great consequence and expect "to have it wear off." This hopefulness is generally confirmed by the doctor's opinion, who perhaps may never have heard that such lesions occur. This attitude of mind of both patient and doctor is the main cause of delay in diagnosis and appropriate treatment. It seems to me that the following theory is the probable explanation of the interim between the sharp pain when rupture occurs and the intense pain which appears some hours later. These tendons are not very vascular, and when they tear, there is probably very little bleeding; what there is, would come from the tissue between the bursa and the tendon. The interim spoken of would come during the period it would take this slight hemorrhage to distend the joint and bursa somewhat, i.e., enough to start a tension pain. This would create some spasm, and the tension caused by this would stop the slight bleeding. It would take several nights or perhaps a week for tension and spasm to subside and the hemorrhage to absorb. During this period the acute pain would continue.
(7) Inability to raise the arm is a constant symptom, but one must be on guard not to mistake unwillingness for inability. After almost any shoulder injury there may be pain when attempt is made to raise the arm, owing to the fact that the head of the humerus has to be forced upward to gain its fulcrum on the glenoid. The mere fact that the muscles have to exert tension to do this, causes pain in whatever structure about the shoulder may be injured. Therefore, the examiner must be sure that an honest effort is made to ignore the pain and elevate the humerus. It takes experience to tell whether such an effort is made, and one judges it by the degree of tension palpable in the deltoid. Even in the case of trivial injuries, such as ruptures of a few fibers of the supra- or infraspinatus, the symptom of inability to raise the arm may be pronounced, simply from the fact that the power to exert the appropriate muscles is inhibited by sensitiveness to pain. As explained on page 59, the deltoid needs the assistance of the supraspinatus and of the short rotators to hold the head of the bone on its fulcrum in order to have proper direction for its power; If the supraspinatus is torn, contraction of the deltoid brings the arm upward on the vertical axis of the humerus, and the amount the shoulder is raised will depend on the amount that the scapula, moving via the. sterno-clavicular joint and at the acromio-clavicular joint, can rise and rotate on the chest wall. Formerly I thought that it was necessary to have this symptom of inability to raise the arm absolutely demonstrable in order to make the diagnosis of rupture of the supraspinatus, but experience has shown that, even when the supraspinatus is torn across its full width, the other short rotators can sometimes hold the head of the humerus on its fulcrum sufficiently to permit the patient to weakly perform elevation. However, as will be explained under No. 10, this elevation is never accomplished with a normal scapulo-humeral rhythm.
(8) A negative X-ray is almost always reported after these in juries. I believe that in the near future we shall be able to make the X-ray of more use in this diagnosis, either by using injections into the joint of non-radiable fluid, or by developing a soft tissue technique which will show the rupture. However, at present, negative X-rays are the rule, for ruptures which do not involve the bony facet of insertion are not shown in the film. A negative X-ray is of some positive importance, however, for it rules out the two conditions which are likely to make confusion in the diagnosis, that is, fracture of the greater tuberosity and the presence of calcified material in the tendon. In long-standing cases changes in the structure of the trabec-ulae of the tuberosity which may be shown by the X-ray do take place. These are described on page 92.
(9) In the symptom complex of this condition, lack of restriction of motion takes a very important part, and this lack of restriction can be best determined when the patient is stooping from the hips with the knees extended. The patient should stoop (Fig. 47) to the horizontal position, letting the arms hang loosely toward the floor. In this position the deltoid is relaxed and there is no fulcrum needed in order to have the arm passively raised, i.e.-, brought forward into complete elevation (quadruped extension) ; in fact, even if this is not passively done, the patient has to exert but little muscular power to swing the arm forward into this position. This he is usually able to do without much pain. The examiner may then hold one hand on the scapula and with the other raise the lower end of the humerus, so that he takes the full weight of the arm and permits the patient to stand upright with the arm still in complete elevation. Such a procedure eifectually rules out restriction from adhesions. Even if the supraspinatus is torn, the patient can retain the arm in this up right position. If he stoops again he can lower it without much pain, and then if he rises to the upright position with the arm relaxed, the humerus will, by gravity alone, come into its normal position at the side of the body. When I say that lack of restriction is an essential symptom, I must not be taken too literally, for there is often, in fact usually, in these cases, a very little restriction in extreme elevation and in rotation, probably due to the presence of fluid.
(10) Faulty scapulo-humeral rhythm is a sine qua non for this diagnosis. When one sees a patient who in raising the arm lets it ascend to the horizontal while maintaining (quadruped) flexion of the scapulo-humeral joint, and then slowly and painfully (perhaps with a little help) proceeds to complete elevation by motion in the scapulo-humeral joint, and finds that when the patient 'allows the arm to descend, he keeps the scapula and humerus fixed in (quadruped) extension until he reaches the horizontal, and then quickly flexes it, a presumptive diagnosis oi rupture of the supraspinatus can be made. Ascent in flexion, descent in extension, might be a slogan for students to learn in this connection. To express this lack of scapulo-humeral rhythm in other words, we may say that the normal ratios of the movements of the joints in elevating the arm, explained on page 59, disappear. Instead, in the first part of the movement only the motions of the scapula on the chest wall are concerned; then the relations of the humerus and scapula change, wholly above the horizontal. In the descent of the arm the reverse is the case—no scapulohumeral motion takes place above the horizontal, but all below it. While the symptom is a sine qua non to the diagnosis of complete rupture of the supraspinatus, it is also present in most cases of minor ruptures and in many cases of calcified deposits. It therefore is an indispensable but not a pathognomonic sign.
(11) The tender or sensitive point is not complained of by the patient as a rule, and in fact he is unconscious of its exact location until the examiner finds it, when he usually says: "You have your finger right on it." Without your aid in locating it he will perhaps know that there is a tender point, but locate it deep under the acromion or even in the spasmodic deltoid muscle down near its point of insertion. In fact, the lower portion of the deltoid is usually also tender. Examination of this part of this muscle in all these patients nearly always shows that there is some thickening and sensitiveness, as compared to the normal side. In the old, chronic cases the sensitiveness at the point of rupture may not be very noticeable, and even when the exact point is pressed the patient will hardly admit that it is tender. Presumably in fresh cases it would be especially sensitive.
FIGURE 41. POSITION OF HANDS FOR EXAMINATION OF SHOULDER
The left thumb lies along the depression below the spine of the scapula and the tip of the forefinger is just anterior to the acromion. The other three fingers cross and hold the clavicle. Thus the shoulder girdle is firmly held and any motion of the scapulo-humeral joint is at once detected.
In speaking of the 11th, one is necessarily obliged to consider the remaining symptoms, since the tender point is at the gap between the ends of the torn tendon, and this gap is the reason for the sulcus and eminence, which may be felt just anterior to the edge of the acromion, when the arm is in dorsal flexion. If the examiner remembers his anatomy, the tender point, sulcus and eminence will be found to be at or near the insertion of the tendon of the supraspinatus. It is the passing of this irregular sulcus and eminence under the acromion and acromio-clavicular ligament which causes a jog, a wince, and a soft crepitus, as the sensitive, irregular base of the bursa disappears under the acromion when the arm is brought forward by the examiner. The two figures (41 and 42) present the condition, it seems to me, more vividly than could any description. However, I will give a few brief additional points under each one of the remaining headings.
FIGURE 42. TIP OF FINGER PRESSING ON EMINENCE AND ON SULCUS The plane of this diagram is halfway between the coronal and sagittal.It is, perhaps, the most important diagram in the book for the reader entirely to understand, for it is the ability to put the finger in this position which enables one to make the clinical diagnosis of rupture of the supraspinatus tendon. The dotted line represents the contour of the bursa. Compare this with Figure 44, which shows the contour of the bursa when filled with the calcified material, and also with Plate II, Fig.3, which shows a large calcified deposit in exactly the situation in which the rupture lies in this diagram. In this one the sulcus is immediately under the tip of the finger and the' eminence just external to it, but in Figure 3 the eminence would be just under the finger. Therefore, as explained on page 148, the tender point in a case of rupture is represented by a depression, but in cases of calcified deposit, by an eminence at the corresponding position.
(12) The sulcus is just about big enough to be filled by the tip of the finger, as indicated in the diagram. It is nearly always found to be larger at operation than one would guess from palpation before incision.
(13) The eminence is an eminence only by contrast with the sulcus. It consists of normal tuberosity with perhaps a remnant of the tendon attached to it. In elderly men without injury to the shoulder one can often feel the tuberosity because the tendon is more or less atrophied, so that at times it is hard to be sure whether the tendon is torn or merely atrophic. However, in most cases of ruptured supraspinatus the eminence is conspicuously large and one is quite sure of its existence. It is well to say here that the eminence which is found in cases of calcified deposit is not on the tuberosity itself, but proximal to the tuberosity in the tendon at just the point where ruptures so often occur. Furthermore, the tenderness is usually greater on the eminence in cases of calcified deposit than it is on the eminence in the cases we are speaking of.
(14) As may be seen under Pathology, the supraspinatus is nearly always torn if any of the other short rotators are, but it is very common to have portions of the adjacent tendons torn, so that the tenderness, eminence and sulcus may be a little internal or external to the mid-point of the insertion of the supraspinatus itself. This latter may be determined pretty accurately by placing the forearm in flexion and drawing a line from the mid-point of the flexure of the elbow to the mid-point of the head of the humerus. The bicipital groove lies about its own width external to this line, and the supraspinatus is on the top of this line and to the outer side of it for about three-quarters of an inch. The insertion of the infraspinatus is just external and also partly in front of that of the supraspinatus, for, as explained in Fig. 6, the two insertions nearly cross each other. The insertion of the teres will be found nearly exactly on the mid-point of the head of the humerus on its outer aspect. Be careful, in determining this, that the forearm is flexed at. the elbow and held straight forward. The insertion of the subscapu-laris can be determined by putting the arm in the anatomic position and placing the examiner's forefinger just external to the tip of the coracoid process, which is always palpable, as shown in Fig. 6.
(15) The jog is noticeable to the patient himself, and sometimes is visible as well as palpable to the examiner.
(16) The patient nearly always winces as the jog occurs, but in long-standing cases he may not do so.
(17) The soft crepitus is not like the crepitus in fractures. It is of a more velvety, gristly character. When one has become familiar with it, it is easily distinguished from the kind of crepitus often found in the shoulders of old working men, which resembles the crepitus one frequently feels over the prepatclla and olecranon bursas and about the other joints.
(18) When the sulcus, eminence and tender point have once passed beneath the acromion as the arm is elevated, there is a sense of relief on the part of the patient which is usually apparent in his countenance. When the arm is almost fully elevated (there is often so much fluid in the joint and bursa that absolutely complete elevation is not attained), the patient is relatively comfortable. His pain will appear again when flexion occurs at the level of the shoulder, after the arm has descended with humerus and scapula locked, to a horizontal position. At this time the jog and crepitus are usually again palpable. As this occurs the patient leans toward the affected side and lowers the whole arm quite suddenly. These eighteen symptoms must be present soon after the accident, but the difficulty is to estimate the degree of the rupture at this time. Partial ruptures must give much the same symptoms as complete ones at this stage, and the degree of spasm must vary, as well as the courage of the patient as he makes a voluntary effort to raise the arm. Immediate diagnosis cannot be easy at this stage. However, the progress of the case makes the diagnosis easier and easier, although valuable time elapses. If exploration is not done these symptoms remain the same and the following points in the course of the case will tend to confirm the diagnosis.
Character of Pain. Practically every patient whom I have seen has given the history that during the first few nights after the accident the pain was severe or intense. Gradually this severe pain changes to a nagging, annoying one, sufficient to greatly interfere with the night's rest, but bearable without drugs. It is usually located near the deltoid insertion far below the actual lesion. Pain of this character continues week after week and with but little change for many months. It is aggravated by the attempt to work, and the patient's resistance to it is gradually lowered as he becomes more and more worn out by restless, painful nights. I am convinced that this pain is very severe as well as prolonged, for I have heard many strong laboring men state that they have never suffered such pain in their lives. It is more the persistence of it than the pain at any one time which wears them out. They often say: "If I could only get a good night's rest I could work during the day." Practically they find that working during the day gives them bad nights, and therefore nearly all of them, in spite of their courage, give up work after a time. Of the series of a hundred cases, only eighteen stated that they had worked for even a brief period. They say that they may go to sleep for a while, but wake with pain in the shoulder or in the region of the insertion of the deltoid, and that they have great difficulty in getting the arm into a comfortable position again. When they do, they go to sleep only to wake up in a few hours for another change of position. Sometimes they get up and walk about or apply hot water bags or other household remedies. It is very characteristic of these cases to have complaint of pain out of proportion to the physical signs, and therefore they receive little sympathy.
Atrophy of the spinati, as shown by prominence of the spine of the scapula, always occurs after these injuries, but does not appear for about three weeks. After it has once appeared it persists, and is apparent for a long time even in the operated cases. In very few of the cases that I have seen years after the injury was it absent. The atrophy may be more conspicuous in the infraspinatus, which is the larger muscle. Whether the fact that the infraspinatus is always also atrophied, is due to the crossing of its fibers of insertion with those of the supraspinatus so that they are always also torn to some degree, or is due to the fact that the two muscles are supplied by the same nerve, i.e., the suprascapular, I do not know, but it is a fact that atrophy of both is a constant sign. Of course atrophy of these muscles occurs in any chronic condition of real severity affecting a shoulder joint, so that the presence of atrophy does not necessarily indicate this diagnosis, but its absence would he strong evidence against it. In a few long-standing cases I have seen only a small amount of atrophy. It is usually very pronounced. As a rule the deltoid is not much atrophied and may even be hypertrophied. The general condition of the patient is a factor in diagnosis, for he gets into a vicious circle. He is out of work so that all the muscles of his body become enfeebled. He often cannot afford good food, and he may, therefore, be ill-nourished. Add to this the constant depletion of his energy from restless, painful nights, and we may readily account for the fact that while previously he was a strong, healthy man, he now appears haggard and unhappy. The mental condition also is poor, for worry on account of inability to work, and that he may never be able to work again, is enhanced by the fact that the physician he consults is unable to tell him the cause of his trouble, and all attempts to relieve him by ordinary remedies absolutely fail. Seeing these cases months after their accident, I am frequently told, "Nothing they have done has done it any good." The actual physical deterioration from worry is still further aggravated by the doubt that is thrown on their veracity by the physicians employed by the insurer. Usually by the time they are sent to see me some months later, their attitude of mind is defensive, and they at once begin to express their disgust with being told that they ought to go to work and think less about the pain. This attitude of mind becomes still worse when they are actually accused of hysteria or malingering. They say they want to work. "Do you think I would lie around like this if I could earn $24.00 a week?" They become embittered at their treatment by society in general in spite of the fact that they may still be receiving their compensation. At length they may lose their self-respect, and brooding over their hard luck take to drink. My second patient was such a case. He had had a good job which he enjoyed; after his injury became discouraged, and evidently decided to let things go and to use up what money he had saved, in drinking as much as he had a mind to. The person for whom he formerly worked, instead of losing sight of him, looked him up, and, realizing that he must have some real trouble with the shoulder, sent him to a doctor who referred him to me. The result of the repair of his tendon was not only that he was able to work, but that he refrained from drinking and worked for ten or more years for the same people who formerly employed him. Unfortunately the attitude of the relatives of such an old man with a disabled shoulder is apt to become somewhat like that of the doctors who have been unable to diagnose and relieve him. His own family after a while get to think of him as a burden, and since they can see nothing the matter, such as a limp or a deformity, are inclined also to think that he has "laid down" before his time. In recent years, however, we see more signs of sympathy, for the compensation such patients may receive will perhaps be the chief support of the family. Undoubtedly many such cases eventually turn up as recipients of charity and eventually die in state institutions. It is not surprising to me that the material reported in this book, which was accumulated by Dr. Akerson at a hospital for the indigent, shows such a high percentage of instances of these lesions. I would venture to predict that if one should see the patients who are chronic nuisances to industrial insurance boards, and the physicians connected with the administration of compensation for industrial injuries, most of those complaining of shoulder disability would have this particular lesion.
Some patients may continue to work. There are rare individuals who, in spite of the disability, have the courage and otherwise sound health to continue to work in spite of the soreness, awkwardness, loss of power, and painful and restless nights. About one-fifth of my series attempted to work for a time before they gave in and sought compensation. I have no doubt that there are others who have never given in. This is a lesion which tries a man's character, and, since it usually occurs in later life, is often the cause of permanent incapacity, for even if the use of the arm returns in good measure at the end of a year, the patient's habit of work has been destroyed, his muscles have become soft. If he has the courage to go to work again, he will find it difficult to get a job. Those courageous men who do work in spite of the lesion, become more or less free of serious symptoms in from two to five years. As has been explained under Pathology, compensatory changes take place so that the eminence absorbs, the sulcus partially fills, and an excess of fluid allays friction. After several years even the night discomfort disappears, and weakness in abduction, atrophy of the spinati, friction rubs, the fluid sign and occasional pain in certain positions may be the only aftermaths of the injury.
Hypertrophy of the Deltoid. Perhaps it would be better to make this heading "well-developed deltoid as contrasted to the spinati," for the hypertrophy is not striking except when compared to the condition of the spinati. It is a fact that, in the long-standing cases, the deltoid itself is as well developed, or even more so, than that of the other side. I explain this because it has to do most of the abducting work of the arm unaided by the supraspinatus. It not only misses its help, but acts at a disadvantage as explained in Fig. 3. Hence it retains its development or even hypertrophies. My third case had a deltoid like a ham, but at the end of five years he could only feebly perform abduction and could not raise even a slight weight in that hand above his head. He had refused operation.
The Fluid Sign. Among the auxiliary signs and symptoms I find some help from what I call "the fluid sign." I had studied shoulders for many years before I realized how fluid in the true shoulder joint behaves. When the arm is by the side, the fluid sags in the relaxed axillary portion of the capsule. When the arm is elevated the axillary portion of the capsule is stretched tightly below the rounded head of the bone, and the fluid is driven upward where the capsule is now relaxed. In case there is a rupture of the supra-spinatus tendon, the fluid is forced through the gap and distends the bursa in the subdeltoid portion beneath the upper fibers of the deltoid. Stand behind one of these patients, who is holding both arms as straight as he can toward the ceiling, and you will see that the contours of the two shoulders are quite different. When there is a considerable amount of synovial secretion, absolute complete elevation of the arm is prevented by the mass of fluid. Another interesting point is that when there is fluid the friction is largely prevented as the arm is elevated. When it subsides pain reappears. This phantom improvement by the formation of fluid is not uncommon. Patients who continue to work in spite of their pain develop fluid, as do people with various affections of the knee. The fluid continually pumping in and out of the bursa dilates it and a true hydrops may result (p. 478). One finds in long-standing cases that the bursa is very large. (See case Fig. 44.) Some fluid, from a dram to an ounce, is a constant operative finding in these cases. It may not be noticed when the bursa is first opened, but if one elevates the arm and puts the axillary portion of the capsule on the stretch, the thick, straw-colored fluid runs out of the wound. Sometimes there is enough to distend the bursa even in the anatomic position, and when the first incision into the bursa is made, it obscures the field and has to be sponged out. This behavior of the fluid was forced on my attention when I used to put the arm in abduction after suture. This caused the weeping wounds described on p. 248, and this serious and annoying complication led me to reason out the facts.
INCOMPLETE RUPTURE
Although there is no sharp anatomic distinction between complete and incomplete rupture, there is the practical one that cases of the former will not recover completely unless the tendon is sutured, while cases of the latter may heal in a natural manner. One which is typically complete involves the whole supraspinatus tendon, with perhaps parts of the adj acent tendons. One which is typical of the incomplete form need neither involve the whole width nor run through the whole thickness of the tendon. In its minimum phase it may be only an evulsion of a few fibers from the tuberosity; in its maximum phase it would be a borderline case of complete rupture. In its acute phase it may be definitely due to trauma; in its chronic phase the tendinitis overshadows the traumatic history. The reader who has the patience to finish this book will inevitably remain confused about the lines of distinction which I have attempted to draw among the six most common clinical entities which affect the shoulder, i.e., complete and incomplete tendon ruptures, rim rents, calcified deposits, tendinitis and arthritis. In fact, I must leave the reader puzzled, for I am still puzzled myself. I can only confront him with the puzzle—show him that there is a puzzle. Personally, I believe that these rim rents and incomplete ruptures are the cause of the great majority of sore shoulders, and yet I believe they usually occur in degenerated tendons. For example, a man might have degenerative changes in both shoulders without symptoms and then, after trauma to one tendon, have severe local symptoms without any signs of trouble in the other shoulder. One cannot even divide complete and incomplete lesions by the criterion of whether or not there is a direct communication from the bursa to the joint through the rupture, for the size of the opening is important also. Yet splitting hairs on a definition is not worth while. Practically, it is convenient to say that when one opens the roof of the bursa and finds the cartilage of the joint exposed to view through a rent in the floor of the bursa, we are dealing with a complete rupture. If there is no communication at all or only a small hole in the base of the bursa, we would class the case as incomplete. Of course the persistence of a direct communication between the joint and the bursa, even if small, is a most important point, because it alters the mechanics, as indicated on the cover of this book. Yet the size of the hole is also important if it is large enough to permit erosion of the joint cartilage (Plate VII, Fig. 8) by friction on the acromion. It seems to me highly probable that incomplete rupture is much more common than complete. Since I have only operated upon cases where very pronounced symptoms existed, I have naturally found many more instances of the complete form, but in my observations on the cadaver, or on living cases in the clinic, I have much more often found incomplete lesions. I have not kept a numerical account and therefore cannot give the exact number or even the proportion. Dr. Akerson's statistics give the best measure we have, but are subject to the criticisms on page 65. Similar observations may be made by any one having access to autopsy material. Moreover, when the economic importance of this lesion is appreciated, and the principles of efficiency become applied to the practice of medicine, such observations must be made. I am inclined to think the table on page 469 also gives a low proportion of the incomplete ruptures, because so many cases in the other classes probably had this lesion besides the lesion which caused their classification. For instance, rupture of the supraspinatus is a not uncommon complication of dislocation and of circumflex paralysis, and many of the minor unclassified cases may have also been instances of this lesion. On the other hand, I have usually found at operation that the rupture was more extensive than I had previously thought, so that a good proportion of the supposed incomplete type may have been complete. Referring to the chapter on Pathology, it will be seen that incomplete ruptures of four kinds are described: (a) A few of the lower fibers on the joint side, together with the synovial reflection, may be torn out; these I call "rim rents." (b) Some of the central fibers may be parted without tearing either the joint side or the bursal side of the tendon. (c) The rupture may extend vertically through the whole tendon, making a communication between the joint and the bursa, without involving the whole breadth of the tendon. (d) The fibers on the bursal side may be eroded without complete communication with the joint. I believe that type (a) is synonymous with the cases so frequently found at autopsy where the sulcus is bare and eburnated, i.e., the condition I speak of as "rim rents." I think that type (b) may be the precursor of calcified deposits. Types (c) and (d) may be among the cases which give "tendinitis" symptoms out of proportion to the traumatic history. Since I do not intentionally operate on incomplete ruptures, what I have to say in regard to these minor lesions is more theoretic than what has been stated concerning the complete ruptures. All four varieties should be distinguished from the complete form by the persistence of considerable power in elevation, because the mechanics of the pull of the supraspinatus are not greatly altered. I have not operated unless there was decided loss of power. The other cardinal symptoms, jog, crepitus, atrophy, sulcus, eminence and local tenderness, will be present, although any one of them or all of them may be found in less pronounced degree than in the complete cases. Type (c) might be recognizable, as the fluid sign should be present because joint and bursa communicate. The diagnosis of the incomplete type is therefore made chiefly by the persistence of a considerable amount of power in the elevated or abducted arm and some doubt about the presence of some of the other symptoms and signs. Complete cases are usually so absolutely typical that no doubt remains. Complete cases do not form adhesions, while many incomplete cases do. If the surgeon is sufficiently informed about the anatomy, pathology and surgery of this particular region, I believe that when in doubt he should explore the bursa through a half-inch incision. If he finds a communication through into the joint, let him close it, but if no opening exists, let him back out, for we do not yet know what to do to these incomplete ruptures. Before closing this chapter, I may say that I believe these lesions to be the most common form of shoulder injury. My slogan has been that complete rupture of the supraspinatus is the most common cause of prolonged disability from industrial accidents to the shoulder. I feel that I have proved this at least to my own satisfaction. I may now add that the incomplete form accounts for the majority of minor shoulder disabilities. This I have not proved, for I do not operate on these cases, but the frequent presence of broadened sulci found in any .series of autopsies in elderly people is convincing to me. The clinical examination of employees with sore shoulders often shows symptoms suggestive of this lesion. Possibly opaque fluid injected in the joints might confirm the diagnosis. I have not felt justified in doing this, for exploration seems to me quite as free from danger. I certainly should try this experiment on patients now if I had in mind some definite plan for relieving them, if I did find broadened sulci indicative of incomplete ruptures, but I do not yet conceive of a plan by which to promptly cure them. The appearance that I think opaque fluid in the joint would show in cases of complete rupture is indicated in the cover design.
FREQUENCY OF COMPLETE RUPTURE OF THE SUPRASPINATUS TENDON
There are certain reasons for believing that this is a far more common lesion than is generally appreciated. 1. The writer's personal experience. 2. The statistics of Dr. Akerson. 3. The lack of attention paid to lesions of the shoulder in general; i.e., of end result studies of large series of shoulder injuries.
1. Personal Experience. The above chart shows that the writer's experience in operating upon these lesions was confined to two periods of about three years each, when attentive study was given to relatively large groups of shoulder cases. In the first period (1911 to 1913 inclusive) an intensive study was made of the shoulder cases at the Massachusetts General Hospital. The author resigned from that hospital in 1914 and was not reappointed until 1929. Other activities and a period in the army during the war intervened, without opportunity to operate on such cases, although I continued to make occasional impartial examinations for the Industrial Accident Board. In 1926, owing to the interest of Dr. Henry C. Marble and Dr. W. A. Bishop, who are directors of Insurance Clinics, I again gave intensive study to a group of shoulder cases, and the chart again ran to a peak. This led to increased interest in other clinics, so that other surgeons (e.g., Dr. Wilson) began doing these operations, which accounts for the decline at the end of my chart, although the rate of frequency, if we included other surgeons' cases, would not show this decline. In other words, the chart shows that whenever I gave intensive study to a group of shoulder injuries, I was able to diagnose some of these cases and to demonstrate them by operation. My work received little attention after the first period but since the second, largely owing to the changes brought about by the Workmen's Compensation Laws, the importance of the lesion is becoming recognized by industrial surgeons in this state. I do not know just how many cases were seen during these two periods, and therefore cannot give the exact percentage of the cases examined which were instances of this lesion, although the limits may be stated pretty positively. For instance, the first fifteen cases were found among less than 200 patients, and the second fifteen cases were from an uncertain number, but probably less than 100. This means that the frequency of occurrence was about 7%% to 15% of all shoulder lesions that came under my observation. By referring to my records for the twenty years since I recognized the first case, I find that I have seen in all about one thousand shoulder cases. Of these more than one hundred have been positively diagnosed as instances of complete rupture and many more as incomplete. This would justify an estimate of between 10% and 20%. It would require an amount of labor disproportionate to the present object to go over these records to apportion the exact percentage, since it is sufficiently clear that I have made this diagnosis in not less than 10% and perhaps more than 20% of all shoulder cases. If cases of partial rupture were included the percentage would be at least doubled. The figures in the annual Reports of the Industrial Accident Board help us only in a negative way, for this diagnosis is not classified. Their tabulations of the durations of disability are not carried over from year to year, so that we cannot obtain a list of the cases in which disability is protracted. This is unfortunate, for this list would probably be largely composed of cases of rupture of the supraspinatus. The report of the Industrial Accident Board for the year 1928, Table 7, gives the following figures in regard to shoulder injuries. It is supposed to cover every accident occurring in industry in this state.
The last two columns, "Sprains and Strains," and "All Other," are the ones which would probably contain most of these ruptures, although a large number must be included under dislocations and fractures. If we double the figures where both shoulders were injured, the total of the two columns would be 748, five per cent of which would be thirty-seven. During the same period, July 1, 1927, to June 30, 1928, I personally made the diagnosis in seventeen cases which were referred to me by Insurance Clinics or by the Board for "Impartial Examination." Since I probably see but a small fraction of these shoulder injuries of doubtful diagnoses which occur annually in this state, the estimate of thirty-seven is surely a minimum one. The maximum reasonable estimate would double this and also include twenty-five per cent of the 125 dislocations. It seems to me pretty well proved that not less than thirty-seven and very likely more than one hundred injuries of this type occur annually among Massachusetts employees. At first sight thirty-seven, or even a hundred, neglected shoulder injuries in a state of 4,200,000 inhabitants does not seem a very serious matter, but as each insured case may cost the state $4,000 for compensation (aside from the pain endured and the economic loss of productive effort in labor), the amount of money involved is considerable (37 X $4,000 = $148,000). This fact mates this obscure injury more interesting, and, if we multiply by 100, still more so. My opinion is that the larger figure is a more accurate estimate. If we included partial ruptures which heal after a few months, but which cause a large total of lost time, the annual expense to the state for injuries of this small tendon can be reasonably estimated to be over half a million. Furthermore, there must be many such injuries which are not industrial. In addition to the above reasons for believing that this lesion is not rare, I may say that in a single set of twenty dissecting room subjects I have always been able to demonstrate one or more instances. When I have been asked to speak to small groups of doctors or students, I have usually been able to find a subject on whom to demonstrate the diagnostic signs of this lesion, by asking at adj acent clinics for cases complaining of inability to raise their arms. I feel quite confident that I can demonstrate (recognized or unrecognized) instances of this lesion by examination of the cases under treatment in the out-patient departments of any large general hospital in any city of the United States, and, in fact, probably in most parts in the world, where there are many persons over forty doing laboring work. This does not necessarily mean that there are large numbers, for each case is apt to be a patient for several years, meanwhile going from one hospital to another in search of relief. 2. Dr. Akerson's statistics, already given on page 67, give us a maximum estimate, because nearly all the observations were made on elderly subjects of the laboring class, in whom a previous injury could only be assumed, for there were no histories negative or positive of accidents. There is a splendid chance for a clinical research at the Long Island Hospital, in future, to correlate autopsy findings with retrospective histories of shoulder injury, taken from patients before death comes. It would be a time-consuming job, but it would help us to decide the important question of whether these lesions can occur without injury, and it might lead to the saving of many thousands of dollars, not only in compensation, cost of medical care and economic loss, but in maintenance of the indigent. Dr. Akerson's work might in this way lead to a saving of more than the cost of his entire department. Similar opportunities exist in like institutions from one end of the country to the other. 3. The Lack of Attention to Shoulder Injuries. There is a voluminous literature on fractures and dislocations (especially on habitual dislocations) of the shoulder, but, with the exception of Dr. Meyer's work (loc. cit.) and an investigation now being undertaken by Dr. Fowler of Evanston, 111., I know of no systematic observations from autopsy findings in this part of the body. Nor are there any serious studies of similar clinical cases. If the End Result system of organization existed in our hospitals and insurance clinics, these cases of prolonged disabilities would be automatically revealed, studied and eventually prevented by early operation. Thus my confidence that these lesions are common is enhanced because no one has evidence to. contradict me, and a few support me. It is clear that Dr. Meyer finds similar lesions, although he explains them as the results of attrition. Dr. Fowler will, I believe, as he has already told me, confirm some of my findings and give support to those of Dr. Akerson.
ARGUMENT
This book is not written to show that I have had good results in this class of cases. My argument is merely that this lesion exists; is not uncommon; has characteristic symptoms which permit accurate diagnosis; and, since I have been able by suture of the tendons to greatly relieve a few cases, even though the diagnosis was belated, it is highly probable that the prolonged and trying symptoms from which these patients suffer, when not operated upon, might be prevented by early diagnosis and the prompt use of a minor surgical operation, which should not be difficult, if promptly done. If I can offer reasonable evidence for the clauses italicized, it seems to me that the conclusions in the last clause of the above paragraph would be sustained sufficiently to justify prompt exploratory operation when the symptoms suggest this diagnosis.
POSSIBLE ACCURACY OF DIAGNOSIS
I have already established the existence of this lesion, endeavored to estimate its frequency and have described the characteristic symptoms. Evidence is now offered to sustain the statement that accurate diagnosis is possible. The following extracts, taken verbatim from my pre- and post-operative reports to insurance companies, show that a'positive diagnosis of this lesion may be made. Every case operated upon during the last sixteen years, in which I have demonstrated a complete rupture of the supraspinatus, is given. Even in the cases operated upon prior to 1916, one may find that my definite pre-opera-tive diagnoses in the records of the Massachusetts Hospital are correct, in all but five cases in which the diagnosis was simply " subacromial bursitis." With each of the abstracts given below the case number is stated. The reader will find further information about each of these cases by referring to these numbers in the Table on pages 255 to 260 in Chapter VIII.
CASE No. 57. Preop. Diag. "The injury which he sustained two years ago, I believe to have been a rupture of the supraspinatus tendon and the upper portion of the capsule of the shoulder joint." Op. Findings. "As soon as the bursa was opened it was apparent that the entire supraspinatus tendon had been torn away, for the cartilage of the bone showed where the supraspinatus tendon should be. A small stub of the tendon still remained attached to the tuberosity. Further exploration showed not only that the supraspinatus tendon, but the upper portion of the infraspinatus tendon was also torn, but the subscapularis was intact. The long tendon of the biceps could be seen crossing the field just at the edge of the subscapularis. The proximal portion of the supraspinatus had retracted so far into the subacromial space that only a rather unsatisfactory portion of it could be pulled upward and attached to the stub on the tuberosity. It was evident that the atrophy which had taken place in the two years left practically no hope of the restoration of the complete function of the muscle or tendon."
CASE NO. 75. Preop. Diag. " I have no hesitation in making a diagnosis of rupture of the supraspinatus tendon, nor in advising an operation to suture it and clean off the ragged vegetations at the edges of the old rupture." Op. Findings. " Showed supraspinatus entirely torn off and retracted far under acromion. Biceps tendon lying at inner edge of rupture."
CASE NO. 88. Preop. Diag. "I feel that the diagnosis of subacromial bursitis is correct, but that the underlying cause of the bursitis was a ruptured supraspinatus tendon. This has now partially healed—enough to renew the power of abduction but not enough to make the point of rupture smooth. The result is an irregularity on the base of the bursa which in abduction impinges on the acromion and acromio-clavicular ligament." Op. Findings. "On opening the bursa the ruptured supraspinatus tendon was beautifully demonstrated, the tendon having been torn from the tuberosity, leaving none of the original attachment on the bone. It had retracted about a half inch and the torn end could be seized with a tenaculum."
CASE NO. 88. Preop. Drag. " He has the following signs indicating that his trouble is a ruptured supraspinatus tendon and his history is typical of this lesion. "1. There is an acutely tender spot on the greater tuberosity at the normal point of insertion of this tendon. "2. I can, I believe, feel at this point a sulcus where the tendon is torn. "3. There is a painful jog in the motion as he raises his arm. "4. There is velvety crepitus as he does this. "5. After the arm has been elevated one can easily pull it down, although the deltoid muscle can be felt strongly contracted. "6. There is a feeling of fullness under the upper part of the deltoid as if there was fluid in the bursa." Op. Findings. "Free straw-colored fluid. Cartilage of head of humerus and the greatly swollen and injected biceps tendon visible on retracting the margins of wound in deltoid. The tear of the supraspinatus tendon was complete and the tendon of the infraspinatus was also almost completely torn. The proximal ends had retracted so as to be barely reached by Allis forceps to enable passing a suture."
CASE NO. 89. Preop. Diag. "Patient presents to me typical symptoms of supraspinatus. He can abduct his arm slowly and with a hitch which gives an obvious sudden change in the relative position of the humerus and the scapula. He cannot maintain his arm extended against any considerable pressure." Op. Findings. "Routine bursal incision disclosed a very extensive tear of the supraspinatus tendon. The biceps tendon had disappeared and could not be located except possibly as a few fibers in the anterior part of the joint."
CASE NO. 96. Preop. Diag. "Examination shows pretty typical signs of a ruptured supraspinatus tendon, except that the friction rub is masked by the presence of joint fluid in the bursa. The outlines of the bursa are visible through a heavy deltoid as evidence of this fluid. It is well shown when the patient attempts to abduct the arm. The arc of abduction cannot be performed without a typical jog in the motion. The patient himself feels this and complains of pain during it. There is tenderness over the bursa." Op. Findings. "Routine bursal incision showed a typical rupture of the supraspinatus tendon which did not involve either the subscapularis or the infraspinatus; making a gap pulled away from the tuberosity of about one-half inch width. Through this, on opening the bursa, the cartilage of the head of the humerus was visible. By retracting a little, the biceps tendon could be seen to the inner side, greatly congested."
CASE No. 97. Preop. Diag. "Diagnosis. Rupture of supraspinatus tendon (left) complete and of severe grade. The same on right but incomplete and partially repaired. Probably rupture of the long heads of both biceps tendons." Op. Findings. "The supraspinatus tendon was completely ruptured -and the upper portion of the subscapularis also. The biceps tendon had disappeared, evidently having been torn off the glenoid and retracted into its groove."
CASE No. 98. Preop. Diag. "Examination shows very typical tenderness, crepitus, abduction weakness and the jog in motion typical of a ruptured supraspi-natus tendon in the right shoulder." Op. Findings. "Routine bursal incision showed the supraspinatus was completely ruptured and also a part of the tendon of the subscapularis over the biceps tendon, and also a portion of the infraspinatus. The joint cartilage was exposed for about a half inch to the outer side of the bicipital groove and there was a tag of tendon still attached to the tuberosity just external to the groove."
CASE No. 102. Preop. Diag. "Examination shows a decided atrophy of the muscles about the right shoulder, tenderness and irregularity of the tissue over the greater tuberosity, a painful jog in the motion of abduction, free external rotation, persistence of passive and loss of active complete abduction. These signs and the history are characteristic of rupture of the supraspinatus tendon. He also has' a rupture of the long head of the biceps, if one may judge by the contour of the belly of the muscle." Op. Findings. "Free joint fluid found in bursa, which was large. The supraspinatus tendon was about half torn away from the tuberosity and the torn tendon retracted only about one-half inch, exposing a small extent (about) one-quarter inch of the edge of the joint cartilage. The opening was not large enough to view the tendon of the biceps, so I made an incision about one-half inch long into the bicipital groove and identified the biceps tendon. It was large and normal in appearance, so that it is likely that the apparent atrophy of the outer belly of the muscle in this case was due to simple disuse from reflex pain."
CASE NO. 106. Preop. Diag. "Examination of the right shoulder shows typical signs of a rupture of the supraspinatus of considerable degree. One can feel the sulcus on the facet of insertion from which the tendon has been evulsed. There is fluid in the bursa." Op. Findings. "The roof of the bursa was thickened. When incised, free straw-colored fluid escaped, about one dram. The supraspinatus was found torn from its attachment and retracted far under the acromion. About one-half of the insertion had evulsed from the facet. The other half was torn about one-half inch from the facet, leaving a thickened, irregular, whitish mass about the size of a large lima bean attached to the tuberosity."
CASE No. 107. Reported in text.
CASE No. 108. Preop. Diag. "The diagnosis is fairly certain of a partial rupture of the supraspinatus, and also a rupture of the long head of the biceps." Op. Findings. "The complete supraspinatus tendon had been torn close to the tuberosity and was retracted about an inch and a half. The infraspinatus and subscapularis were intact, but the biceps tendon had been torn completely off the glenoid and had retracted part way, instead of wholly into the sheath, leaving a frayed end protruding at the edge of the articular surface. In repairing I used this by sewing the supraspinatus to it and the subscapularis, anchoring the biceps tendon in its groove as I did so."
CASE No. 112. Preop. Diag. "Examination shows the following: A slight atrophy of the intrinsic muscles of the shoulder, a soft crepitus which occurs with a snap just as the tuberosity passes under the acromion in abduction, a tender point on the greater tuberosity at the insertion of the supraspinatus tendon, a tendency of the scapula to follow the motions of the humerus, a flaccid condition of the outer head of the biceps muscle. These signs indicate that he has torn the supraspinatus tendon from its attachment on the tuberosity, and probably has also torn the biceps tendon from its adjustment on the glenoid." Op. Findings. "This displayed a perfectly typical complete rupture of the supraspinatus tendon without rupture of either the subscapularis or infraspinatus. The biceps tendon was slightly frayed at its inner edge where there were two small papilloma-Iike, whitish excrescences, the size of one-quarter of a pea. The stub of the ruptured tendon was still attached to the tuberosity, but had worn down to a falciform edge; similar falciform edges showed on the lateral aspect of the tear; i.e., the unruptured edges of the subscapularis and infraspinatus. By lifting the edge towards the subscapularis, a pinkish, inflamed biceps tendon was demonstrated. A few fibers of the outer portion of this had been ruptured as spoken of before. There was only a moderate amount of joint fluid seen at any time. The edges of the torn surfaces were refreshed, and the parts sutured in place with three heavy braided silk sutures."
CASE No. 115. See history on page 389
CASE No. 119. Preop. Diag. "Typical ruptured supraspinatus tendon. Atrophy, crepitus, jog, fluid, loss of power very great. Biceps O. K. Rotation free, tender sulcus." Op. Findings. " The tendon was much thicker than usual and less retracted, so that the triangular gap was longer transversely than vertically. . . . There was quite a stub on the tuberosity, enough to suture. The biceps tendon was so badly damaged that there were but a few strands of it left and these were adherent to the roof of the joint. Most of the tendon had retracted into the groove and become adherent there. None was left crossing the joint surface and none was seen in the joint, although it might have been imbedded there behind the head."
CASE No. 123. Preop. Diag. " This patient has the typical symptoms of a rupture of the supraspinatus tendon of considerable extent, but not enough to prevent his having a fair amount of power in abduction—although with pain. He has atrophy of the spinati, scapulo-humeral spasm, a j og in the motion of abduction, the fluid sign with limitation in complete abduction, a tender, palpable defect on the greater tuberosity where the tendon should be attached." Op. Findings. "An exploratory incision a half inch long was first made and it was at once apparent that the supraspinatus and the infraspinatus tendons were evulsed from their facets, leaving no stubs of tendon. The biceps tendon, which was double at this point, was greatly swollen and inflamed and presented as soon as the roof of the bursa was opened. To its inner side the subscapularis and the inner portion of the tendinous expansion of all the tendons lay intact, and to its outer side was bare joint cartilage and the top and posterior portion of the greater tuberosity from which the tendons had been torn. The facets were smooth and the superficial parts of them had not been carried away by the tendons. The incision was enlarged to an inch and a half and a good view of the field obtained. It was found that the teres minor had also been evulsed. The whole posterior part of the capsule and conjoined tendon of the above muscles was retracted downward and outward. It was impossible to draw this back and to suture it in place."
CASE No. 127. Preop. Diag. "At my first examination I did not make the diagnosis in this case, although it had been suggested by Dr. Marble, but on my second examination, seventeen days later, I wrote, 'H--- is better, but I have changed my opinion about the diagnosis. I am now quite confident that he has a ruptured tendon and should be operated upon. I think Dr. Marble was correct in his original diagnosis.' " Op. Findings. "A small exploratory incision was first made over the point of tenderness. As soon as the roof of the bursa was incised, an irregular, whitish mass of tendon about as large as a thumb nail popped out of the incision. It proved to be the proximal portion of the torn tendon and was about one-quarter inch thick. It evidently turned on itself as the arm was abducted and caused the catch which the patient himself could accurately localize, There was about a tablespoonful of straw-colored fluid in the bursa. The incision was then enlarged to about two inches and a good view of the lesion obtained. This case differed from others on which I have operated in that the tear did not involve the whole thickness of the tendon, but left a very thin layer toward the joint surface so that there was not a demonstrable communication with the true joint. However, the layer was so thin that the cartilage could be seen through it. The ruptured portion formed a little flap about a square inch in extent, attached only to the proximal end and evulsed on the distal end from the facet of insertion. I have seen similar cases in the cadaver where the distal end had not evulsed. It is a fact that lamination of the tendon is found in many cases, but this is the first one on which I have operated where the laminated portion evulsed without the lower surface also tearing. The free portion seemed rather necrotic but was clearly rather recently ruptured. The torn surface was rather bulbous, as if partially healed. Near the lesion and to its inner side was a streaked, red area which was excessively tender when touched, but the torn end itself had no sensation and was not so made by the novo-caine. It is to be assumed, therefore, that the pain in these cases is not due to the tissue pinched but to the uninjured tissue on the tuberosity which does the pinching."
CASE No. 128. Preop. Diag. " My opinion is very strong that he has a ruptured supraspinatus, but I am a little uncertain as to whether it is not a renewed injury in an old lesion. X-ray is very strong evidence of this. Clinically, I should not suspect it. In either case I should advise immediate operation as soon as arrangements can be made." Op. Findings. "On opening the bursa there was found to be evidence of old inflammation in the bursa, as well as recent light adhesions. The supraspinatus was torn away from the tuberosity to the extent of about one-half inch, and little of the bursal floor remained untorn, but there was a gap directly into the joint through which the cartilage could be seen. This gap was about one-quarter of an inch in extent. The tendon had retracted very little and I was able to close it with four silk sutures, two of heavy silk and two of light silk."
CASE No. 129. Preop. Diag. "Signs of ruptured supraspinatus tendon were present at my previous examination, but they are much more prominent now than they were at that time. He has a very distinct crepitus, sulcus, eminence, scapulo-humeral spasm, tenderness at the border of the tuberosity; localized tenderness, atrophy of the supraspinatus, sign of fluid when both arms are elevated. I agree with Dr. Marble in the diagnosis and would advise operation in this man's case." Op. Findings. "The bursa was first opened by a half-inch exploratory incision. A small amount of free fluid escaped and it was readily seen that the supraspinatus tendon was ruptured and greatly retracted. . . . The tendon was partly evulsed and partly ruptured at the 'palisade junction.' The complete tendon was involved with possibly some of the infraspinatus. As in another recent case (H--- ) there was still some tissue remaining on the joint side so that the cartilage was partly covered with a turgid, deep-red, softish tissue containing a few obvious whitish tendinous bands. One of these was especially noteworthy because it was very sensitive, and the patient winced when it was touched. I excised it because it did not seem to be of sufficient strength to make up for its sensitiveness. The biceps tendon lay to the inner side of the rupture buried in inflamed synovial folds, but not injured, unless the strand of tendon above alluded to had been stripped off it. The bulk of the proximal end of the supraspinatus tendon had retracted far under the acromion and could barely be drawn into the field."
CASE NO. 135. Preop. Diag. " I feel very confident that he has a rupture of the supraspinatus tendon. I am not sure that there was not a previous rupture and that this latter accident merely increased the trouble. However, there is no question in my mind but that his chances will be much better if his bursa is explored and suture is done, if the tendon is ruptured." Op. Findings. "No blood or fluid on opening bursa. A complete rupture of the supraspinatus, with extension across the bicipital groove, about one-half inch into the subscapularis. Definite indications that the rupture was fairly recent; i.e., very little separation between the distal and proximal portions. Stub of tendon still attached to the tuberosity over most of its extent. No new-formed falciform edge. Biceps tendon flattened and superficially reddened in portions beneath rupture. Parts satisfactorily sutured together with pedicle silk; five stitches. In my opinion, the condition found indicated a recent rupture of a tendon which had already been partially ruptured."
CASE No. 137. Preop. Diag. "Examination shows that this patient has a symptomless, chronic bursitis, with crepitus in the right shoulder. The left shoulder shows the typical signs and symptoms of a rupture of the supraspinatus tendon. Since he has considerable power in abduction—although the abduction is painful, and accompanied with a jog and crepitus—I am inclined to think that the rupture is not extensive enough to involve the adjoining tendons. Even though this man is sixty-two, and it is four months since the injury, I would advise him to have the tendon sutured to the tuberosity." Op. Findings. "A one-half inch exploratory incision was made and the bursa opened. Rupture of the supraspinatus throughout its whole extent was disclosed. The rupture extended also, to a slight extent, into the insertion of the infraspinatus. The sulcus and tuberosity were bare, except for a very slight amount of tag of tendon near the edge of the bicipital groove. The incision was enlarged to two and one-half inches to permit suture."
ERRORS IN DIAGNOSIS
But a skeptical reader may now ask for a statement of how many cases I have operated upon under this diagnosis and have failed to find a complete rupture of the tendon. I give below a similar set of verbatim extracts from the records of nine cases during the same sixteen years, the only ones in which I have made a positive diagnosis and have not been confirmed by the operative findings.
CASE No. 76. Preop. Diag. "I believe this patient has a ruptured supraspinatus tendon, at the point of the insertion of the tendon in the tuberosity. This diagnosis is consistent with the X-ray appearances seen in the films taken by Dr. George. These films show an irregular opacity in the area of the bursa, which may be due to extravasated blood or to crumbs of bone torn off the tuberosity." Op. Findings. The operative notes in this case have been lost, but I clearly remember that the condition proved to be a case of calcified deposit which had recently ruptured into the bursa, leaving a defect in the tendon very similar to a true rupture, but containing blood and calcified material.
CASE NO. 80. Preop. Diag. "This is unquestionably a case of ruptured supraspinatus tendon of considerable extent, but the main symptoms are due to a tuft of synovial granulations from the remnant of the supraspinatus tendon still attached to the tuberosity." Op. Findings. " The walls were much thickened and there were synovial tags in the region, over the tuberosity, showing more or less chronic inflammation. The tender point, which could be felt prior to the operation and was thought to be a tag of tendon remaining on the tuberosity, proved to be a rounded elevation, markedly circumscribed and about one-half inch in diameter, slightly longer in the axial direction than the transverse. This was acutely tender when pressed on. It was incised and found to be the insertion of the tendon of the supraspinatus attached to an osteophyte at the edge of the joint cartilage. There was no direct evidence of a rupture of the supraspinatus tendon. If there had been one, it must have healed. No communication with the joint was demonstrated. The essential pathology was probably the hypertrophic arthritis which was evident in other joints. (Patient's age was 77.)"
CASE NO. 91. Preop. Diag. "The history and symptoms are typical of a ruptured supraspinatus tendon in the right shoulder, with some adhesions of the bursa, or blocking of the motion by the remains of the torn tendon impinging on the acromion. I think the latter." Op. Findings. "The base of the bursa was deeply congested and swollen, but there was no demonstrable tear of the tendon of the supraspinatus. There were light adhesions in the bursa which were broken up with the finger. The short rotators and capsule were greatly contracted and were slowly stretched until full external rotation and abduction could be attained, and the wound closed."
CASE No. 105. Preop. Diag. " I have little doubt that this patient has a rupture of the supraspinatus tendon of considerable extent." Op. Findings. " Incision through the roof of bursa with the escape of about one dram of clear, straw-colored fluid. Exploration revealed an intensely inflamed zone on the greater tuberosity, approximately the size of a half dollar with red periphery and white center, resembling the condition seen in calcified cases. An inflamed fold moved back and forth over this as the patient's arm was moved. This fold was excised. The point of the knife was used to puncture the tendon in several places in the inflamed area with the purpose of allowing a new blood supply by attaching the scar to the inflamed base. There was no indication that the supraspinatus tendon had been ruptured."
CASE No. 110. Preop. Diag. "The whole tuberosity is tender and it is hard to find a definite spot from which one can say the tendon has been torn. With the exception of this, his symptoms are fairly characteristic of a ruptured supraspinatus. From the relaxed condition of the biceps muscle and particularly of its outer head, I am inclined to feel that the biceps tendon is torn from its attachment on the glenoid. Indeed this may be the main lesion. "I should advise inspection of his bursa under local anaesthesia and suture of the tendons if they are found torn. If there is no tear in the base of the bursa, I should advise opening the joint between the supraspinatus and the subscapularis and inspecting the tendon of the biceps. "Remarks. This case is atypical in the age of the patient (17). Ruptured supraspinatus lesions are usually in elderly men. The character of the accident is unusual; sudden abduction efforts are more common as causes. There has been comparatively little pain, especially in the first week, and usually one has a history of swelling over the bursa in the first few days. Palpation over the tuberosity is a little atypical. For these reasons I cannot be as positive as I sometimes am, but I am sufficiently certain of a rupture to feel that in the boy's place I would want to have an exploration. Little harm would be done if this is negative, which I am confident it will not be." Op. Findings. "The exploratory instrument was first introduced into the bursa, which was found to be full of adhesions and consisted of a series of pockets of walled synovia. Through the exploratory instrument it could be definitely determined that the bursa had been subacutely inflamed, but that there was no tear in the supraspinatus tendon. There was no fluid in the bursa. As both Dr. Baker and I thought that the biceps tendon was probably torn, the incision was enlarged to about one and a half inches, and the bicipital groove was incised. It did not contain the tendon, which evidently had retracted downward. The arm was put through the accustomed motions of rotation and abduction while a finger was introduced into the bursa to break up all the adhesions existing there. When the adhesions had been broken, which was easily done, the motion of the arm was normal. No steps were taken to repair the biceps tendon."
CASE No. 111. Preop. Diag. "The shoulder presents typical signs of a ruptured supraspinatus tendon of a considerable degree. He has my fluid sign— characteristic velvety crepitus, a jog in motion, a tender irregularity on the greater tuberosity and weakness in abduction. He is able, however, with a little coaxing, to abduct the arm, but has very irregular action of the humerus on the scapula as he does this. There is still some ecchymosis in the anterior portion of the arm over the bicipital region, as if after the injury blood may have escaped down the tendon sheath; the tendon, however, appears to be intact." Op. Findings. "Exploration of the bursa showed no fluid. No communication was found between the bursa and the joint. The bursa was adherent over about half the extent of the lower portion. On separating the adhesions it was evident that the supraspinatus had been torn, but had spontaneously healed; the tissues were red and swollen with white patches here and there. I therefore closed the wound in the usual manner without doing anything in the way of an operation."
CASE No. 120. Preop. Diag. "The left shoulder presents very typical signs of an extensive rupture of the supraspinatus and possibly of the long head of the biceps. There is slight but decided atrophy—consistent with a history of two weeks. There is a very tender point on the tuberosity, scapulo-humeral spasm, a j og in motion and the fluid sign. In the stooping position the patient can abduct and hold the arm abducted as he straightens up." Op. Findings. "Routine bursal incision. Adhesions prevented easy access, for roof was stuck to base over an area as large as a quarter over the greater tuberosity. These were separated and showed that the tendon of the supraspinatus was bright red, swollen, and covered with tags of vascular adhesions. The line of demarcation of the affected area was very sharp on the outer side, so that the contrast between the yellowish white to the right and the turgid red at the left was very decided. It suggested an infarction. Although there was some free fluid in the bursa there was no communication through the inflamed area to the joint. The supraspinatus tendon, if ruptured at all, must have been torn beneath the base of the bursa without communicating with the bursa. Several small incisions were made with the point of the knife to relieve tension in the tendon. Through one of these a tiny bit of white nondescript tissue protruded. This was saved for pathologic examination j I am pretty sure it was necrotic tendinous substance. The wound was closed as usual without endeavoring to suture the roof of the bursa. The pathology found at this operation may be explained in two ways, or as a combination of both ways. There was certainly an acute bursitis with recent adhesions, but it was impossible for me to say positively that this localized acute inflammation over the site of the supraspinatus tendon was due to a rupture of the tendon beneath the base of the bursa. It might have been due, as suggested by the evidence of osteitis shown in the X-ray, to a chronic necrotic process in the tendon. The extrusion of the bit of necrosed tendon from the incision also supports this. So does the symptomless condition in the well shoulder. It seems to me that if we accept the man's history that the condition of the shoulder was O. K. before he helped lift the case, that the whole picture can be explained by the supposition that there was a necrotic process going on in the tendon which had weakened it so that it partially evulsed without tearing into the bursa. This would explain all which was found at the operation, and my opinion is that this theory truly does account for the facts. I have had several other similar cases and have frequently seen evidence of such lesions in the cadaver."
CASE No. 126. Preop. Diag. August 12, 1929. "I have little doubt that this patient has a mild rupture of the supraspinatus, but as the power in abduction is good, operation need not be considered. It is probably not an extensive rent. I suspect both from the clinical signs and from the X-ray that he has had an old lesion here for some years. It seems to me that the best plan of treatment would be to let him rest a few weeks and to have him attend your clinic three times a week for massage. If he does not feel able to go to work again in a month, let me see him again." Sept. 22, 1929. "Examination is as on August 19th. My opinion that he has a small rupture of the supraspinatus is somewhat strengthened by the fact that the symptoms have not improved. As he is only forty-two, I am inclined to advise an exploratory incision under novoeaine to confirm the diagnosis and, if necessary, to suture the tendon. The spot at which he complains of tenderness is so localized that it seems likely we shall find some lesion at this region." Op. Findings. Oct. 23, 1929. "Under local ansesthesia no rupture of the tendon was demonstrated. The walls of the subacromial bursa were thickened and the bursa contained a little fluid. There was nothing found which indicated any recent injury other than the presence of this chronic bursitis. The wound was closed after taking out a small specimen of the synovial lining for pathologic examination." (This showed chronic inflammation.)
CASE NO. 181. Preop. Diag. "In my opinion, he has a chronic subacromial bursitis in consequence of a rupture of the tendon of the supraspinatus." Op. Findings. "A half-inch exploratory incision showed that the roof of the bursa was thickened and adherent to the floor beneath. The wound was enlarged to about one and one-half inches and the adhesions freed, partly by cutting and partly by tearing with the finger. Several small bursal sacs had replaced the usual large one. These sacs lay beneath the adhesions which permitted a certain amount of motion. The adhesions were red and inflamed looking. There were one or two small calcified deposits which were wiped out. The periphery of the bursa outward and backward under the acromion was more normal in appearance and not adherent. The total area involved by the adhesions was about the size and shape of a fifty-cent piece over the greater tuberosity and insertion of the supraspinatus tendon. The most acute tenderness was felt at this point, although there was a little sensitiveness over the bicipital groove. Two or three tags of inflamed serosa were removed for examination and a very small bit of tendon at the point where the adhesions centered was clipped out for examination."
In most of these nine cases, although there was not a complete rupture, there was some evidence of partial rupture beneath the base of the bursa. However, I did not confirm this supposition by cutting through the base, for it seemed to me that its tissue formed a bridge over the gap which would assist in healing the tendon. I am inclined now to think that I have been too conservative, for several of these cases had long convalescences, and it might have been wiser to explore beneath the base of the bursa. At the danger of repetition, I wish to state that I do not intentionally operate, unless I think the ruptures are complete, because I feel confident that where the rupture is complete, healing will not take place unless suture is done. I am not sure enough of what the treatment of partial ruptures should be, to make me urge operation, even if I were sure of the diagnosis. Therefore, the above nine cases may be considered to be errors in diagnosis, although by no means as negative explorations. The difficulty is to tell beforehand whether or not there is actually a complete rupture which needs suture. I think the fact that during a period of sixteen years I made the diagnosis correctly twenty-one times, and incorrectly in only nine cases, shows that the diagnosis is not difficult. When in doubt, such a trivial operation as exploration would be justified, even if the proportion of errors was three to one. In several of the nine cases it is to be noted that the mistake could have been avoided by more reliance on the fact that if there are decided restricting adhesions the diagnosis is not established. In the first case the X-ray indicated the presence of a calcified deposit and should have warned me not to make the mistake, although I should have operated at any rate. In several of the other cases where a mistake was made, the notes indicate that I was in decided doubt about the diagnosis before the operation, and, therefore, the incision as a matter of fact was "exploratory."
END RESULTS IN OPERATED CASES
We next come to the clause "since I have been able to relieve a few cases even though the diagnosis was belated." By referring to pp. 255-260, the reader may see that, excluding cases where there was a coincident fracture of considerable extent, I have operated on thirty-seven cases. In four of these the tendon was retracted to such a degree that I could not even attempt a suture. I have been unable to trace two patients operated upon about twenty years ago. Deducting these six cases we have thirty-one in which an attempt was made to suture the tendon. The results have been as follows: poor, four; fair, seven; good, twenty. That is, two out of every three operations were successful in that the results enabled the patients to return to work, although in most cases only after the elapse of months. A very few, but not many, of my results have been perfect in the sense that the arm was just as useful and just as painless as before the injury; but many of them have been good in the sense that the arms have been relatively painless and quite, if not completely, useful. When I have written "good" I mean that the operation was well worth doing. When I have written "fair" it should convey that, in my opinion, there was some improvement from the operation, but that it was hardly worth doing. "Poor" means that the sum total of relief of the suffering of the patient was not sufficient to compensate for the pain and trouble which were incident to the recovery. There have been no bad results in the sense that any joint was made worse by the operation, but in at least two of the "fair" cases (Cases 83 and 112, see p. 175) the patient's point of view would have been that the result was poor, because his symptoms were not improved in spite of his post-operative pain. There are many factors to account for the lack of perfection in the results, such as the age, the length of time the operation has been delayed, coincident disease, and above all, the desire of the patient to get well. The non-industrial patient is more readily pleased by improvement which lacks perfection than is the employee, who prefers compensation and no work, to double the pay plus work which would undoubtedly cause some pain and discomfort. This compensation factor always causes some delay in the convalescence. Hard times have the same effect. However, my argument does not need to show that all results should be perfect. I could give many excuses for the failures, but will be contented to present the following table.
In three of the four poor results, the tear was very extensive and the repair unsatisfactory; three had weeping wounds from excessive fluid drainage without frank sepsis (see p. 248), and all four had secondary operations. The seven cases of fair results were all improved to a considerable extent but have not actually gone to work again permanently. There was one death which might possibly be attributed to the operation. This patient, Case No. 123, was drowned while in bathing at one of the beaches three weeks after I did an exploratory operation. The operation had shown that the tendons were too badly injured to admit of any attempt at repair. The wound healed by first intention, and as the patient enjoyed going in bathing I permitted him to do so about ten days after the operation. On the twenty-first day he was drowned. He was known to have had a heart lesion. The medical examiner reported "Death by drowning," and did no autopsy. I myself can see no connection between the operation and the drowning, but two doctors offered testimony at the Industrial Accident Board that the patient had had pulmonary embolism from the operative wound. The Board, however, did not accept their testimony, because there was no autopsy or other reason to support their diagnosis. I feel that the proportion of good results is a sufficient reason for advising this operation, even in late cases. With greater experience and improved technique it is likely that the percentage of good results will be increased, but, as in many other surgical conditions, prompt recognition and treatment will be of greater importance than the difference in surgical skill between experienced and inexperienced operators, provided the pathologic condition is thoroughly understood.
END RESULTS IN UNOPERATED CASES
As most of my cases have been "industrial" the question of compensation becomes an important factor in estimating the period of disability. Cases who have no prospect of compensation will unquestionably go to work sooner; for instance, Case 119, a painter who had his own shop, began doing some work within a month after his operation. On the other hand in some cases, the compensation becomes equivalent to an old age pension. I have spent much time and money in tracing the unoperatcd cases of both partial and complete rupture, and have obtained enough information to venture the estimates on page 124 as to the probable costs of each. My estimate of $300,000.00 for 100 cases of complete rupture is also sustained by figures on ten patients on whom I did operate and therefore established the diagnosis. In five of these (delayed) cases the operation was a practical failure, but the patients were no worse off in consequence, and therefore were in a similar status to those in which no operation was done. In the other five the operation was essentially successful.
(The law limits total compensation to $1,000 so that these figures do not cover the period the patient is still disabled after his compensation ceases. The figures also include all medical and surgical charges.)
Case 96 in the first group had a delayed convalescence but eventually was able to go to work again as a steamfitter. Case 127 in the second group was a similar one. The reader may shift either case to the other group if he is disposed to exaggerate either average figure. Although it would not be fair to use the second group at all in computing the cost of 100 unoperated cases, by using it we may obtain an average minimum figure — $2,143.00. Therefore, the figure for 100 cases must be somewherebetween$200,000.00and$4-00,000.00. Pain and disability are difficult to estimate in figures; these estimates are presented to impress on the reader that this lesion is important.
REFERENCES
BTTCHOLZ, C. H., Der Abriss der Supraspinatusshue, Arch. f. klin. Chir., Berlin, 1922, cxxi, 255-264. CODMAN, E. A., Abduction of the Shoulder. An interesting observation in connection with Subacromial Bursitis and Rupture of the Supraspinatus, Boston Med. and Surg. Jour., 1912, clxvi, no. 24, 890-891; Also: Complete Rupture of the Supraspinatus Tendon. Operative Treatment with Report of Two Successful Cases, Boston Med. and Surg. Jour., 1911, clxiv, no. 20, 708-710; On Stiff and Painful Shoulders, As Explained by Subacromial Bursitis and Partial Rupture of the Tendon of the Supraspinatus, Boston Med. and Surg. Jour., 1911, clxv, no. 4, 115-120; The Pathology and Treatment of Lesions in and about the Shoulder Joint. The Industrial Doctor, 1926, iv, No. 8,121-131; Obscure Lesions of the Shoulder; Rupture of the Supraspinatus Tendon, Boston Med. and Surg. Jour., 1927, cxcvi, no. 10, 381-387. FOWLER, E. B., Rupture of Spinati Tendons and Capsule repaired by new operation, Illinois M. J., 1932, lxi, 332-334. KITCHEN, A. S., Surgery of the Supraspinatus Muscle, Journ. Michigan M. Soc, 1920, xix, 64-67. METER, A. W., Absence of the Tendon of the Long Head of the Biceps. Jour. Anat. and Phys., 1913-1914, xlviii; Also: Anatomical Specimens of Unusual Clinical Interest, Am. J. Orthop. Surg., 1915, xiii, 86; Unrecognized Occupational Destruction of the Tendon of the Long Head of the Biceps Brachii, Arch. Surg., 1921, ii, p. 130; Further Observations Upon Use-Destruction in Joints, Jour. Bone and Joint Surg., 1922, iv, p. 491; Evidences of Attrition in the Human Body, Proc. Am. Assn. Anatomists, Anat. Rec, 1923, xxv, 142; Further Evidences of Attrition in the Human Body, Proc, Am. Assn. Anatomists, Anat. Rec, xxvii, 211, 1924; Further Evidences of Attrition in the Human Body, Am. Jour. Anat., 1924, xxxiv, 241; Spontaneous Dislocation of the Tendon of the Long Head of the Biceps Brachii, Arch, of Surg., 1926, xiii, 109; Spon taneous Dislocation and Destruction of Tendon of Long Head of Biceps Brachii j Fifty-nine Instances, Arch, of Surg., 1928, xvii, no. 3, 493-506; The Minuter Anatomy of Attrition Lesions, Jour. Bone and Joint Surg., xiii, 841, 1931. WARNER, F., Injury to Tendons and Joints, Intn. J. Surg., N. Y., 1918, xxxi, 196. WILSON, P. D., Complete Rupture of Supraspinatus Muscle. J. A. M. A., 1931, 483.
So far as I know there is at present no literature on the subject of this chapter which deserves serious study, except that comprised in the above references. I have no doubt that Doctor Meyer and I refer to the same lesions which were studied by Doctor Akerson and can be found by any one who wishes to look for them in similar material. Doctor Meyer's attention has been focused on the long head of the biceps; mine has been focused on the supraspinatus. Probably both of us are in a measure right, and in great measure wrong, but at least we have opened up the field for future students who wish to relieve persons incapacitated by lesions in this region of the body.
NON-OPERATIVE TREATMENT OF RUPTURE OF THE SUPRASPINATUS TENDON
I think every general surgeon who could see one of the complete cases at operation would agree that no form of physiotherapy could influence beneficially one of these lesions, except in a subjective way. The subjective symptoms might possibly be alleviated to a certain degree by massage or by diathermy, but as a matter of fact, nearly all patients say that these agents are of little help. From the very nature of the lesion, manipulations and forced exercises can do no good and might do some harm. If it is determined that a patient is not to have an operation, there are two rational plans of treatment: (1) Fixation in elevation to relax the tendon, improve the blood supply and approximate the torn ends; (2) Gentle "stooping exercises" to help nature smooth off the irregular surface of the lesion. This is merely an aid to nature's own partially successful method. Fixation in elevation, to be effective, would necessarily have to be instituted soon after the injury, and would require at least three weeks. It would be useless in old cases, yet even in the old cases one can see, when the bursa is open on the operating table, that there is a tendency toward approximation of the torn ends of the tendon as the arm is abducted. Of course, in these old cases the proximal end is retracted and cicatrized in its retracted position. Even prolonged fixation in such cases could accomplish little except in possibly diminishing the size of the defect. This tendency to approximation observed at operation in old cases, when the arm is abducted, shows that it is probable that if the rupture were small, this treatment, if immediately instituted, would be worth while. If I were the patient, I would prefer incision and suture to this problematical and uncomfortable, even if reasonable, plan.
The "stooping exercise" method is founded on the pathologic findings described in Chapter III. Clearly nature has developed this method of absorption of the tuberosity to restore function after this accident, for as these patients, after a year or two of misery, improve somewhat, it is fairly clear that this method of smoothing off the eminence and sulcus which caused the jog is the best she can do. Nature's plan is the combination of this slow smoothing-off of the tuberosity and meanwhile increasing the supply of fluid, which, as the lower portion of the capsule becomes tense in any action, is forced up to the site of friction. The idea of the stooping exercises is to begin this process with the weight taken off the arm so that the irregular surface is not forced up under the acromion by muscular tension. If the patient stands and elevates the arm, the very point which is sore becomes the fulcrum on the acromion for the deltoid to exert its power. When the patient stoops with the arm relaxed, the scapula can be abducted on the humerus without the need of the fulcrum either on the glenoid or acromion. Gravity takes the place of the power of the deltoid. It is clear that until a patient can swing his arms freely in the stooping position without pain, he is not ready to use the arm when standing. To patients who refuse operation I explain these mechanics and impress on them what I have said in the last paragraph. I also try to teach them to sleep with the arm abducted, with the hand behind the head. Palliatives in the form of drugs or physiotherapy are not often required in these cases. The pain is always bearable, if they do not increase it with work or exercise which make a fulcrum of the sore point. I think I can accomplish more with these patients by explanation of the mechanics of their trouble than I can with any palliative measures. Show a workman the normal function of the joint, the necessity of the supraspinatus to maintain the fulcrum on the glenoid, the tendency, without it, for the fulcrum to ride on the sore spot where it touches the acromion, the changed action of the weight of the arm when stooping or lying with the hand behind the head, and, as a rule, he will get your drift. He knows about levers and weights. When he understands his condition, he will get rid of the fear element and realize that though his arm is impaired, he has not really lost the use of it. He has learned that he has lost the use of certain motions unless he is willing to stand the pain. This education has more therapeutic value than drugs or electrical treatment. Massage, of course, may do good in stimulating the nutrition of the tissues, but it cannot unite the tendon.
It has seemed to me best to present my operations on the shoulder tabulated in this way, rather than to give complete case histories of each patient. Many of the cases have been used in the text to illustrate different points, sometimes only the occupation being used and perhaps in another place the preoperative diagnosis given to compare with the operative findings, etc. Under the comments at the right of this table the page numbers are given when the individual cases are referred to in the text. Should any one desire to do so, he could, by referring to these pages, make up brief individual case histories. As a rule, the cases which have been spoken of in the text are those in which the result was poor or fair. Those which I have considered good, lack detail. On the whole, compared with the results of the cases in the rest of the table, the outcome in the cases of complete rupture has been relatively poor. The reader is urged to bear in mind that in all the cases on which I have operated my attempts were more or less delayed, for only cases 18, 27, 42, 49,106,115,127, 128, 129 and 135 were done within two months of the accident. In cases 49 and 115 suture was impossible, and cases 27 and 42 could not be traced over a period of years, although the immediate results were good. I probably should not have written this book at all had the results all been good, for one of my chief objects is to urge prompt diagnosis and immediate operation. Some of the cases marked "poor" actually did obtain some improvement. For instance, Case 88 worked over a year after the operation and then had another accident, so that his total compensation was the maximum allowed by law. Case 89 has worked steadily as a watchman after he had made a settlement with the insurer. I feel that I have certainly not exaggerated the benefits of surgery in these delayed cases, for I am sure something was accomplished in all of them, even in cases such as number 115 where no suture was attempted, for at least a definite diagnosis was made, as a basis for a settlement. If, as I hope, eventually the profession comes to realize the importance and frequency of this lesion, and the laboring class becomes educated to take it seriously, exploration through a small incision will be the rule in doubtful cases. When the insurance companies become interested in the problem, I shall be glad to cooperate in making a more extensive survey of the economic side than that which is presented on page 176.
REFERENCE
Wilson and Fowler have modified my operative methods. References to their articles will be found at the end of Chapter V.
OPERATIVE TREATMENT OF RUPTURE OF THE SUPRASPINATUS TENDON
The best time to operate would be immediately after the injury. When in doubt of the diagnosis, exploratory incision of the bursa should be done. The technique of this incision is the same as that which has just been described for use in cases of calcified deposits. Practically the whole base of the bursa can be inspected through this incision and the exact extent of the rupture determined. The incision is then enlarged inward or outward at either end for a half-inch, depending on the direction of the tear. On account of the herringbone structure of the deltoid it makes little difference whether or not the enlargement of the incision is at an angle with the first one. A good exposure can be obtained with an incision one and one- half to two inches in length. Do not enlarge upward farther than the coraco-acromial ligament. Assuming that the operation is done soon after the accident, it would seem that no special directions would be needed. The surgeon knowing the normal relations would restore them by appropriate sutures and close the wound in his favorite manner. It seems to me that this immediate operation would be very easy, but I have not been able to operate on one of these cases in an early stage. In general the operation has two main objects: the repair of the tendon to give power to the arm, and the making of a frictionless lower bursal surface to relieve inflammation and pain. Perhaps the latter is more important, for even a powerful arm, if painful, is not as useful as an arm which is rather weak in the power of abduction but not painful. It is important to keep these two objects in mind, for although in some cases both can be attained, it is sometimes necessary to take a choice between them, because the tissues may be so damaged and retracted that good approximation is impossible. In such a case we may wish to discard all hope of restoring power and devote our whole effort to trying to allay friction. For instance, the tuberosity could be excised wherever it is free from tendinous attachment, and hence is useless. This might diminish the pain by removing the eminence. One must not feel too discouraged, however, about his repair work, for on several occasions I have opened a bursa a second time and found a smooth base and no visible sign of my suture, which, at the end of my previous operation, had appeared rough and clumsy with the ends of the tendons not even approximated but held "a distance." (See p. 245.) Even in a certain number of the delayed cases which I have operated upon, there has been little difficulty in making a satisfactory suture aiming for both objectives, but in other cases, there was little or no hope of making a smooth, even suture which would leave no rough eminence or sulcus. The latter is particularly likely to be the case where the tendon is evulsed from the tuberosity, leaving no stub to hold the stitches. In a few cases the retraction was so great that no suture could be attempted at all.
Special Points and Special Difficulties
I have found that in the old cases on which I have operated, it is seldom easy, often difficult and sometimes impossible to repair the tendon. It seems best to list the difficulties and then to discuss each.
Position on table Mobilizing the tendons The long head of the biceps. Drilling the tuberosity or removing it. Suturing the rent. Formation of a new sulcus. Frictionless surface Material of suture.
Shape of needles.
Closure of bursa. Disposal of fluid. Postoperative treatment.
1. The arrangement of the position of the patient on the table to permit proper mobilization of the arm during the operation, is an important factor in technique. The point of the shouldeT is a difficult region on which to work, for both the surgeon and the assistants. It slinks away and the patient's head and neck seem to wish to take its place. (See Fig. 50.) I should like to stress the importance of so placing a heavy sand bag under the shoulder and another under the corresponding hip that the patient is half turned on his side, while the head, with the face turned away, is at a lower level than the point of the shoulder. The shoulder should be slightly over the edge of the table toward the operator, so that the arm may be allowed to hang down in a position of dorsal flexion when desired. This position throws the distal portion of the supraspinatus tendon forward for the maximum distance from under the acromion.
The operator and assistant stand on the same side of the table, while the anaesthetist and nurse with the instrument table are on the other side. A second assistant is welcome, and often almost necessary, because the first assistant must at times give his entire attention to holding the arm and the nurse may be occupied with retractors. Much of the facility with which the operation is conducted depends on the assistant who holds the arm, for his ability to rotate just at the right time will enable the operator to put his needle at just the right point in the somewhat small field. Since the lips of the incision do not move appreciably, the operative field is really controlled by the assistant as he rotates the humerus, bringing this side of the rent or that into a position which the operator desires. The maneuver already described, of letting air into the joint and bursa, is often a great help. The position in which to place the sutures is best illustrated by a diagram. (Fig. 52.) While this is the ideal, it is seldom possible to carry it out exactly, for too often the retracted, stiffened tissues cannot be worked into nice apposition.
FIGURE 52. METHODS OF PLACING SUTURES a illustrates the writer's suggestion that the biceps tendon may be sutured to the supraspinatus in some cases when the former has been already torn from the edge of the glenoid, b, c, and d suggest the method of placing the sutures in the ruptured supraspinatus and in the tuberosity. The ideal is c, for in this case the lines of incision have been carried up on each side of the supraspinatus to mobilize it. d illustrates Dr. Wilson's method of cutting a slot to receive the supraspinatus tendon, e and / offer a suggestion for operation in a case where the short rotators have been entirely evulsed from the head of the humerus. Fascia lata might be passed through a drill hole and through a slot over the tuberosity to form an anchorage for the tendons.
2. Mobilizing the tendons. When one considers that each one of the short rotators is separated from the other by a definite bony partition through most of its extent, and it is only the last three-quarter inch which is welded with the others into the terminal conjoined tendon or cuff (Fig. 10), it would seem easy to isolate any one tendon so that the more or less elastic muscle belly could be stretched enough to bring the tendon down again to the tuberosity and suture it there. However, if you try this on a normal shoulder at autopsy, you will find it is not easy, and when you try it on a ruptured tendon in which operation has been delayed for many months, you will find it impossible. In the first place, you are cramped for room by the acromion and coraco-acromial ligament so that you cannot see the muscle bellies even in the normal shoulder. In the second place, if you dissect back more than an inch on either the supraspinatus or infraspinatus, you run the risk of wounding the suprascapular nerve, and if you do, you may lose your power in those muscles forever. In order to get at these tendons more effectively, I used to use the "sabre-cut incision," which gave a perfect exposure and every possible opportunity. (Plate VIII.) Even then the mobilization was only a little more satisfactory, so I have given up this incision. Practice has given me a little more confidence, and I believe now I can do almost as well through the simple routine incision. Dr. William Rogers has suggested removing the deltoid attachment with the periosteum from the acromion and suturing them back at the end of the operation." This seems rational, but I have not tried it and do not know whether one may rely on having the deltoid origin anchor again satisfactorily. I have sometimes thought that a subcutaneous osteotomy of the base of the acromion might mobilize it enough even without division of the coraco-acromial and acromioclavicular ligaments to allow easy access. The trouble with any incision which mobilizes the acromion is the long period which one must wait for union to occur before moving the joint. I am inclined at present to do all the mobilizing I can through the routine incision, and I find that I am constantly improving in my ability to do this. It is probably best to remove the falciform edge of new tissue and to refresh the edges of the tendon itself. I attribute some of my imperfect results to my failure to do this. One learns by experience to put the suture back of the falciform edge, for the latter has no strength and the stitch at once tears out. One is tempted not to remove the edge because it is obviously difficult to close the rent without using it, and it seems folly not to save all the tissue one can. It might be contended that the falciform edge may have more tendency to unite than the real tendon substance, which has very little blood supply, so that perhaps I may be wrong in recommending the removal of this new tissue with which nature is attempting to repair the damage. The method of closure which seems to me the best is illustrated in Fig. 52.
3. The long head of the biceps. The problems connected with how to deal with the long head of the biceps when it is found exposed, owing to the retraction of the ruptured tendons, are not a few. I can only discuss them and do not pretend to solve them. Although I am not in agreement with some of Meyers' views on the importance of the role of the biceps tendon in shoulder injuries, I feel that his observations ought to be known to every one who operates on these cases. To my mind, the rupture of the supraspinatus is the primary and important lesion which uncovers the biceps tendon, makes it slip a little at the top of the bicipital groove and to tend to be caught between the tuberosity and the acromion. At any rate, one often finds it a conspicuous, pink, inflamed-looking, swollen band lying across the j oint cartilage at the bottom of the rent. ( Plate VIII.) The portions exposed in the rent look inflamed; those covered by the remaining intact part of the capsule are white, glistening and normal. It is pretty obvious that our suture should cover up the biceps tendon without interfering with it otherwise. It usually lies just under the inner edge of the rent, but if any of the subscapularis fibers are involved, it lies entirely exposed. Sometimes it is not found at all, for it has been torn away from its glenoid attachment and has retracted down the bicipital groove. Sometimes it is split in two, longitudinally. Often it is flattened and frayed at the edges. Varying proportions of it may be ruptured. It may be composed of indefinitely separated longitudinal strands, some of which have become welded into the capsule. It may have little, rice-like tags on its edge. However, almost always the parts which do not become exposed in the gap left by the supraspinatus are normal in appearance. When it has ruptured from the glenoid, it may be held high in the groove by a few remaining bands, and we can capture it and pull it up. What shall we do with it? We might try to suture it back on the glenoid, or rather on the fibrocartilage which surrounds the glenoid. Or we might attach it to the proximal portion of the supraspinatus, or to the capsule, or anchor it in the groove, or excise a part of it and use it to repair the supraspinatus. We might even take a relatively normal biceps tendon, clip its attachment off the glenoid, anchor the tendon in the groove, and then use the redundant portion to fill the gap in the supraspinatus. (Fig. 52a.) This would give the biceps muscle a fixed origin, and we would at the same time obtain a firm attachment for our supraspinatus. We should only have lost whatever function the long head of the biceps has from having its attachment on the glenoid rather than on the humeral head; i.e., the outer head of the biceps would no longer be of use in motions of the humerus on the scapula, but could still apply its power in flexing the forearm on the humerus. What then is this function which we should lose so far as scapulo-humeral motion is concerned? The function of the biceps muscle is fourfold. First, it is a flexor of the forearm on the humerus. Second, it is one of the flexors (or extensors?) of the whole arm on the scapula; in a sense, therefore, it is a weak abductor or elevator of the arm. Third, the external insertion on the tubercle of the radius enables it to act as a supinator of the radius and hand. Fourth, the long head of the biceps passing through the intertubercular groove helps to retain the head of the bone on the glenoid, and stabilizes the head in the various degrees of rotation, as the arm is elevated. This function is well illustrated by the findings in two of my cases, which at operation showed that except for the subscapularis, the whole of the capsule with the tendons of the supraspinatus, infraspinatus and teres minor had been evulsed, yet the head did not tend to dislocate; apparently it was held in the joint'by the long head of the biceps, and by that only. We lose nothing in the first function, little in the second, none in the third and but a problematic amount in the fourth, by using it in the way suggested in Fig. 52a. So far as the action of the shoulder joint is concerned, particularly with reference to the functions of flexion of the arm on the scapula and of the forearm on the humerus, the origin of the short head of the biceps from the coracoid process is more important than that of the long head from the edge of the glenoid. The coracoid origin is sufficient to give power in these motions; the long head is chiefly a stabilizer and one of secondary use so far as the application of power is concerned. For instance, in cases in which the long head of the biceps is ruptured and no other lesion has occurred, the function of the shoulder remains almost normal. The short rotators are sufficient to maintain the fulcrum on the glenoid in most positions of the arm, but where these short rotators are damaged, I am confident that the long head serves a very useful purpose in guiding the head of the humerus and restraining it from forging upward and getting its fulcrum on the acromion. I therefore regard it as important to keep the long head of the biceps intact if possible. I have notes that in some of my operated cases, the biceps was torn away from its glenoid attachment. In such cases in future I intend to search for the distal end of the tendon and to anchor it with stitches in the bicipital groove, and also to the supraspinatus tendon, thus abandoning any idea of retaining its stabilizing function and being content with retaining its power as a flexor of the forearm. At present I see no good mechanical way of re-attaching it to the glenoid so as to make it function in guiding the head of the humerus as the latter is abducted. One is apt to think of the long head of the biceps moving up and down in the intertubercular groove, but this is not what actually happens. The humerus moves up and down on the tendon; it is not the tendon which moves through the groove. (See Fig. 52.) On the whole, I should say that if the operator finds that the biceps is so damaged that he thinks it will not in future form a smooth cord on which the humerus can ride up and down, he had better use it, as described above, to replace the lost substance in the supraspinatus.
4. What shall we do if we find there is no stub of supraspinatus tendon left on the tuberosity to which we may suture the proximal portion? In long-standing cases we find a tuberosity completely bare of tendinous substance, and perhaps somewhat eroded. Since this tuberosity is useless unless we can suture the tendon to it, it might as well be removed. I have not hitherto excised the tuberosity in cases in which I could not suture, but it might be well to do so. Such an excision would make the surface which must ride under the acromion less apt to cause friction. Nature does exactly this by causing recession of the tuberosity. As a rule I have drilled two holes in the tuberosity with an ordinary shoemaker's awl, and passed a heavy silk suture through these holes and the tendon so as to draw the tendon as nearly as possible to the facet of insertion of the supraspinatus. This can usually be accomplished, but occasionally the supraspinatus is so retracted that I cannot quite draw it down to the bone. I have on several occasions made a sort of plastic so that I covered the suture with part of the roof of the bursa, believing that the repair of the tendon comes not from the tendon itself, but from the adj acent synovial membrane which is much richer in vascular supply.
5. Another operative problem is how to repair the rent. As explained in the chapter on pathology, these rents are in a general way triangular, with the base on the humerus and the apex retracted, the apex being usually the center of the supraspinatus, and the sides the lateral expansions which are united to the neighboring tendons. The ideal way to close would be to bring the center of the apex to the center of the base, but if the retraction is great and the base is small, the triangle is so prolonged upwards that one is tempted to close the gap from side to side until very near the base, and then to make the last suture a triangular stitch. This method is easier, but it does not bring back the normal relations. However, it is a feasible method to use where there is much retraction. The exact way in which to put the sutures does not seem important, that is, whether they are mattress sutures or interrupted or continuous.
6. Formation of a new sulcus. If the reader will refer to Chapter IV, and especially to Plate VI, Figs. 3-4, and their legends concerning the remarkably effective method which nature has devised to attach the supraspinatus tendon to its facet, he will feel great doubt as to whether the surgeon will ever be able to imitate it with any degree of success. We need much study and experimental work before we can rely on being able to create a line of living cement such as the "blue line," with its pores for the finger-like processes. At present, from what we know of histology, it seems doubtful whether in adult life such a method of union of tendon to bone can ever be achieved. However, we know that tendon can form a fairly firm cicatricial attachment to raw bone. What is the best practical way to secure this ?
If it were possible, we should wish to have the new tendon form on the raw surfaces of the sulcus and of the tuberosity down to the actual edge of the joint cartilage. When I drill the tuberosity I try to drill it as far as the cartilage edge, and I usually erode the bone of the sulcus with the point of a knife or curette, so that the tendon will have a little better chance to become attached by granulation. Dr. Philip Wilson has improved on my operation by cutting a slot around the cartilage edge and drilling through the base of the tuberosity. He then passes a slip of fascia lata through the drill holes to be attached above to the supraspinatus. He thus makes a more ideal suture, so that the tendon fills the entire sulcus and thus gains a firm hold on the tuberosity. It remains to be seen whether nature will tolerate such attachments indefinitely.
7. A frictionless surface for the base of the bursa is a most important point. Dr. Wilson's method has this advantage. It would be repetition to discuss this further, but I should like to repeat that even in those cases where the suture at the end of the operation has seemed rough, it may nevertheless be so changed by the healing process that a surface is produced which at a later operation appears smooth and normal.
8. I use silk sutures because I want them to endure long enough for new, strong, scar tissue or tendinous substance to form over them. I use a fairly heavy pedicle silk for the main suture, which passes through the holes in the tuberosity or between the proximal and distal portions of the tendon. I have on four occasions reopened the bursa later to remove these silk stitches because the patient complained of pain. The following are the findings in these four cases:
CASE 18 Mr. R. H. S. Age 60. M. G. H. No. 181765 E. S., Mar. 26, 1912. A typical case of complete rupture of the supraspinatus, one and one-quarter inches wide. Although much retracted, the tendon was caught and sutured in place with three mattress sutures. The functional result was good, but he continued to have more or less pain, apparently from the formation of a considerable amount of dense inflammatory tissue about the site of suture. On Feb. 13,1913, under novocaine, the bursa was again opened and the tendon was found not only completely repaired, but there was a large amount of dense hypertrophic, callous-like tissue about the sutures. This mass impinged on the acromion in abduction; most of it was removed with the scissors and a new opening made through the supraspinatus into the joint, so that some of the synovial fluid could flow into the bursa and lubricate it. The result of this operation has been satisfactory. Twelve years later, on June 9, 1925, he called to see me because of a slight injury to his left shoulder. The right, on which I had operated, had given him no trouble in the intervening years, although he had worked steadily as a coachman.
CASE 29 Mr. M. M. W. Age 39. M. G. H. No. 184216 W. S., Aug. 5, 1912. A clear case of badly ruptured supraspinatus tendon. The tendon was sutured with heavy silk and function was restored. During the following year he had much pain on use of the arm in his work as a laborer. The bursa was again explored and the silk sutures and some of the chronic inflammatory tissues lying about them were removed. I also made a new opening into the true joint to permit the fluid to flow into the bursa. This was followed by improvement but not by complete relief. No late report. Note that entire repair of the rupture had taken place.
CASE 88 Mr. T. M. Age 50+. Operated on at Faulkner Hospital, July 24, 1926, six months after his injury. The supraspinatus, infraspinatus and part of the subscapularis were found to be torn away, exposing the biceps tendon, which was greatly inflamed. There was much fluid in the joint. A very unsatisfactory suture was made, and the tuberosity had to be drilled. The arm was put up in abduction. Mild sepsis occurred and there was much fluid drainage, so that the wound took several weeks to heal. Some of the deep sutures were taken out. In spite of this the result at first was good, and he returned to his work after five months. He worked for a year and three months, although in some pain, and then had another slight injury. On July 2, 1928,1 again explored the bursa and found that most of the sutures had pulled away, leaving the condition practically as bad as at the first operation. This was as bad a result as I have ever had. The patient was for a time benefited, but in the end gained nothing by the operation, for I did not attempt a second suture.
CASE 112 Mr. A. C. Age 62. Operated on at the Trumbull Hospital on June 11, 1928, three months after his injury. A typical complete rupture of the supraspinatus was found and satisfactorily sutured. The immediate result appeared to be good. However, the patient would not go to work again, complained bitterly of pain on use of the arm and became very neurasthenic. On Feb. 7, 1929, I again explored the bursa, thinking that if I took out the deep sutures some of the irritation might be relieved. My notes say: "I operated on him yesterday under novocaine ansesthesia. Dr. B. E. Wood was present and Dr. Stevenson assisted. Incision was made just inside the old scar and the bursa was opened. It was clearly shown that the former suture had been effective in restoring the insertion of the tendon. Moreover, the floor of the bursa was smooth and shiny, and there did not appear to be any cause for friction over the site of the suture. One heavy silk suture could be seen just below the transparent synovial lining of the base of the bursa; this was easily pulled out, but the other two sutures were buried deeply in the new-formed tendon and were found and removed with difficulty, as I was anxious not to weaken the tendon in so doing. In two of the sutures the knots were apparently untied; in one the knot was still present, but almost untied. At first I thought that the knots of the two untied ones had been left behind, but on reflection I think it is more reasonable to suppose that they had become untied as the tissues increased in amount and grew into the knots, which were cut very short. Yet it is possible that they broke off and remained in, although the total amount of silk in the untied ones appears greater than in the tied one by more than double. At any rate, very little silk could have been left behind. "I did not feel satisfied that the silk was causing any trouble, for there appeared to be no inflammation about it, and the tender point of which the patient complained was nearly a half-inch away from the sutures, on the edge of the greater tuberosity close to the bicipital groove. That there was some inflammation at this point was made clear by finding a little crumbly, soft, cheesy tissue close to the synovial sheath of the biceps tendon, which in certain positions bulged slightly. The repair of the tendon was weakest at this point, and I fear that my search for the sutures weakened it still more, although not to an extent sufficient to interfere with function, and recompensed by the finding of this suspicious tissue. Two tiny bits of this tissue were saved for pathologic examination. (Plate V, Fig. 5.) The patient still claimed to be unable to work in January, 1931. Since three out of four cases, which were explored a year or so after the first operation, showed not only firm tendons but hyper-trophied ones, it seems to me that it is proved that suture may be effective. In each case I was surprised to see how well nature had restored the even convexity of the floors of the bursae, which at the completions of the operations had been quite irregular and rough at the suture lines. All four cases, if operated on immediately after their injuries, might have had excellent results; as it was, although two of the four cases had good results, little was gained by the other two patients, unless they may take some satisfaction as demonstrators of the fact that these tendons even when badly broken may be repaired.
9. The shape of the needles is dictated by the shape of the field of operation and by the fact that a tremendous strain is put on them. They must be either fully curved or half curved, not over a half-inch long and with very strong shank and eye. One has to work between the acromion and the tuberosity, where there is very little room, so that even a curved needle such as is used in ordinary operations is too large to be turned about in this space.
10. Shall we close the roof of the bursa or shall we merely close the muscle, leaving the roof of the bursa free to allow the synovial secretions to seep into the areolar tissue? As I have previously stated, there is usually in these cases a considerable synovitis with a large amount of fluid. If the bursa is closed tight, this fluid forms under tension and causes pain. Closure also tends to keep blood in the bursa which would otherwise be washed out by the fluid itself. I prefer the idea of leaving the roof of the bursa unsutured to allow this fluid to escape, but I am not prepared to say positively that it is not better to suture the bursa and allow free motion after the operation to pump fluid out between the stitches. The fact is, in cases where there is much fluid (and these cases are usually those that have continued to work in spite of the friction and pain), the fluid seeps into the soft tissues to an extent which causes marked swelling and sometimes induces an edema and suggestion of sepsis. This used to be a frequent complication when I put the arm in elevation, permitting the lower side of the capsule to be held tense and therefore driving the fluid up toward the wound. Now that I treat them without restraint, I do not have this complication
11. The postoperative treatment. I find that my tendency has been, as the years go by, to allow more motion and to allow it sooner. I usually pad the axilla with a small pillow and then let the arm lie on it in a position a little more abducted than that in which the arm rests in a sling, contriving as best I can to keep the hand away from the front of the abdomen, because the tendency of the patient after these operations is to get the arm in a strongly internally rotated position, and therefore the recovery of the power of external rotation is slow. After the first night is over, I remove the dressing and let the patient put the arm in any comfortable position which he can find. Each day I exercise it in a way which is difficult to describe, but which is a matter of personal touch. The general purpose of the exercises is to let the patient bend his body from the hips with the arm relaxed, as described under the stooping exercises (Fig. 47). As in treating fractures near joints, I try to make the patient do as much active and passive motion of the arm as I believe I can without displacing the fragments. It is impossible to lay down more definite directions, but I may say that by the end of the first week I expect the patient to be able to bend his body at the hips to a right angle, and to let both the injured and well arm fall in a relaxed position at right angles to his body. By twisting his body from side to side so as to make one shoulder higher than the other, alternately, he can also move the joint without contracting the shoulder muscles. During the second week he is encouraged to swing the arms a little in both directions in this stooping position. The wound should be soundly and completely healed and the patient discharged from the hospital in from ten days to two weeks. After that he is encouraged to take the stooping exercises. If the patient is cooperative and understands the mechanics of the operation and can use common sense in taking his exercises, he gets on fairly smoothly, but there is pain of an annoying although not of a serious degree, not only for weeks but for months. I do not think this would be the case where the operation was done immediately after the accident. In convalescence it is a good rule to restrain the patient from exercising his arm in the erect position until he has learned to abduct it freely and strongly in the stooping position. (See Fig. 47.) In long-standing cases the nerves of the region have already become sensitized and are slow in returning to a normal condition. Much of this postoperative soreness in the delayed cases is due to the sensitiveness and synovitis acquired between the date of the injury and that of the operation.
THE SABRE-CUT INCISION
Reprinted from the Bos. Med. & Surg. Jour., Mar. 10, 1927. It does not differ greatly from Kocher's posterior incision, but is more appropriate after a preliminary exploratory cut anterior to the joint.
FIGURE 1
"Sabre-cut" seemed an appropriate name for this incision, for it might well be made by the downward cut of a sabre on top of the shoulder. An incision is made through the acromio-clavicular joint and continued with a saw through the base of the acromion. The anterior point of the incision would be continuous with a previous routine bursal exploratory incision. When the acromion has been sawed through, an epulet of tissue, consisting of the deltoid muscle and the acromion process from which it arises, is formed to be pulled outward and downward. This step is accomplished' with ease, for it is only held by a little areolar tissue and a few fibers of the trapezius attached to the upper margin of the detached portion of the acromion. The upper posterior fibers of the deltoid must be separated a little to gain mobility. In sawing the base of the acromion one must bear in mind the suprascapular nerve which supplies the supra- and infra-spinatus muscles and lies between them, a little below the saw-cut. It is deep enough to be out of the way of the saw but not of gross carelessness.
FIGURE 2
The second diagram shows the structures exposed when this epulet is pulled downward and outward. Even without dissection one can identify the subscapularis, supraspinatus and infraspinatus as they emerge to join together their tendinous expansions beneath the base of the bursa. To one unfamiliar with this dissection the smooth convex surface of this base appears to be the articular surface of the humerus. The subacromial and subcoracoid or coraco-humeral bursse are nicely shown. As explained in previous papers, they are often intercommunicating and are always functionally one bursa although frequently, as in this instance, separated by one of the diaphanous nictitating folds. Notice the separated portion of the acromion and see how easily it will fit back into place.
FIGURE 3
The third diagram is identical with the last except that the supraspinatus and capsule have been cut across into the true joint and the ends of the supraspinatus depicted as retracted. The stub of the tendon is still attached to the tuberosity beneath the base of the bursa, while the muscular belly is retracting into the supraspinatus fossa. The glenoid and the articular surface of the humerus are exposed, with the long head of the biceps arising from the superior edge of the glenoid lying across the cartilaginous surface of the head of the humerus. This is exactly the condition I have found at operation again and again in the living, except that there is seldom so much of a stub of tendon still attached to the tuberosity. Quite frequently it is entirely evulsed from the latter, requiring drilling of the tuberosity to resuture it. I have always found the base of the bursa to be torn across with the tendon. The point of least resistance appears to be about the subbursal portion of the tendon. In fact the tendon itself is very short, the muscle fibers beginning within a half-inch of the attachment. In the long-standing cases on which I have operated the biceps tendon is found inflamed, swollen and bright pink in color, forming a striking contrast with the white articular surface of the humerus. Sometimes it is apparently absent entirely, having been evulsed and then retracted downward into its sheath. To close this incision the parts are sutured back into place in the reverse order of these diagrams. It is probably safer to wire the acromion process, although catgut in the soft parts holds it well. I do not advise attempting to close the bursa even in the exploratory operation; a stitch or two in the muscle holds the edges in sufficient apposition and excess fluid may drain into the areolar tissue.
The pendulum will probably swing in future toward postoperative treatment in abduction and back again to adduction. Dr. Wilson now uses abduction after the sabre-cut incision and complete repair of the insertion into the bone by the use of fascia lata. It is possible that this method has the advantage of creating a larger gap between the head of the humerus and the acromion and the coraco-acromial ligament, because reunion of the mobilized acromion process would take place at a higher level, since it is pressed upward by the abducted humerus.
The Sabre-Cut Incision. Although I have personally given up the sabre-cut incision for cases of rupture of the supraspinatus, it is still used by others, especially by Dr. Wilson. It gives a splendid opportunity to repair the tendon or any other structure in the shoulder joint, but it is really a major operation, while the one I use is a minor one. The main reasons why I seldom use it are three. In the first place, I have learned to work through the routine incision in such a way that I can do the operation without cutting any ligaments or bone. This improvement has come about not only from doing the operation in dorsal flexion, but by using the method of rotating the humerus so that each desired point is placed in the middle of the small incision at the appropriate moment for a stitch. One assistant has to manipulate the arm in unison with the wishes of the surgeon. In the second place, I have found that after division and suture the acromio-clavicular joint may remain somewhat unstable. A third reason is less technical and more in the domain of human nature. In Industrial Surgery there is not a frank understanding between surgeon and patient as in their ordinary professional relation. The patient is apt to have the element of compensation too strongly in mind, as compared to a cooperative tendency to make the best of the surgeon's attempt to better an injured limb, although both know it may never again be "as good as new." The extent of the sabre-cut incision exaggerates in the patient's mind the degree of the injury and the scar would certainly be impressive to a commission or jury.
Frontispiece
RUPTURE OF THE SUPRASPINATUS TENDON
FRONTISPIECE
THANKS to Dr. F. B. Mallory I was able to obtain the autopsy specimen of a case of a completely ruptured supraspinatus, from which this painting was made by Mr. Aitkin. The skin and subcutaneous tissues were removed; then the fibers of the deltoid separated and held apart by retractors as in the usual routine incision. The diamond-shaped area between the two retractors is the floor of a rather large bursa. Nearly the whole right half of this floor retains its normal, smooth, whitish appearance, but in the left-hand portion of the base or floor is a roughly triangular area which represents the gap formed by the retracted supraspinatus tendon. At the right of this triangular gap, the long head of the biceps appears just beneath the falciform edge of the portion of the musculo-tendi-nous cuff formed by the subscapularis. In the left angle of the triangular area is seen a falciform edge formed by some of the superficial fibers of the infraspinatus. Just superior to this are a few vertical fibers of the deep posterior part of the supraspinatus which have not been evulsed. This was a. very thin, tenuous bit of tissue. The remaining central portion is roughly divided into three parts. The upper, bluish third is the exposed cartilage of the true joint. On its shiny surface near the very edge of the true joint cartilage, we see the high light of the reflection of the window. The lower third of this central space shows a typical "volcano" on the tip of the tuberosity, such as those depicted in Plate V, Figure 1, and in Figures 36 and 40. Between this "volcano" and the cartilage, and also occupying about one-third of the central area and bounded on the right by the margin of the biceps tendon, and on the left by the film-like, untorn edges of the infraspinatus and supraspinatus, we see a red, granulation-like irregular surface. This is the pathologically changed facet of insertion of the supraspinatus tendon and of a portion of that of the infraspinatus from which the tendons have been torn. Compare Figure 40, which is the Rontgen picture of the same specimen. It must be understood that this picture represents the result of an injury experienced, in all probability, many years before; the tuberosity is in the recessing stage, and the edges of the torn tendons have become smooth by becoming falciform. The distal stub of the supraspinatus tendon, which was probably present in the first few months after the injury, being functionless, has disappeared. The proximal end of the tendon has retracted upward and could only be demonstrated if the newly formed falciform edge of the whole rent were removed. Even in this old case it could be isolated, pulled down and attached to the tuberosity, although with difficulty. One can readily imagine the pain which this patient endured during the first few years after his injury from the mere mechanical irritation from the tuberosity striking on the edge of the acromion during efforts at elevation of the arm, although nature has gradually nearly smoothed off the former prominent tuberosity, and, by partial healing of the edges of the torn structures, has made a new base of approximately spherical surface to pass under the acromion. The writer's operative efforts have mostly been concerned with relieving the results of such conditions. When the general practitioner has learned to recognize the symptoms of these lesions within a few days of their occurrence, suture of such torn tendons will be easily and successfully accomplished.
References
- ↑ Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy 1994;10:363-70.
- ↑ Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202.
- ↑ Denard PJ, Lädermann A, Brady PC, et al. Pseudoparalysis From a Massive Rotator Cuff Tear Is Reliably Reversed With an Arthroscopic Rotator Cuff Repair in Patients Without Preoperative Glenohumeral Arthritis. Am J Sports Med 2015;43:2373-8.
- ↑ Inman VT, Saunders M, Abbott, MC. Observations on the function of the shoulder joint. J Bone Joint Surg Br. 1944;1(26):1-30
- ↑ Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med 1982;10:336-9.
- ↑ Chalmers PN, Cvetanovich GL, Kupfer N, et al. The champagne toast position isolates the supraspinatus better than the Jobe test: an electromyographic study of shoulder physical examination tests. J Shoulder Elbow Surg 2016;25:322-9.
- ↑ Gerber C, Blumenthal S, Curt A, Werner CM. Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J Shoulder Elbow Surg 2007;16:815-20.
- ↑ Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg 1996;5:307-13.
- ↑ Collin P, Treseder T, Denard PJ, Neyton L, Walch G, Lädermann A. What is the Best Clinical Test for Assessment of the Teres Minor in Massive Rotator Cuff Tears? Clin Orthop Relat Res 2015;473:2959-66.
- ↑ Patte D, Goutallier D. [Grande libération antérieure dans l'épaule douloureuse par conflit antérieur]. Rev Chir Orthop Reparatrice Appar Mot 1988;74:306-11.
- ↑ Walch G, Boulahia A, Calderone S, Robinson AH. The 'dropping' and 'hornblower's' signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br 1998;80:624-8.
- ↑ Collin P, Treseder T, Denard PJ, Neyton L, Walch G, Lädermann A. What is the Best Clinical Test for Assessment of the Teres Minor in Massive Rotator Cuff Tears? Clin Orthop Relat Res. 2015 Sep;473(9):2959-66
- ↑ Neer C. Cuff tears, biceps lesions, and impingement. In: Neer C, ed. Shoulder reconstruction. Philadelphia: W. B. Saunders Company; 1990:41-142.
- ↑ Walch G, Boulahia A, Calderone S, Robinson AH. The 'dropping' and 'hornblower's' signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br 1998;80:624-8.
- ↑ Nove-Josserand L, Edwards TB, O'Connor DP, Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res 2005:90-6.
- ↑ Werner CM, Conrad SJ, Meyer DC, Keller A, Hodler J, Gerber C. Intermethod agreement and interobserver correlation of radiologic acromiohumeral distance measurements. J Shoulder Elbow Surg 2008;17:237-40.
- ↑ Sheean AJ, Hartzler RU, Denard PJ, et al. Preoperative Radiographic Risk Factors for Incomplete Arthroscopic Supraspinatus Tendon Repair in Massive Rotator Cuff Tears. Arthroscopy. 2018 Apr;34(4):1121-1127.
- ↑ Hamid N, Omid R, Yamaguchi K, Steger-May K, Stobbs G, Keener JD. Relationship of radiographic acromial characteristics and rotator cuff disease: a prospective investigation of clinical, radiographic, and sonographic findings. J Shoulder Elbow Surg 2012;21:1289-98.
- ↑ Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases). Am J Roentgenol Radium Ther Nucl Med 1971;112:493-506.
- ↑ Plomb-Holmes C, Clavert P, Kolo F, Tay E, Ladermann A, French Society of A. An orthopaedic surgeon's guide to ultrasound imaging of the healthy, pathological and postoperative shoulder.Orthop Traumatol Surg Res. 2018 Dec;104(8S):S219-S232.
- ↑ Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007;35:719-28.
- ↑ Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994:78-83.
- ↑ Sheean AJ, Hartzler RU, Denard PJ, et al. Preoperative Radiographic Risk Factors for Incomplete Arthroscopic Supraspinatus Tendon Repair in Massive Rotator Cuff Tears. Arthroscopy. 2018 Apr;34(4):1121-1127.
- ↑ Meyer DC, Farshad M, Amacker NA, Gerber C, Wieser K. Quantitative analysis of muscle and tendon retraction in chronic rotator cuff tears. Am J Sports Med 2012;40:606-10.
- ↑ Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Investigative radiology 1998;33:163-70.
- ↑ Williams MD, Lädermann A, Melis B, Barthelemy R, Walch G. Fatty infiltration of the supraspinatus: a reliability study. J Shoulder Elbow Surg 2009;18:581-7.
- ↑ Kissenberth MJ, Rulewicz GJ, Hamilton SC, Bruch HE, Hawkins RJ. A positive tangent sign predicts the repairability of rotator cuff tears. J Shoulder Elbow Surg 2014;23:1023-7.
- ↑ Sheean AJ, Hartzler RU, Denard PJ, et al. Preoperative Radiographic Risk Factors for Incomplete Arthroscopic Supraspinatus Tendon Repair in Massive Rotator Cuff Tears. Arthroscopy. 2018 Apr;34(4):1121-1127.
- ↑ Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 1996;67:264-8.
- ↑ Niglis L, Dosch JC. Intra- and inter-observer agreement in MRI assessment of rotator cuff healing using the Sugaya, Goutallier, Warner and Thomazeau classifications 10 years after surgery. “s.l.” and “s.n.”: Université de Strasbourg; 2015.
- ↑ Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand 2001;72:365-71.
- ↑ Neer CS, 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89.
- ↑ Bono CM, Renard R, Levine RG, Levy AS. Effect of displacement of fractures of the greater tuberosity on the mechanics of the shoulder. J Bone Joint Surg Br 2001;83:1056-62.
- ↑ Greiner S, Scheibel M. [Bony avulsions of the rotator cuff : Arthroscopic concepts]. Der Orthopade 2011;40:21-4, 6-30.
- ↑ Burkhart SS, Klein JR. Arthroscopic repair of rotator cuff tears associated with large bone cysts of the proximal humerus: compaction bone grafting technique. Arthroscopy 2005;21:1149.
- ↑ Lädermann A, Denard PJ, Burkhart SS. Arthroscopic management of proximal humerus malunion with tuberoplasty and rotator cuff retensioning. Arthroscopy 2012;28:1220-9.
- ↑ Burkhart SS, Klein JR. Arthroscopic repair of rotator cuff tears associated with large bone cysts of the proximal humerus: compaction bone grafting technique. Arthroscopy 2005;21:1149. Complete reabsorption of the tuberosities have also been observed (Figure).
- ↑ Moore DR, Cain EL, Schwartz ML, Clancy WG, Jr. Allograft reconstruction for massive, irreparable rotator cuff tears. Am J Sports Med 2006;34:392-6.
- ↑ Roche CP, Diep P, Hamilton M, et al. Impact of inferior glenoid tilt, humeral retroversion, bone grafting, and design parameters on muscle length and deltoid wrapping in reverse shoulder arthroplasty. Bulletin of the Hospital for Joint Disease 2013;71:284-93.
- ↑ Ek ET, Neukom L, Catanzaro S, Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg 2013;22:1199-208.
- ↑ Sershon RA, Van Thiel GS, Lin EC, et al. Clinical outcomes of reverse total shoulder arthroplasty in patients aged younger than 60 years. J Shoulder Elbow Surg 2014;23:395-400.
- ↑ Lädermann A, Denard P, Abrassart S, Schwitzguébel A. Achilles Tendon Allograft for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity: A Case Report. Knee Surg Sports Traumatol Arthrosc 2016;Jan 25.
- ↑ Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg Am 1985;67:974-9.
- ↑ Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 2010;26:417-24.
- ↑ Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2000;82:505-15.
- ↑ Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA, 3rd. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 1991;73:982-9.
- ↑ Lädermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. International orthopaedics 2015;39:2403-14.
- ↑ Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202.
- ↑ Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res 1990:81-6.
- ↑ Meyer DC, Farshad M, Amacker NA, Gerber C, Wieser K. Quantitative analysis of muscle and tendon retraction in chronic rotator cuff tears. Am J Sports Med 2012;40:606-10.
- ↑ Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 2010;26:417-24.
- ↑ Hohmann E, König A, Kat CJ, Glatt V, Tetsworth K, Keough N.Single- versus double-row repair for full-thickness rotator cuff tears using suture anchors. A systematic review and meta-analysis of basic biomechanical studies. Eur J Orthop Surg Traumatol. 2018 Jul;28(5):859-868.
- ↑ Sobhy MH, Khater AH, Hassan MR, El Shazly O. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol. 2018 May;28(4):593-605.
- ↑ Noyes MP, Lädermann A, Denard PJ. Functional Outcome and Healing of Large and Massive Rotator Cuff Tears Repaired With a Load-Sharing Rip-Stop Construct. Arthroscopy. 2017 Sep;33(9):1654-1658.
- ↑ Denard PJ, Burkhart SS. A load-sharing rip-stop fixation construct for arthroscopic rotator cuff repair. Arthrosc Tech 2012;1:e37-42.
- ↑ Lo IK, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy 2004;20:250-67.
- ↑ Burkhart SS, Danaceau SM, Pearce CE, Jr. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy 2001;17:905-12.
- ↑ Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet 1982;154:667-72.
- ↑ Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2000;82:505-15.
- ↑ Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 2010;26:417-24.
- ↑ Lädermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. International orthopaedics 2015;39:2403-14.
- ↑ Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202.
- ↑ Dodson CC, Bedi A, Sahai A, Potter HG, Cordasco FA. Complete rotator cuff tendon avulsion and glenohumeral joint incarceration in a young patient: A case report. J Shoulder Elbow Surg. 2010;19(2):e9–e12
- ↑ Albritton MJ, Graham RD, Richards RS, 2nd, Basamania CJ. An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. J Shoulder Elbow Surg 2003;12:497-500.
- ↑ Collin P, Treseder T, Lädermann A, et al. Neuropathy of the suprascapular nerve and massive rotator cuff tears: a prospective electromyographic study. J Shoulder Elbow Surg 2014;23:28-34.
- ↑ Berhouet J, Collin P, Benkalfate T, et al. Massive rotator cuff tears in patients younger than 65 years. Epidemiology and characteristics. Orthopaedics & traumatology, surgery & research : OTSR 2009;95:S13-8.
- ↑ Collin PG, Gain S, Nguyen Huu F, Lädermann A. Is rehabilitation effective in massive rotator cuff tears? Orthopaedics & traumatology, surgery & research : OTSR 2015;101:S203-5.
- ↑ Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am 2007;89:1928-34.
- ↑ Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg 2005;14:238-46.
- ↑ Gerber C, Rahm SA, Catanzaro S, Farshad M, Moor BK. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. J Bone Joint Surg Am 2013;95:1920-6.
- ↑ Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85.
- ↑ Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am 2007;89:1928-34.
- ↑ Collin PG, Gain S, Nguyen Huu F, Lädermann A. Is rehabilitation effective in massive rotator cuff tears? Orthopaedics & traumatology, surgery & research : OTSR 2015;101:S203-5.
- ↑ Voisin JL, Ropars M, Thomazeau H. The human acromion viewed from an evolutionary perspective. Orthopaedics & traumatology, surgery & research : OTSR 2014;100:S355-60.
- ↑ Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg 2005;14:238-46.
- ↑ Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2008;90:2423-31.
- ↑ Carbonel I, Martinez AA, Calvo A, Ripalda J, Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop 2012;36:1877-83.
- ↑ Connelly TM, Shaw A, O'Grady P. Outcome of open massive rotator cuff repairs with double-row suture knotless anchors: case series. Inter Orthop 2015.
- ↑ Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthroscopy 2012;28:909-15.
- ↑ Meyer DC, Farshad M, Amacker NA, Gerber C, Wieser K. Quantitative analysis of muscle and tendon retraction in chronic rotator cuff tears. Am J Sports Med 2012;40:606-10.
- ↑ Barber FA, Burns JP, Deutsch A, Labbe MR, Litchfield RB. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy 2012;28:8-15.
- ↑ Denard PJ, Lädermann A, Jiwani AZ, Burkhart SS. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudoparalysis. Arthroscopy 2012;28:1214-9.
- ↑ Lädermann A, Denard PJ, Burkhart SS. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy 2011;27:1620-7.
- ↑ Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthroscopy 2012;28:909-15.
- ↑ Lädermann A, Denard PJ, Burkhart SS. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy 2011;27:1620-7.
- ↑ Collin P, Abdullah A, Kherad O, Gain S, Denard PJ, Lädermann A. Prospective evaluation of clinical and radiologic factors predicting return to activity within 6 months after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 2015;24:439-45.
- ↑ Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 2005;87:1229-40.
- ↑ Cho NS, Moon SC, Jeon JW, Rhee YG. The influence of diabetes mellitus on clinical and structural outcomes after arthroscopic rotator cuff repair. Am J Sports Med 2015;43:991-7.
- ↑ Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med 2011;39:2099-107.
- ↑ Clement ND, Hallett A, MacDonald D, Howie C, McBirnie J. Does diabetes affect outcome after arthroscopic repair of the rotator cuff? J Bone Joint Surg Br 2010;92:1112-7.
- ↑ Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-Term Outcome After Structural Failure of Rotator Cuff Repairs. J Bone Joint Surg Am 2006;88:472-9.
- ↑ Trantalis JN, Boorman RS, Pletsch K, Lo IK. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy 2008;24:727-31.
- ↑ Hayashida K, Tanaka M, Koizumi K, Kakiuchi M. Characteristic retear patterns assessed by magnetic resonance imaging after arthroscopic double-row rotator cuff repair. Arthroscopy 2012;28:458-64.
- ↑ Denard PJ, Burkhart SS. Techniques for managing poor quality tissue and bone during arthroscopic rotator cuff repair. Arthroscopy 2011;27:1409-21.
- ↑ Djurasovic M, Marra G, Arroyo JS, Pollock RG, Flatow EL, Bigliani LU. Revision rotator cuff repair: factors influencing results. J Bone Joint Surg Am 2001;83-A:1849-55.
- ↑ Deniz G, Kose O, Tugay A, Guler F, Turan A. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: does it improve, halt or deteriorate? Arch Orthop Trauma Surg 2014;134:985-90.
- ↑ Park JS, Park HJ, Kim SH, Oh JH. Prognostic Factors Affecting Rotator Cuff Healing After Arthroscopic Repair in Small to Medium-sized Tears. Am J Sports Med 2015;43:2386-92.
- ↑ Cadet ER, Hsu JW, Levine WN, Bigliani LU, Ahmad CS. The relationship between greater tuberosity osteopenia and the chronicity of rotator cuff tears. J Shoulder Elbow Surg 2008;17:73-7.
- ↑ Park JS, Park HJ, Kim SH, Oh JH. Prognostic Factors Affecting Rotator Cuff Healing After Arthroscopic Repair in Small to Medium-sized Tears. Am J Sports Med 2015;43:2386-92.
- ↑ Hayashida K, Tanaka M, Koizumi K, Kakiuchi M. Characteristic retear patterns assessed by magnetic resonance imaging after arthroscopic double-row rotator cuff repair. Arthroscopy 2012;28:458-64.
- ↑ Mellado JM, Calmet J, Olona M, et al. MR assessment of the repaired rotator cuff: prevalence, size, location, and clinical relevance of tendon rerupture. European radiology 2006;16:2186-96.
- ↑ cCarron JA, Derwin KA, Bey MJ, et al. Failure with continuity in rotator cuff repair "healing". Am J Sports Med 2013;41:134-41.
- ↑ Lädermann A, Denard P, Abrassart S, Schwitzguébel A. Achilles Tendon Allograft for an Irreparable Massive Rotator Cuff Tear with Bony Deficiency of the Greater Tuberosity: A Case Report. Knee Surg Sports Traumatol Arthrosc 2016;Jan 25.
- ↑ Deniz G, Kose O, Tugay A, Guler F, Turan A. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: does it improve, halt or deteriorate? Arch Orthop Trauma Surg 2014;134:985-90.
- ↑ Hartzler RU, Sperling JW, Schleck CD, Cofield RH. Clinical and radiographic factors influencing the results of revision rotator cuff repair. International journal of shoulder surgery 2013;7:41-5.
- ↑ Nove-Josserand L, Edwards TB, O'Connor DP, Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res 2005:90-6.
- ↑ de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR American journal of roentgenology 2009;192:1701-7.
- ↑ Khazzam M, Kuhn JE, Mulligan E, et al. Magnetic resonance imaging identification of rotator cuff retears after repair: interobserver and intraobserver agreement. Am J Sports Med 2012;40:1722-7.
- ↑ Saccomanno MF, Cazzato G, Fodale M, Sircana G, Milano G. Magnetic resonance imaging criteria for the assessment of the rotator cuff after repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 2015;23:423-42.
- ↑ Motamedi AR, Urrea LH, Hancock RE, Hawkins RJ, Ho C. Accuracy of magnetic resonance imaging in determining the presence and size of recurrent rotator cuff tears. J Shoulder Elbow Surg 2002;11:6-10.
- ↑ Khazzam M, Kuhn JE, Mulligan E, et al. Magnetic resonance imaging identification of rotator cuff retears after repair: interobserver and intraobserver agreement. Am J Sports Med 2012;40:1722-7.
- ↑ Zanetti M, Hodler J. MR imaging of the shoulder after surgery. Radiologic clinics of North America 2006;44:537-51, viii.
- ↑ Tudisco C, Bisicchia S, Savarese E, et al. Single-row vs. double-row arthroscopic rotator cuff repair: clinical and 3 Tesla MR arthrography results. BMC musculoskeletal disorders 2013;14:43.
- ↑ Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experimental rotator cuff repair. A preliminary study. J Bone Joint Surg Am 1999;81:1281-90.
- ↑ Ok JH, Kim YS, Kim JM, Yoo TW. Learning curve of office-based ultrasonography for rotator cuff tendons tears. Knee Surg Sports Traumatol Arthrosc 2013;21:1593-7.
- ↑ Nazarian LN, Jacobson JA, Benson CB, et al. Imaging algorithms for evaluating suspected rotator cuff disease: Society of Radiologists in Ultrasound consensus conference statement. Radiology 2013;267:589-95.
- ↑ Kluger R, Bock P, Mittlbock M, Krampla W, Engel A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med 2011;39:2071-81.
- ↑ Miller BS, Downie BK, Kohen RB, et al. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med 2011;39:2064-70.
- ↑ Barth J, Fotiadis E, Barthelemy R, Genna S, Saffarini M. Ultrasonic evaluation of the repair integrity can predict functional outcomes after arthroscopic double-row rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 2015;23:376-85.
- ↑ Iannotti JP, Deutsch A, Green A, et al. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am 2013;95:965-71.
- ↑ Kim JH, Hong IT, Ryu KJ, Bong ST, Lee YS, Kim JH. Retear rate in the late postoperative period after arthroscopic rotator cuff repair. Am J Sports Med 2014;42:2606-13.
- ↑ Codsi MJ, Rodeo SA, Scalise JJ, Moorehead TM, Ma CB. Assessment of rotator cuff repair integrity using ultrasound and magnetic resonance imaging in a multicenter study. J Shoulder Elbow Surg 2014;23:1468-72.
- ↑ Collin P, Yoshida M, Delarue A, et al. Evaluating postoperative rotator cuff healing: Prospective comparison of MRI and ultrasound. Orthopaedics & traumatology, surgery & research : OTSR 2015;101:S265-8.
- ↑ Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-Term Outcome After Structural Failure of Rotator Cuff Repairs. J Bone Joint Surg Am 2006;88:472-9.
- ↑ Paxton ES, Teefey SA, Dahiya N, Keener JD, Yamaguchi K, Galatz LM. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: minimum ten-year follow-up. J Bone Joint Surg Am 2013;95:627-32.
- ↑ Noyes MP, Lädermann A, Denard PJ. Functional Outcome and Healing of Large and Massive Rotator Cuff Tears Repaired With a Load-Sharing Rip-Stop Construct. Arthroscopy. 2017 Sep;33(9):1654-1658
- ↑ Denard PJ, Lädermann A, Brady PC, et al. Pseudoparalysis From a Massive Rotator Cuff Tear Is Reliably Reversed With an Arthroscopic Rotator Cuff Repair in Patients Without Preoperative Glenohumeral Arthritis. Am J Sports Med 2015;43:2373-8.
- ↑ Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009;18:600-6.
- ↑ Hartzler RU, Sperling JW, Schleck CD, Cofield RH. Clinical and radiographic factors influencing the results of revision rotator cuff repair. International journal of shoulder surgery 2013;7:41-5.
- ↑ Agrawal V. Healing rates for challenging rotator cuff tears utilizing an acellular human dermal reinforcement graft. International journal of shoulder surgery 2012;6:36-44.
- ↑ Lenart BA, Martens KA, Kearns KA, Gillespie RJ, Zoga AC, Williams GR. Treatment of massive and recurrent rotator cuff tears augmented with a poly-l-lactide graft, a preliminary study. J Shoulder Elbow Surg 2015;24:915-21.
- ↑ Keener JD, Wei AS, Kim HM, et al. Revision arthroscopic rotator cuff repair: repair integrity and clinical outcome. J Bone Joint Surg Am 2010;92:590-8.
- ↑ Shamsudin A, Lam PH, Peters K, Rubenis I, Hackett L, Murrell GA. Revision versus primary arthroscopic rotator cuff repair: a 2-year analysis of outcomes in 360 patients. Am J Sports Med 2015;43:557-64.
- ↑ Shamsudin A, Lam PH, Peters K, Rubenis I, Hackett L, Murrell GA. Revision versus primary arthroscopic rotator cuff repair: a 2-year analysis of outcomes in 360 patients. Am J Sports Med 2015;43:557-64.
- ↑ Vastamaki M, Lohman M, Borgmastars N. Rotator cuff integrity correlates with clinical and functional results at a minimum 16 years after open repair. Clin Orthop Relat Res 2013;471:554-61.
- ↑ Namdari S, Donegan RP, Chamberlain AM, Galatz LM, Yamaguchi K, Keener JD. Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg Am 2014;96:99-105.
- ↑ Chuang MJ, Jancosko J, Nottage WM. Clinical outcomes of single-row arthroscopic revision rotator cuff repair. Orthopedics 2014;37:e692-8.
- ↑ Piasecki DP, Verma NN, Nho SJ, et al. Outcomes after arthroscopic revision rotator cuff repair. Am J Sports Med 2010;38:40-6.
- ↑ Lädermann A, Denard PJ, Burkhart SS. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy 2011;27:1620-7.
- ↑ Denard PJ, Lädermann A, Jiwani AZ, Burkhart SS. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudoparalysis. Arthroscopy 2012;28:1214-9.
- ↑ Chuang MJ, Jancosko J, Nottage WM. Clinical outcomes of single-row arthroscopic revision rotator cuff repair. Orthopedics 2014;37:e692-8.
- ↑ Piasecki DP, Verma NN, Nho SJ, et al. Outcomes after arthroscopic revision rotator cuff repair. Am J Sports Med 2010;38:40-6.
- ↑ Hartzler RU, Sperling JW, Schleck CD, Cofield RH. Clinical and radiographic factors influencing the results of revision rotator cuff repair. International journal of shoulder surgery 2013;7:41-5.
- ↑ Lädermann A, Denard PJ, Burkhart SS. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy 2011;27:1620-7.
- ↑ Piasecki DP, Verma NN, Nho SJ, et al. Outcomes after arthroscopic revision rotator cuff repair. Am J Sports Med 2010;38:40-6.
- ↑ Djurasovic M, Marra G, Arroyo JS, Pollock RG, Flatow EL, Bigliani LU. Revision rotator cuff repair: factors influencing results. J Bone Joint Surg Am 2001;83-A:1849-55.
- ↑ Lo IK, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy 2004;20:250-67.
- ↑ Lädermann A, Denard PJ, Burkhart SS. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy 2011;27:1620-7.
- ↑ Trantalis JN, Boorman RS, Pletsch K, Lo IK. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy 2008;24:727-31.
- ↑ Loew M, Magosch P, Lichtenberg S, Habermeyer P, Porschke F. How to discriminate between acute traumatic and chronic degenerative rotator cuff lesions: an analysis of specific criteria on radiography and magnetic resonance imaging. J Shoulder Elbow Surg 2015;24:1685-93.
- ↑ Fleckenstein JL, Watumull D, Conner KE, et al. Denervated human skeletal muscle: MR imaging evaluation. Radiology 1993;187:213-8.
- ↑ Lädermann A, Denard PJ, Kolo FC. A new tear pattern of the rotator cuff and its treatment: Fosbury flop tears. International journal of shoulder surgery 2015;9:9-12.
- ↑ Lädermann A, Denard PJ, Kolo FC. A new tear pattern of the rotator cuff and its treatment: Fosbury flop tears. International journal of shoulder surgery 2015;9:9-12.
- ↑ Nakamizo H. Arthroscopic repair for subacromial incarceration of a torn rotator cuff. AP-SMART 2015;2:90-4.
- ↑ Romeo AA, Loutzenheiser T, Rhee YG, Sidles JA, Harryman DT, 2nd, Matsen FA, 3rd. The humeroscapular motion interface. Clin Orthop Relat Res 1998:120-7.
- ↑ Taneja AK, Kattapuram SV, Chang CY, Simeone FJ, Bredella MA, Torriani M. MRI findings of rotator cuff myotendinous junction injury. AJR American journal of roentgenology 2014;203:406-11.
- ↑ Zarins B, Ciullo JV. ACute muscle and tendon injuries in athletes. Clinics in sports medicine 1983;2:167-82.
- ↑ Ludig T, Walter F, Chapuis D, Mole D, Roland J, Blum A. MR imaging evaluation of suprascapular nerve entrapment. European radiology 2001;11:2161-9.
- ↑ Bredella MA, Tirman PF, Fritz RC, Wischer TK, Stork A, Genant HK. Denervation syndromes of the shoulder girdle: MR imaging with electrophysiologic correlation. Skeletal radiology 1999;28:567-72.
- ↑ Walch G, Nove-Josserand L, Liotard JP, Noel E. Musculotendinous infraspinatus ruptures: an overview. Orthopaedics & traumatology, surgery & research : OTSR 2009;95:463-70.
- ↑ Hertel R, Lambert SM. Supraspinatus rupture at the musculotendinous junction. J Shoulder Elbow Surg 1998;7:432-5.
- ↑ Lädermann A, Christophe FK, Denard PJ, Walch G. Supraspinatus rupture at the musclotendinous junction: an uncommonly recognized phenomenon. J Shoulder Elbow Surg 2012;21:72-6.
- ↑ Tirefort J, Cunningham G, Lädermann A. Reverse Fosbury Flop Tear of the Rotator Cuff. Case Reports in Orthopedics 2017;2017:3635897.
- ↑ Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994:78-83.
- ↑ Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 1999;8:599-605.
- ↑ Melis B, Nemoz C, Walch G. Muscle fatty infiltration in rotator cuff tears: descriptive analysis of 1688 cases. Orthopaedics & traumatology, surgery & research : OTSR 2009;95:319-24.
- ↑ Williams MD, Lädermann A, Melis B, Barthelemy R, Walch G. Fatty infiltration of the supraspinatus: a reliability study. J Shoulder Elbow Surg 2009;18:581-7.
- ↑ Kissenberth MJ, Rulewicz GJ, Hamilton SC, Bruch HE, Hawkins RJ. A positive tangent sign predicts the repairability of rotator cuff tears. J Shoulder Elbow Surg 2014;23:1023-7.
- ↑ Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 1996;67:264-8.
- ↑ Sheean AJ, Hartzler RU, Denard PJ, et al. Preoperative Radiographic Risk Factors for Incomplete Arthroscopic Supraspinatus Tendon Repair in Massive Rotator Cuff Tears. Arthroscopy 2018;34:1121-7.
- ↑ Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res 2010;468:1498-505.
- ↑ Collin P, Treseder T, Lädermann A, et al. Neuropathy of the suprascapular nerve and massive rotator cuff tears: a prospective electromyographic study. J Shoulder Elbow Surg 2014;23:28-34.
- ↑ Lädermann A, Genevay M, Abrassart S, Schwitzguebel AJ. Supraspinatus Intramuscular Calcified Hematoma or Necrosis Associated with Tendon Tear. Case Rep Orthop 2015;2015:496313.
- ↑ Sheean AJ, Hartzler RU, Denard PJ, et al. Preoperative Radiographic Risk Factors for Incomplete Arthroscopic Supraspinatus Tendon Repair in Massive Rotator Cuff Tears. Arthroscopy 2018;34:1121-7.
- ↑ Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87:1476-86.
- ↑ Tokish JM, Alexander TC, Kissenberth MJ, Hawkins RJ. Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg 2017;26:e177-e87.
- ↑ Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202.
- ↑ Axe JM. Tendon transfers for irreparable rotator cuff tears: An update. EFORT Open Rev 2016;1:18-24.
- ↑ Levy O, Mullett H, Roberts S, Copeland S. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elbow Surg 2008;17:863-70.
- ↑ Collin PG, Gain S, Nguyen Huu F, Lädermann A. Is rehabilitation effective in massive rotator cuff tears? Orthopaedics & traumatology, surgery & research : OTSR 2015;101:S203-5.
- ↑ Ainsworth R. Physiotherapy rehabilitation in patients with massive, irreparable rotator cuff tears. Musculoskeletal care 2006;4:140-51.
- ↑ Levy O, Mullett H, Roberts S, Copeland S. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elbow Surg 2008;17:863-70.
- ↑ Yian EH, Sodl JF, Dionysian E, Schneeberger AG. Anterior deltoid reeducation for irreparable rotator cuff tears revisited. J Shoulder Elbow Surg 2017;26:1562-5.
- ↑ Collin PG, Gain S, Nguyen Huu F, Lädermann A. Is rehabilitation effective in massive rotator cuff tears? Orthopaedics & traumatology, surgery & research : OTSR 2015;101:S203-5.
- ↑ Boileau P, Maynou C, Balestro JC, et al. [Long head of the biceps pathology]. Rev Chir Orthop Reparatrice Appar Mot 2007;93:5S19-53.
- ↑ Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg 2005;14:238-46.
- ↑ Boileau P, Baque F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am 2007;89:747-57.
- ↑ Scheibel M, Lichtenberg S, Habermeyer P. Reversed arthroscopic subacromial decompression for massive rotator cuff tears. J Shoulder Elbow Surg 2004;13:272-8.
- ↑ Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol 2010;11:13-20.
- ↑ Chen KH, Chiang ER, Wang HY, Ma HL. Arthroscopic Partial Repair of Irreparable Rotator Cuff Tears: Factors Related to Greater Degree of Clinical Improvement at 2 Years of Follow-Up. Arthroscopy 2017;33:1949-55.
- ↑ Cuff DJ, Pupello DR, Santoni BG. Partial rotator cuff repair and biceps tenotomy for the treatment of patients with massive cuff tears and retained overhead elevation: midterm outcomes with a minimum 5 years of follow-up. J Shoulder Elbow Surg 2016;25:1803-9.
- ↑ Galasso O, Riccelli DA, De Gori M, et al. Quality of Life and Functional Results of Arthroscopic Partial Repair of Irreparable Rotator Cuff Tears. Arthroscopy 2017;33:261-8.
- ↑ Godeneche A, Freychet B, Lanzetti RM, Clechet J, Carrillon Y, Saffarini M. Should massive rotator cuff tears be reconstructed even when only partially repairable? Knee Surg Sports Traumatol Arthrosc 2017;25:2164-73.
- ↑ Henry P, Wasserstein D, Park S, et al. Arthroscopic Repair for Chronic Massive Rotator Cuff Tears: A Systematic Review. Arthroscopy 2015;31:2472-80.
- ↑ Shon MS, Koh KH, Lim TK, Kim WJ, Kim KC, Yoo JC. Arthroscopic Partial Repair of Irreparable Rotator Cuff Tears: Preoperative Factors Associated With Outcome Deterioration Over 2 Years. Am J Sports Med 2015;43:1965-75.
- ↑ Yoo JC, Ahn JH, Koh KH, Lim KS. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy 2009;25:1093-100.
- ↑ L’Episcopo J. Tendon transplantation in obstetrical paralysis. Am J Surg 1934;25:122-5.
- ↑ Boileau P, Baba M, McClelland WB, Jr., Thelu CE, Trojani C, Bronsard N. Isolated loss of active external rotation: a distinct entity and results of L'Episcopo tendon transfer. J Shoulder Elbow Surg 2017.
- ↑ Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Relat Res 1992:152-60.
- ↑ Gerber C, Pennington SD, Lingenfelter EJ, Sukthankar A. Reverse Delta-III total shoulder replacement combined with latissimus dorsi transfer. A preliminary report. J Bone Joint Surg Am 2007;89:940-7.
- ↑ Costouros JG, Espinosa N, Schmid MR, Gerber C. Teres minor integrity predicts outcome of latissimus dorsi tendon transfer for irreparable rotator cuff tears. J Shoulder Elbow Surg 2007;16:727-34.
- ↑ Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am 2012;94:891-8.
- ↑ Grimberg J, Kany J, Valenti P, Amaravathi R, Ramalingam AT. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthroscopy 2015;31:599-607 e1.
- ↑ Bonnevialle N, Joudet T. [Massive Rotator Cuff Lesions]. Société Francophone d'Arthroscopie. Marseille2017.
- ↑ Gerber C, Rahm SA, Catanzaro S, Farshad M, Moor BK. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. J Bone Joint Surg Am 2013;95:1920-6.
- ↑ Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202.
- ↑ Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013;29:459-70.
- ↑ Burkhart SS, Denard PJ, Adams CR, Brady PC, Hartzler RU. Arthroscopic Superior Capsular Reconstruction for Massive Irreparable Rotator Cuff Repair. Arthrosc Tech 2016;5:e1407-e18.
- ↑ Boutsiadis A, Chen S, Jiang C, Lenoir H, Delsol P, Barth J. Long Head of the Biceps as a Suitable Available Local Tissue Autograft for Superior Capsular Reconstruction: “The Chinese Way”. Arthroscopy Techniques 2017.
- ↑ Pouliart N, Somers K, Eid S, Gagey O. Variations in the superior capsuloligamentous complex and description of a new ligament. J Shoulder Elbow Surg 2007;16:821-36.
- ↑ Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013;29:459-70.
- ↑ Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy 2018;34:93-9.
- ↑ Senekovic V, Poberaj B, Kovacic L, et al. The biodegradable spacer as a novel treatment modality for massive rotator cuff tears: a prospective study with 5-year follow-up. Arch Orthop Trauma Surg 2017;137:95-103.
- ↑ Deranlot J, Herisson O, Nourissat G, et al. Arthroscopic Subacromial Spacer Implantation in Patients With Massive Irreparable Rotator Cuff Tears: Clinical and Radiographic Results of 39 Retrospectives Cases. Arthroscopy 2017;33:1639-44.
- ↑ Lewington MR, Ferguson DP, Smith TD, Burks R, Coady C, Wong IH. Graft Utilization in the Bridging Reconstruction of Irreparable Rotator Cuff Tears: A Systematic Review. Am J Sports Med 2017;45:3149-57.
- ↑ Petrillo S, Longo UG, Papalia R, Denaro V. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: a systematic review. Musculoskelet Surg 2017;101:105-12.
- ↑ Sevivas N, Ferreira N, Andrade R, et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: a systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg 2017;26:e265-e77.
- ↑ Kang JR, Sin AT, Cheung EV. Treatment of Massive Irreparable Rotator Cuff Tears: A Cost-effectiveness Analysis. Orthopedics 2017;40:e65-e76.
- ↑ Lädermann A, Denard PJ, Tirefort J, Collin P, Nowak A, Schwitzguebel AJ. Subscapularis- and deltoid-sparing vs traditional deltopectoral approach in reverse shoulder arthroplasty: a prospective case-control study. Journal of orthopaedic surgery and research 2017;12:112.
- ↑ Lädermann A, Lo EY, Schwitzguebel AJ, Yates E. Subscapularis and deltoid preserving anterior approach for reverse shoulder arthroplasty. Orthopaedics & traumatology, surgery & research : OTSR 2016;102:905-8.
- ↑ Ernstbrunner L, Suter A, Catanzaro S, Rahm S, Gerber C. Reverse Total Shoulder Arthroplasty for Massive, Irreparable Rotator Cuff Tears Before the Age of 60 Years: Long-Term Results. J Bone Joint Surg Am 2017;99:1721-9.
- ↑ Virk MS, Nicholson GP, Romeo AA. Irreparable Rotator Cuff Tears Without Arthritis Treated With Reverse Total Shoulder Arthroplasty. Open Orthop J 2016;10:296-308.