Difference between revisions of "Shoulder:Disorders of the Acromioclavicular Joint"
m (→Bullet Points) |
|||
| Line 1: | Line 1: | ||
| − | ==Bullet Points | + | ==Bullet Points: Osteology: The acromioclavicular joint is a diarthrodial joint fibrocartilaginous. The intraarticular disc is located between the osseous segments.== |
| − | |||
| − | |||
*Stability: The acromioclavicular ligament (superior, inferior, anterior, and posterior components) provides horizontal stability. The superior ligament is strongest, followed by posterior. The coracoclavicular ligaments (trapezoid and conoid) provides vertical stability. The trapezoid inserts 2.5 cm from end of clavicle. It is a stabilizer against horizontal and vertical loads. The conoid inserts 4.6 cm from end of clavicle in the posterior border more important ligament vertical stabilizer of acromioclavicular joint. The normal coracoclavicular distance (superior coracoid to inferior clavicle) is 11-13 mm. The deltotrapezial fascia, capsule, deltoid and trapezius act as additional stabilizers | *Stability: The acromioclavicular ligament (superior, inferior, anterior, and posterior components) provides horizontal stability. The superior ligament is strongest, followed by posterior. The coracoclavicular ligaments (trapezoid and conoid) provides vertical stability. The trapezoid inserts 2.5 cm from end of clavicle. It is a stabilizer against horizontal and vertical loads. The conoid inserts 4.6 cm from end of clavicle in the posterior border more important ligament vertical stabilizer of acromioclavicular joint. The normal coracoclavicular distance (superior coracoid to inferior clavicle) is 11-13 mm. The deltotrapezial fascia, capsule, deltoid and trapezius act as additional stabilizers | ||
*Arthritis: The rate of asymptomatic acromioclavicular joint arthritis is high (65%) found the age of 40. | *Arthritis: The rate of asymptomatic acromioclavicular joint arthritis is high (65%) found the age of 40. | ||
*Distal clavicular osteolysis: this condition is classically seen in body builders. | *Distal clavicular osteolysis: this condition is classically seen in body builders. | ||
| − | *Acromioclavicular joint dislocation: Surgery | + | *Acromioclavicular joint dislocation: Surgery might be considered only in high grade (4-5). |
<br /> | <br /> | ||
| Line 81: | Line 79: | ||
<br /> | <br /> | ||
===History=== | ===History=== | ||
| − | Open distal clavicle resection was reported separately in 1941 by Mumford | + | Open distal clavicle resection was reported separately in 1941 by Mumford<ref>Mumford E. Acromioclavicular dislocation: a new treatment. J Bone Joint Surg Am 1941;23:799–802.</ref> and Gurd.<ref>Gurd FB. The Treatment of Complete Dislocation of the Outer End of the Clavicle: An Hitherto Undescribed Operation. Annals of surgery 1941;113:1094-8.</ref> |
<br /> | <br /> | ||
Revision as of 07:34, 27 December 2020
Contents
- 1 Bullet Points: Osteology: The acromioclavicular joint is a diarthrodial joint fibrocartilaginous. The intraarticular disc is located between the osseous segments.
- 2 Key words
- 3 Anatomical Considerations
- 4 Biomechanics of the Acromioclavicular Joint
- 5 Radiological or Radiographic Evaluation of the Acromioclavicular Joint
- 6 Arthritis
- 7 SAPHO syndrome
- 8 Distal Clavicular Osteolysis
- 9 Operative Treatment of Arthritis, SAPHO and Distal Clavicle Osteolysis
- 10 Acromioclavicular Joint Dislocation
- 11 Classification
- 12 Scores
- 13 Treatment option
- 14 Postoperative Rehabilitation
- 15 Complications
- 16 References
Bullet Points: Osteology: The acromioclavicular joint is a diarthrodial joint fibrocartilaginous. The intraarticular disc is located between the osseous segments.
- Stability: The acromioclavicular ligament (superior, inferior, anterior, and posterior components) provides horizontal stability. The superior ligament is strongest, followed by posterior. The coracoclavicular ligaments (trapezoid and conoid) provides vertical stability. The trapezoid inserts 2.5 cm from end of clavicle. It is a stabilizer against horizontal and vertical loads. The conoid inserts 4.6 cm from end of clavicle in the posterior border more important ligament vertical stabilizer of acromioclavicular joint. The normal coracoclavicular distance (superior coracoid to inferior clavicle) is 11-13 mm. The deltotrapezial fascia, capsule, deltoid and trapezius act as additional stabilizers
- Arthritis: The rate of asymptomatic acromioclavicular joint arthritis is high (65%) found the age of 40.
- Distal clavicular osteolysis: this condition is classically seen in body builders.
- Acromioclavicular joint dislocation: Surgery might be considered only in high grade (4-5).
Key words
Acromioclavicular joint; Anatomy; Biomechanics; Arthritis; Distal clavicular osteolysis; Instability; Dislocation; Separation; Imaging; SAPHO syndrome; Distal clavicular osteolysis; Gorham-Stout disease; Conservative; Nonoperative Treatment; Stabilization; Reconstruction: Coracoclavicular cerclage; Mazzocca; Acute; Chronic; Complication.
Anatomical Considerations
The acromioclavicular joint that anchors the clavicle to the scapula. It is a diarthrodial joint that primarily rotates as well as translates in the anterior-posterior and the superior-inferior planes. The joint is surrounded by a capsule with synovium and an articular surface that is made up of hyaline cartilage containing an intra-articular meniscus-type structure. The mean width of the articular surface is 24.3+/-3 mm (range, 17-30 mm) for the acromial side and 24.6+/-3 mm (range, 17-30 mm) for the clavicular side.1 The mean anterior overhang of the acromion (anterior acromion-anterior joint distance) is 2.6+/-2.6 mm (range, 0-10 mm), whereas the mean anterior oversize of the clavicle (anterior clavicle-anterior joint distance) is 2.2+/-1.9 mm (range, 0-5 mm) (Figure). Only 60% of the acromioclavicular joints are aligned anteriorly, 3% have minor overhang of the acromion, 3% have minor overhang of the clavicle, 24% have major overhang of the acromion, and 10% have major overhang of the clavicle (Figure). Therefore, major misalignment anteriorly is found in 34% of the cases. The only reliable landmarks are the articular facets of both the acromion and the clavicle.[1] The center of the conoid ligament inserts under the posterior part of the clavicle 46 mm medially to the acromioclavicular joint. The center of the trapezoid ligament has an anterior insertion under the clavicle, 25 mm medially to the acromioclavicular joint.[2][3][4][5] The normal coracoclavicular distance (superior coracoid to inferior clavicle) is 11-13 mm. The acromioclavicular joint has dual innervation from both the suprascapular nerve and the lateral pectoral nerve.

Biomechanics of the Acromioclavicular Joint
The acromioclavicular joint is stabilized both by static and dynamic stabilizers. The static stabilizers include 1) the four acromioclavicular ligaments (superior, inferior, anterior, and posterior), 2) the lateral coracoclavicular ligaments (conoid and trapezoid), 3) the medial coracoclavicular ligaments (Figure and Video) and 4) the coracoacromial ligament.[6][7] The latter, when transferred during standard Weaver-Dunn repair is only 1/4 as strong as the intact coracoclavicular ligaments; such technique of stabilization do not provide sufficient strength and is considered by many as obsolete.[8][9][10]
 Medial coracoclavicular ligament (asterisk) in a right shoulder region. View from in front. C clavicle, CP coracoid process (horizontal portion), DM deltoid muscle (resected), PM pectoralis minor, SM subclavius muscle. Reprinted from Stimec et al.,[6] with permission. |
The capsular ligaments acted as a primary restraint to posterior displacement of the clavicle (Video).[11]
The superior ligament is strongest, followed by posterior. Both ligaments provide the most restraint to posterior translation of the acromioclavicular joint and must be preserved during a Mumford procedure. The coracoclavicular ligaments (trapezoid and conoid) provides vertical stability. The dynamic stabilizers include the deltoid and trapezius muscles.[12]
The coracoclavicular ligaments’ main contribution is to vertical stability. However, its double bundle configuration contributes also partially to horizontal stability due to their relative orientation.[13][14]
After lesion of the acromioclavicular ligaments, the conoid ligament acts as the primary restraint against anterior and superior loading, while the trapezoid functioned as the primary restraint against posterior loading.[15] When a load is applied in a superior direction, the conoid ligament fails first in its midsubstance region.[16] [17]
During elevation of the arm, the clavicle with respect to the thorax generally undergoes elevation (11-15 degrees), retraction (15 -29 degrees), and posterior long-axis rotation (15-31 degrees). Motion of the scapula (protraction-retraction) plays a major role in the motion at the acromioclavicular joint.[18]
Radiological or Radiographic Evaluation of the Acromioclavicular Joint
X-ray
Proper radiographic evaluation of the acromioclavicular joint requires multiple views. Zanca view is performed by tilting the x-ray beam 10° to 15° toward the cephalic direction. This view allows to analyze the acromioclavicular joint as well as the coracoclavicular (CC) interspace.[19] The average distance between the clavicle and coracoid process is usually between 1.1 to 1.3 cm.[20] An increase in the coracoclavicular distance of 25% to 50% over the normal side indicated complete coracoclavicular ligament disruption.[21]
Ultrasound
Acromioclavicular joint pathology is relatively easy to analyze using ultrasound imaging. Pathological signs can be detected (osteophytes, erosions, effusion and geyser phenomenon, being a large synovial cyst extending into the supraclavicular fossa) (Figure) and joint tenderness evaluated by applying pressure on the probe whilst above the joint line. Dynamic analysis (the patient’s arm being brought from neutral position to a “cross arm” position) can reveal joint subluxation. This tool is also useful to guide intra-articular cortisone injection.[26]

Magnetic Resonance Imaging (MRI)
Magnetic. resonance imaging (MRI) allows excellent anatomical display of acromioclavicular joint structures and can give clinically relevant information on the type and extension of acromioclavicular joint trauma and associated pathologies, which may influence treatment.[28] However it is not feasible for use on a routine basis because of its costs and limited local availability. Magnetic. resonance imaging (MRI) is not helpful in making the diagnosis of symptomatic acromioclavicular joint arthritis. A focused history and clinical examination remain the mainstay for surgical decision making.[29]
Arthritis
Prevalence
The hyaline articular cartilage becomes fibrocartilage on the acromial side of the joint by the age of 17 and on the clavicular side by the age of 24. The meniscus undergoes afterwards rapid degeneration and is no longer functional beyond the 4th decade.[30] This could explain the high rate of asymptomatic acromioclavicular joint arthritis (65%) found after the age of 40 (Figure). Consequently, acromioclavicular joint width varies between 1 and 3 mm in the young adult and 0.5 mm in 60-year-old patients.[31] The condition can be associated to an arthrosynovial cyst (Figures).
SAPHO syndrome
Synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) is an acronym for various osteoarticular and dermatological manifestations that can appear in the same patient. It is a rare autoimmune disease of unknown cause, which due to its clinical presentation and symptoms is often misdiagnosed and unrecognized.[32] It is estimated that about 50-70% of patients who might have SAPHO, also suffer from shoulder girdle pain including acromioclavicular joint. These characteristics are related to an underlying chronic inflammatory sterile osteitis resulting in swelling, tenderness and pain of bone structures and adjacent tissues.[33] Therapy is empirical and aimed at easing pain and modifying the inflammatory process. It includes nonsteroidal anti-inflammatory drugs (NSAIDs) as the first-line agents. Antibiotics, corticosteroids, disease-modifying anti-rheumatic drugs, biologicals targeting tumor necrosis factor alpha or interleukin-1, and bisphosphonates have all been used with variable success. Surgery is reserved to treat complications.[34]
Distal Clavicular Osteolysis
Dupas et al. first describe in 1936 osteolysis in the distal clavicle as a result of trauma. Even if a trauma is not necessary, this condition is mainly found in weight trainers,[35] judo player, handball player (Figure).[36][37]
Operative Treatment of Arthritis, SAPHO and Distal Clavicle Osteolysis
A patient whose condition does not respond to conservative management or who is unwilling to alter his or her exercise training and performance regimen require surgery.
History
Open distal clavicle resection was reported separately in 1941 by Mumford[42] and Gurd.[43]
Arthroscopic Distal Clavicle Excision
Indication/Contraindication
This procedure is only indicated if there acromioclavicular pain (most of acromioclavicular arthritis are not painful). Joint instability is a contraindication.
Operative technique
Perform a subacromial bursectomy along with excision of the medial fibrofatty tissue around the distal clavicle and the scapular spine. The acromioclavicular joint is then expose using instrumentation through an anterior working portal. First remove using a power burr through an anterior portal 2-3 mm of the acromion (bipolar disease necessitate bipolar resection).[44]
This will improve visualization of the distal clavicle, and then resect 7 mm of the clavicle. It is important to preserve at least one of the acromioclavicular ligaments, if possible the superior that contributes for 56% (versus 25% for the posterior) of the resistance to posterior displacement of the clavicle. The end-point is to create a 1 cm space. The use of a 70° scope through the posterior or the anterolateral portal allows a better view of the superior part of the joint.
Coplaning of Distal Clavicle
Indication
Coplaning of distal clavicle is indication when the acromioclavicular joint is not painful but associated to a prominent inferior osteophyte that make an impression on the musculotendinous junction of the supraspinatus. The latter osteophyte might be responsible for musculotendinous junction lesion.[45] It is important to limit the removal of inferior clavicle osteophytes, to avoid partial resection of the distal clavicle that could destabilize the joint and generate more pain.[46]
Operative Technique
If an acromioplasty is indicated, begin by acromioplasty first. All soft tissue from the undersurface of the distal clavicle must be cleaned while viewing through a posterior or a lateral portal. Coplaning of the distal clavicle is achieved by alternately viewing through a posterior portal while using a burr through a lateral portal, then viewing through a lateral portal while using a burr through an anterolateral or an anterior portal.
Postoperative Care
Isolated distal clavicle excision or coplaning do not require any type of postoperative immobilization. Range of motion is regained actively the day after the surgery. Day life activities then begins according to the pain. Light sports such as brake stroke is authorized after two to four weeks. Strengthening is not recommended.
Acromioclavicular Joint Dislocation
Prevalence
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
Mechanism
Two common mechanisms account for acromioclavicular joint injury. Direct injuries occur during falls or blow onto acromioclavicular joint with the arm in the adducted position. Indirect injury occurs as the result of a fall on an outstretched hand driving the humeral head into the acromion.
Physical Examination
Swelling, deformity and tenderness locally at the acromioclavicular joint are observed.
| Left acromioclavicular joint dislocation | Superior view | Posterior view |
Instability should be tested dynamically and in all planes (Video).
Reducibility of the dislocation should be tested if not too painful (Video). These are the most reliable symptoms/signs. The cross body adduction stress is performed with the arm elevated to 90 degrees and then adducted across the chest. This produce pain specifically at the acromioclavicular joint due to compression across the joint and may reveal posterior intricateness of the clavicle in the trapezius (Video).
Classification
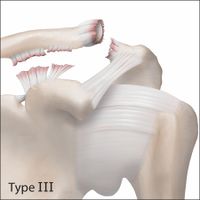
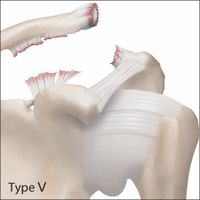
The radiographic classification of acromioclavicular joint injuries described by Rockwood includes six types:
|
Type VI Injuries are inferior acromioclavicular joint dislocations into a subacromial or subcoracoid position. |
The Rockwood classification based on the severity of the radiological displacement on both planes (vertical and horizontal planes) is widely accepted by the shoulder trauma surgeon community for the decision making, despite the low reliability.[47][48] Cho et al. demonstrated an overall lack of reliability of the Rockwood classification of acromioclavicular joint dislocations and of decisions regarding their treatment. There is especially poor agreement between experienced shoulder surgeons. The addition of 3D CT did not improve reliability of classification and treatment of acromioclavicular joint dislocations.[49]
The ISAKOS consensus group has recently further expanded this classification by suggesting the addition of subgroups of the type III lesions. The IIIA (stable) and IIIB (unstable) in an effort to provide effective guidance in the management of this group of injuries. The subclassification criteria are rather clinical with the unstable type IIIB lesions presenting with continuous pain, rotator cuff weakness, diminished abduction range of motion, and scapular dyskinesis. Differentiation between IIIA and IIIB on a radiographic basis is important as it may guide the doctor towards a treatment strategy. The acromial center line to dorsal clavicle (AC-DC) measurement and use of the Alexander view provides the clinician with a more realistic appreciation of true AC joint displacement, especially in defining watershed cases (ie, IIIA/IIB/IV) and may better inform the decision-making process regarding management options and recommendations.
Scores
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
Treatment option
The main goals of treatment, whether surgical or non-surgical, are to achieve a pain-free shoulder with full range of motion, normal strength, and no limitations in activities. The demands on the shoulder will differ from patient to patient, and these demands should be considered during the initial evaluation.
Conservative Treatment (Nonoperative Treatment)
All types of acromioclavicular joint dislocation can be treated non-surgically, at least at the beginning. The actual surgical recommendations are mainly based on small retrospective series or obsolete techniques. There is nowadays no formal indication for acute reconstructions. The rare exceptions are open acromioclavicular dislocation, or dislocation associated to Ideberg III to V glenoid fractures, floating shoulders,…
In case of treatment failure of neglected acromioclavicular dislocation, secondary reconstructions is still possible and gives actually results as good as primary treatment. Consequently, evaluation must be done on a case-by-case basis, taking into account hand dominance, occupation, labor, sport, and the risk for reinjury (rudby, american football).
The rehabilitation program of acute acromioclavicular dislocation treated conservatively evolve by four different phase:[50][51]
- First, short immobilization to decrease pain and inflammation is recommended. Patients should be encouraged to cease sling use as soon as their symptoms allow. Immediate glenohumeral mobility exercises such as internal/external rotation elbow at the side and flexion/extension of the elbow are recommended to avoid potential secondary frozen shoulder. After two weeks, progressive forward elevation is encouraged. According to patient’s own pain thresholds, closed-chain exercises with the hand fixed to a wall, table, or floor starts to improve scapular control.
- Then, strengthening exercises using isotonic contractions are prescribed.
- Open-chain exercises with the goal of increasing strength, power, endurance, and neuromuscular control are progressively added. Reinforcement with diagonals exercises in which persistent deficit are observed are recommended.
- Finally, return to activity with sport-specific functional drills is allowed.
Surgical Treatment
A basic principle in the treatment of acute acromioclavicular joint dislocations is to restore joint congruity and mechanical stability as accurately as possible, in order to provide physiologic conditions for the development of rigid scar tissue healing. Acute acromioclavicular joint dislocation requires stabilization in both planes, i.e., at the coracoclavicular junction and at the acromioclavicular joint.[51][52][53][54] The weight of the upper limb should be taken into account, with six weeks of immobilization to unload the construct in patients who have high (> 25 kg/m2) body mass index values.[52] Different types of acromioclavicular reconstructions are possible and it is unclear if there is individual differences between the constructs (Figure).[55]
Open and arthroscopic AC joint reconstruction techniques have no differences in loss of reduction, the complication rate, and the revision rate based on the available literature.[56]
Open Reduction for Acute Dislocation
Surgery is performed in the beach-chair position under general anesthesia, and an interscalene regional block is often added. A saber cut incision is made from the posterior acromial angle to the coracoid process along Langer’s lines. After subcutaneous dissection, traumatic detachment of the deltoid and trapezius permits visualization of the clavicle, base of the coracoid process, acromioclavicular joint, and acromion. The base of the coracoid process is then exposed by blunt dissection, and subcoracoid transfer of 4 non-resorbable No. 6 sutures is then performed using a long clamp with a 90 degree angulation.
These sutures are then inserted in the clavicle through two 3.2 mm drill holes made to approximate the normal insertion points of the coracoclavicular ligaments (25 mm and 46 mm from lateral end of the clavicle). The sutures are passed through the bone with a shuttle relay technique and a long Mayo needle. Two knots are placed under the clavicle to avoid skin irritation.
Two AP 2.5 mm drill holes are made 5 mm from the lateral end of the clavicle and 5 mm from the medial end of the acromion. Two No. 6 sutures are passed around the AC joint with an untwist Mayo needle and tied tightly to reduce anteroposterior translation. The cerclage is realized in a figure of 8 configuration that is the more stable construct. As described by Barth et al., the acromion and clavicle are not perfectly aligned with acromioclavicular joint. Consequently, the articular facets that are the most reliable landmark are reduced under direct visualization. The reduction and the acromioclavicular and coracoclavicular cerclages are tied tightly. The deltotrapezial interval is carefully repaired and the wound that measure usually 6 cm is closed in routine fashion.[57]
Arthroscopic Reduction for Acute Dislocation
This subsection does not exist. You can ask for it to be created, but consider checking the search results below to see whether the topic is already covered.
Open Reduction for Chronic Dislocation: Mazzocca Technique and its Variants
Indications
Proper indications are irreducible dislocations or dislocations with severe displacement for patients who complains of persistent pain, muscle fatigue, popping, loss of strength, or scapular dyskinesis after a reasonable period of appropriate physiotherapy, in a supple shoulder. The use of a free tendon graft placed in an anatomic position reproduce the conoid and trapezoid ligaments and perform as the intact coracoclavicular ligament complex.[10][58]
Postoperative Rehabilitation
Immobilization is recommended during six weeks, time needed for the reconstruction to develop biologic stability. Immediate glenohumeral mobility exercises such as internal/external rotation elbow at the side and flexion/extension of the elbow with the arm supported or in the supine position are recommended to avoid potential secondary frozen shoulder. After six weeks, progressive forward elevation is allowed and exercises against resistance are added. Emphasis should be placed on strengthening the scapular stabilizers. Consequently, sports such as brace stroke, nordic walking, elliptic machine and rowing are permitted at six weeks. Overhead sports and heavy labor are not allowed before three to four months postoperative.
Complications
Hardware migration is not anymore a complication as most surgeons to abandon their use. Loss of reduction of the acromioclavicular joint is found in around 30% of the cases. The cause depends of the type of repair. The weight of the arm and scapula places tremendous static forces on the coracoclavicular reconstruction. The quality of the AC reduction comparing a reduced, subluxated (<50%) or dislocated (>50%) joint affected the clinical outcome scores (Constant, DASH) in a statistically significant manner (P < .005), with improved results with a better reduction. Persistent instability explains most of the chronic pain found after reconstruction.[51][52][59] Migration of the fixation device or erosion through the clavicle or the coracoid process from non absorbable materials used to augment the repair not uncommon (Figures).
Osteolysis of the distal clavicle can be observed particularly when the graft or the non absorbable materials goes around the clavicle, creating a complete discontinuity between the medial and lateral clavicle (Figure).
Coracoclavicular calcification are frequent but should not be considered as a complication as they do not influence clinical results. In fact, the calcification maintained reduction and the stability of the reconstruction seems to be enhanced. Similarly, acromioclavicular arthritis is frequently found on both operated and nonoperated sides and do not compromise clinical outcome.[51][60]
References
- ↑ 1.0 1.1 Barth J, Boutsiadis A, Narbona P, et al. The anterior borders of the clavicle and the acromion are not always aligned in the intact acromioclavicular joint: a cadaveric study. J Shoulder Elbow Surg 2017;26:1121-7
- ↑ Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clinics in sports medicine 2003;22:219-37.
- ↑ Boehm TD, Kirschner S, Fischer A, Gohlke F. The relation of the coracoclavicular ligament insertion to the acromioclavicular joint: a cadaver study of relevance to lateral clavicle resection. Acta Orthop Scand 2003;74:718-21.
- ↑ Rios CG, Arciero RA, Mazzocca AD. Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Am J Sports Med 2007;35:811-7.
The acromioclavicular joint has dual innervation from both the suprascapular nerve and the lateral pectoral nerve. - ↑ Miller M, Thompson S. Delee & Drez's Orthopaedic Sports Medicine: Principles and Practice: Elsevier; 2003.
- ↑ 6.0 6.1 Stimec BV, Lädermann A, Wohlwend A, Fasel JH. Medial coracoclavicular ligament revisited: an anatomic study and review of the literature. Arch Orthop Trauma Surg 2012;132:1071-5
- ↑ Moya D, Poitevin LA, Postan D, Azulay GA, Valente S, Giacomelli F, Mamone LA. The medial coracoclavicular ligament: anatomy, biomechanics,and clinical relevance-a research study. JSES Open Access. 2018 Sep 22;2(4):183-189
- ↑ Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am 1972;54:1187-94.
- ↑ Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med 2004;32:1929-36.
- ↑ 10.0 10.1 Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med 2006;34:236-46
- ↑ Fukuda K, Craig EV, An KN, Cofield RH, Chao EY. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am 1986;68:434-40.
- ↑ Abrassart S, Gagey O, Hoffmeyer P. La chape trapézo-deltoïdienne : réalité ou illusion d’optique. Revue de Chirurgie Orthopédique et Réparatrice de l'Appareil Moteur 2007;93:96-7.
- ↑ Lädermann A, Gueorguiev B, Stimec B, Fasel J, Rothstock S, Hoffmeyer P. Acromioclavicular joint reconstruction: a comparative biomechanical study of three techniques. J Shoulder Elbow Surg 2013;22:171-8.
- ↑ Yoo YS, Tsai AG, Ranawat AS, et al. A biomechanical analysis of the native coracoclavicular ligaments and their influence on a new reconstruction using a coracoid tunnel and free tendon graft. Arthroscopy 2010;26:1153-61.
- ↑ Debski RE, Parsons IMt, Woo SL, Fu FH. Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am 2001;83-A:1344-51.
- ↑ Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med 2004;32:1929-36.
- ↑ Mazzocca AD, Spang JT, Rodriguez RR, et al. Biomechanical and radiographic analysis of partial coracoclavicular ligament injuries. Am J Sports Med 2008;36:1397-402.
- ↑ Ludewig PM, Behrens SA, Meyer SM, Spoden SM, Wilson LA. Three-dimensional clavicular motion during arm elevation: reliability and descriptive data. The Journal of orthopaedic and sports physical therapy 2004;34:140-9.
- ↑ 19.0 19.1 Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases). Am J Roentgenol Radium Ther Nucl Med 1971;112:493-506
- ↑ Bosworth BM. Complete acromioclavicular dislocation. N Engl J Med 1949;241:221-5
- ↑ Bearden JM, Hughston JC, Whatley GS. Acromioclavicular dislocation: method of treatment. J Sports Med 1973;1:5-17.
- ↑ Barth J, Boutsiadis A, Narbona P, et al. The anterior borders of the clavicle and the acromion are not always aligned in the intact acromioclavicular joint: a cadaveric study. J Shoulder Elbow Surg 2017;26:1121-7.
- ↑ Gastaud O, Raynier JL, Duparc F, Baverel L, Andrieu K, Tarissi N, Barth J. Reliability of radiographic measurements for acromioclavicular joint separations. Orthop Traumatol Surg Res. 2015 Dec;101(8 Suppl):S291-5.
- ↑ Rahm S, Wieser K, Spross C, Vich M, Gerber C, Meyer DC. Standard axillary radiographs of the shoulder may mimic posterior subluxation of the lateral end of the clavicle. J Orthop Trauma. 2013 Nov;27(11):622-6.
- ↑ Karargyris O, Murphy RJ, Arenas A, Bolliger L, Zumstein MA. Improved identification of unstable acromioclavicular joint injuries in a clinical population using the acromial center line to dorsal clavicle radiographic measurement. J Shoulder Elbow Surg. 2020 Mar 5. pii: S1058-2746(19)30844-4.
- ↑ Plomb-Holmes C, Clavert P, Kolo F, Tay E, Ladermann A, French Society of A. An orthopaedic surgeon's guide to ultrasound imaging of the healthy, pathological and postoperative shoulder. Orthop Traumatol Surg Res. 2018 Dec;104(8S):S219-S232.
- ↑ 27.0 27.1 Plomb-Holmes C, Clavert P, Kolo F, Tay E, Ladermann A, French Society of A. An orthopaedic surgeon's guide to ultrasound imaging of the healthy, pathological and postoperative shoulder. Orthop Traumatol Surg Res. 2018 Dec;104(8S):S219-S232
- ↑ Arrigoni P, Brady PC, Zottarelli L, Barth J, Narbona P, Huberty D, Koo SS, Adams CR, Parten P, Denard PJ, Burkhart SS. Associated lesions requiring additional surgical treatment in grade 3 acromioclavicular joint dislocations. Arthroscopy. 2014 Jan;30(1):6-10
- ↑ Singh B, Gulihar A, Bilagi P, et al. Magnetic resonance imaging scans are not a reliable tool for predicting symptomatic acromioclavicular arthritis. Shoulder Elbow 2018;10:250-4.
- ↑ Bontempo NA, Mazzocca AD. Biomechanics and treatment of acromioclavicular and sternoclavicular joint injuries. Br J Sports Med 2010;44:361-9.
- ↑ Petersson CJ. Degeneration of the acromioclavicular joint. A morphological study. Acta Orthop Scand 1983;54:434-8.
- ↑ Firinu D, Garcia-Larsen V, Manconi PE, Del Giacco SR. SAPHO Syndrome: Current Developments and Approaches to Clinical Treatment. Curr Rheumatol Rep 2016;18:35.
- ↑ Aljuhani F, Tournadre A, Tatar Z, et al. The SAPHO syndrome: a single-center study of 41 adult patients. The Journal of rheumatology 2015;42:329-34.
- ↑ Rukavina I. SAPHO syndrome: a review. Journal of children's orthopaedics 2015;9:19-27.
- ↑ Nevalainen MT, Ciccotti MG, Morrison WB, Zoga AC, Roedl JB. Distal clavicular osteolysis in adults: association with bench pressing intensity. Skeletal Radiol. 2016 Nov;45(11):1473-9
- ↑ Dupas J, Badilon P, Daydé G. Aspects radiologiques d’une ostéolyse essentielle progressive de la main gauche. J Radiol 1936;20:383-7
- ↑ Ehricht HG. [Osteolysis of the lateral clavicular end after compressed air damage]. Archiv fur orthopadische und Unfall-Chirurgie 1959;50:576-82.
- ↑ Gorham LW, Stout AP. Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone); its relation to hemangiomatosis. J Bone Joint Surg Am 1955;37-A:985-1004
- ↑ El-Kouba G, de Araujo Santos R, Pilluski PC, Severo A, Lech O. Gorham-Stout Syndrome: Phantom Bone Disease. Revista brasileira de ortopedia 2010;45:618-22
- ↑ Schwarzkopf R, Ishak C, Elman M, Gelber J, Strauss DN, Jazrawi LM. Distal clavicular osteolysis: a review of the literature. Bull NYU Hosp Jt Dis 2008;66:94-101.
- ↑ Cahill BR. Osteolysis of the distal part of the clavicle in male athletes. J Bone Joint Surg Am 1982;64:1053-8.
- ↑ Mumford E. Acromioclavicular dislocation: a new treatment. J Bone Joint Surg Am 1941;23:799–802.
- ↑ Gurd FB. The Treatment of Complete Dislocation of the Outer End of the Clavicle: An Hitherto Undescribed Operation. Annals of surgery 1941;113:1094-8.
- ↑ Gaillard J, Calo M, Nourissat G. Bipolar Acromioclavicular Joint Resection. Arthrosc Tech 2017;6:e2229-e33.
- ↑ Lädermann A, Christophe FK, Denard PJ, Walch G. Supraspinatus rupture at the musclotendinous junction: an uncommonly recognized phenomenon. J Shoulder Elbow Surg 2012;21:72-6.
- ↑ Bouchard A, Garret J, Favard L, Charles H, Ollat D. Failed subacromial decompression. Risk factors. Orthop Traumatol Surg Res. 2014 Dec;100(8 Suppl):S365-9.
- ↑ Gastaud O, Raynier JL, Duparc F, Baverel L, Andrieu K, Tarissi N, Barth J. Reliability of radiographic measurements for acromioclavicular joint separations. Orthop Traumatol Surg Res. 2015 Dec;101(8 Suppl):S291-5.
- ↑ Gladstone J, Wilk K, Andrews J. Nonoperative treatment of acromioclavicular joint injuries. Oper Tech Sports Med 1997;5:78–87.
- ↑ Cho CH, Hwang I, Seo JS, Choi CH, Ko SH, Park HB, Dan J. Reliability of the classification and treatment of dislocations of the acromioclavicular joint. J Shoulder Elbow Surg. 2014 May;23(5):665-70.
- ↑ Gladstone J, Wilk K, Andrews J. Nonoperative treatment of acromioclavicular joint injuries. Oper Tech Sports Med 1997;5:78–87.
- ↑ 51.0 51.1 51.2 51.3 Lädermann A, Grosclaude M, Lubbeke A, et al. Acromioclavicular and coracoclavicular cerclage reconstruction for acute acromioclavicular joint dislocations. J Shoulder Elbow Surg 2011;20:401-408
- ↑ 52.0 52.1 52.2 Barth J, Duparc F, Andrieu K, et al. Is coracoclavicular stabilisation alone sufficient for the endoscopic treatment of severe acromioclavicular joint dislocation (Rockwood types III, IV, and V)? Orthopaedics & traumatology, surgery & research : OTSR 2015;101:S297-303
- ↑ Scheibel M, Dröschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011 Jul;39(7):1507-16.
- ↑ Sobhy MH. Midterm results of combined acromioclavicular and coracoclavicular reconstruction using nylon tape. Arthroscopy. 2012 Aug;28(8):1050-7
- ↑ Dyrna F, Imhoff FB, Haller B, et al. Primary Stability of an Acromioclavicular Joint Repair Is Affected by the Type of Additional Reconstruction of the Acromioclavicular Capsule. Am J Sports Med 2018:363546518807908.
- ↑ Gowd AK, Liu JN, Cabarcas BC, et al. Current Concepts in the Operative Management of Acromioclavicular Dislocations: A Systematic Review and Meta-analysis of Operative Techniques. Am J Sports Med 2018:363546518795147.
- ↑ Abrassart S, Gagey O, Hoffmeyer P. La chape trapézo-deltoïdienne : réalité ou illusion d’optique. Revue de Chirurgie Orthopédique et Réparatrice de l'Appareil Moteur 2007;93:96-7
- ↑ Boutsiadis A, Baverel L, Lenoir H, Delsol P, Barth J. Arthroscopic-assisted Acromioclavicular and Coracoclavicular Ligaments Reconstruction for Chronic Acromioclavicular Dislocations: Surgical Technique. Tech Hand Up Extrem Surg. 2016 Dec;20(4):172-178.
- ↑ Mayr E, Braun W, Eber W, Ruter A. [Treatment of acromioclavicular joint separations. Central Kirschner- wire and PDS-augmentation]. Der Unfallchirurg 1999;102:278-86.
- ↑ Hessmann M, Gotzen L, Gehling H. Acromioclavicular reconstruction augmented with polydioxanonsulphate bands. Surgical technique and results. Am J Sports Med 1995;23:552-6.