Difference between revisions of "Shoulder:Developmental Anatomy of the Shoulder and Anatomy of the Glenohumeral Joint"
| Line 17: | Line 17: | ||
===Anatomy=== | ===Anatomy=== | ||
| − | The acromion is normally formed by the fusion of several ossification | + | The acromion is normally formed by the fusion of several ossification centers.<ref>Prescher A. Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. Eur J Radiol, 2000, 35: 88– 10210</ref> Macalister<ref>Macalister A. Notes on acromion. J Anat Physiol, 1893, 27: 244.1– 244.251</ref> found that several ossification points fuse to form three major elements. The anterior element is the preacromion, the middle element is the mesacromion, and the posterior element, which forms the acromial angle, is the metacromion. These three elements merge to form a triangular epiphyseal bone, which finally fuses with the basiacromion. The basiacromion typically fuses with the scapular spine by age 12, and all four centers should unite by ages 15 to 18. However, some do not have complete ossification until as late as age 25 years,<ref>McClure JG, Raney RB. Anomalies of the scapula. Clin Orthop Relat Res, 1975, 110: 22– 31</ref> leading to an inhomogeneous group of variations known as “os acromiale.” Thus, any diagnosis of such deformity should not be defined until after this time point.<ref>Johnston PS, Paxton ES, Gordon V, Kraeutler MJ, Abboud JA, Williams GR. Os acromiale: a review and an introduction of a new surgical technique for management. Orthop Clin North Am, 2013, 44: 635– 644</ref> The types of os acromiale are determined according to the unfused segment immediately anterior to the site of nonunion,<ref name=":0">Boehm TD, Matzer M, Brazda D, Gohlke FE. Os acromiale associated with tear of the rotator cuff treated operatively. J Bone Joint Surg Br, 2003, 85: 545– 549</ref><ref>Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic os acromiale. J Am Acad Orthop Surg, 2006, 14: 12– 19</ref> which contains the meta-acromion (base), the meso-acromion (mid), and the pre-acromion (tip) from proximally to distally (Figure).<ref name=":0" /> |
| − | |||
| − | |||
| − | |||
| − | |||
===Morbidity=== | ===Morbidity=== | ||
Revision as of 06:44, 29 July 2021
Contents
- 1 Bullet Points
- 2 Key words
- 3 Os Acromiale
- 4 What would Codman have thought about this?
- 4.1 The anatomy of the human shoulder
- 4.1.1 The sterno-clavicular joint
- 4.1.2 The acromio-clavicular joint
- 4.1.3 The coracoid process
- 4.1.4 The acromion process
- 4.1.5 The spine of the scapula
- 4.1.6 The glenoid
- 4.1.7 The blade
- 4.1.8 The clavicle
- 4.1.9 The ligaments
- 4.1.10 The coraco-acromial ligament
- 4.1.11 The muscles
- 4.1.12 The short rotators
- 4.1.13 The musculo-tendinous cuff
- 4.1.14 The sulcus and anatomic neck
- 4.1.15 Bursa about the shoulder
- 4.1 The anatomy of the human shoulder
- 5 References
Bullet Points
- Os acromiale is a developmental defect which results from the lack of an osseous union between the ossification centers of the acromion, leading to the fibrocartilaginous tissue connection.
- The prevalence of os acromiale is 1% to 15%, and is quite common in the African American population.
- Nonoperative therapy for symptomatic os acromiale should be started, including physiotherapy, nonsteroidal anti-inflammatory drugs, and injections.
- Surgical treatment is indicated after failed conservative treatment. In symptomatic patients with fixable acromiale.
Key words
Os Acromiale
Reproduced from You et a.,[1] with permission
Introduction
Os acromiale represents an unfused accessory center of ossification of the acromion of the scapula. It is regarded as one of the reasons for rotator cuff tears and shoulder impingement.[2][3] which is generally asymptomatic and discovered accidentally. This anatomic deformity occurs more frequently in persons of Black ancestry than in persons of White, Native American and Middle Eastern ancestries.[4] Treatment for symptomatic patients is primarily non-operative, like nonsteroidal anti-inflammatory drug, physical therapy or corticosteroid injection. Surgical procedures are typically recommended only after non-operative treatments have failed. Common procedures include arthroscopic subacromial decompression with acromioplasty,[5] open or arthroscopically assisted reduction and internal fixation with or without bone grafting,[6][7] and open or arthroscopic excision of the os fragment.[8]
Anatomy
The acromion is normally formed by the fusion of several ossification centers.[9] Macalister[10] found that several ossification points fuse to form three major elements. The anterior element is the preacromion, the middle element is the mesacromion, and the posterior element, which forms the acromial angle, is the metacromion. These three elements merge to form a triangular epiphyseal bone, which finally fuses with the basiacromion. The basiacromion typically fuses with the scapular spine by age 12, and all four centers should unite by ages 15 to 18. However, some do not have complete ossification until as late as age 25 years,[11] leading to an inhomogeneous group of variations known as “os acromiale.” Thus, any diagnosis of such deformity should not be defined until after this time point.[12] The types of os acromiale are determined according to the unfused segment immediately anterior to the site of nonunion,[13][14] which contains the meta-acromion (base), the meso-acromion (mid), and the pre-acromion (tip) from proximally to distally (Figure).[13]
Morbidity
The frequency of os acromiale has ranged from 1 to 15% in radiographic and anatomical studies9, 11, 16-18. Case et al.19 compared a South African cadaver sample (n = 494) with a medieval Danish archaeological sample (n = 532). The results showed that the South African frequency (18.2%) was significantly higher than the medieval Danish frequency (7.7%, P < 0.0001, and a left side bias (72%) among the South Africans (P = 0.013). However, sex and age biases were not found. Kumar et al.20 reviewed the X-rays and MRI of Korean patients visiting a shoulder clinic, and found that 13 cases out of 1568 patients had an os acromiale; there were 5 and 8 cases of pre-acromiale and meso-acromiale, respectively. Thus, the prevalence of os acromiale in this study population was found to be 0.7 (7 cases per 1000 patients), which is much lower than for Black and White people, comparing with other studies. At the same time, gender and hand dominance was not associated with frequency of os acromiale. A systematic review and meta-analysis of 23 studies revealed a significantly higher frequency in persons of Black ancestry than in persons of White, Native American, and Middle Eastern ancestries, and significantly higher unilateral and bilateral frequencies in those with Black ancestry; there were no significant interactions of Os acromiale frequency with gender and side5.
Os Acromiale with Rotator Cuff Tear
Some previous studies have demonstrated a high incidence of full thickness rotator cuff tears in os acromiale patients (approximately 50%)21, 22. However, due to the small samples of the former papers, 15 and 6 shoulders, respectively, the latter studies re-examine the relationship between rotator cuff tear and os acromiale. Boehm et al.23 assessed operation notes and axillary radiographs for the presence and the type of os acromiale in 1000 consecutive patients with open rotator cuff repairs. Only 62 patients (6.2%) revealed an os acromiale in the axillary radiographs, and the average number of tendons involved in the cuff tear was the same (1.4) in patients with and without os acromiale; the average age of patients with and without os acromiale was 55 and 56 years, respectively. This result was similar to the 8% general incidence of os acromiale reported by Yammine5. Ouellette et al.24 retrospectively analyzed 84 MRI studies of the shoulder, which revealed that the presence of os acromiale may not significantly predispose to supraspinatus and infraspinatus tendon tears. However, subjects with step-off deformity (Fig. 2)24 of an os acromiale are at greater risk of rotator cuff tears than are similar subjects without such deformity. In young throwing athletes, Roedl et al.25 found that rotator cuff tears were significantly more common on the follow-up MRI in patients with acromial apophysiolysis (68%, 15 of 22) compared with control patients (29%, 6 of 21; P = 0.015, Fisher exact test; OR = 5.4). In addition, grades of rotator cuff tears were significantly higher in patients with acromial apophysiolysis compared with control patients (P = 0.03).
(A) Os acromiale without step-off deformity. T1-weighted sagittal MRI of the shoulder shows an os acromiale without step-off deformity (arrow) relative to the inferior cortex of the acromion. A, acromion; H, humeral head; O, os acromiale; P, posterior. (B) Os acromiale with step-off deformity. T1-weighted sagittal MRI of the shoulder shows malalignment (white arrowhead) between the inferior cortex of the os acromiale (arrow) and the acromion. A, acromion; C, clavicle; P, posterior24.
In general, the most common os acromiale is the large, relatively triangular mesoacromion, which forms an interface with the acromion in proximity to the acromioclavicular joint (ACJ), while a less common os acromiale, the preacromion, is noted at the distal tip of the acromion26. There is a strong relationship between os acromiale and race, while the correlation between os acromiale and rotator cuff tear is full of controversies.
Symptoms and Diagnosis
Os acromiale can be easily diagnosed with plain X-rays with at least two views (AP, axillary views). As mentioned above, the frequency of os acromiale has ranged from 1 to 18.2% in radiographic and anatomical studies. If these figures are correct, clearly, most of patients with os acromial are asymptomatic.
Symptoms
Patients with symptomatic os acromiale, especially in young people and athletes with overhead activity, may have pain at the superior aspect of the shoulder25, 27. Symptoms can also occur at night. Along with pain, patients may have decreased shoulder motion and strength. Patients will be tender to palpation at the site of the os acromiale and there may also be obvious movement of the bone.
Imaging Diagnosis
Although the os acromiale usually can be seen on an axillary lateral radiograph (Fig. 3)28, it can be obscured by the proximal part of the humerus and be missed, in which case the double-density sign becomes a very important and typical indication in the anteroposterior view of the shoulder (Fig. 4)28. In addition, ultrasound is a quick and accurate method. In Boehm et al.29, the os acromiale could be identified in all 25 patients (100%) with radiologically confirmed os acromiale. In 12 patients, an os acromiale could be identified on the contralateral side (48%). The average width of the non-ossified space was 4.3 mm (2.5 to 7.6 mm). Three different sonographic types of bony margins of the os acromiale and the acromion exist: Type I with flat bony margins; Type II with marginal osteophytes and Type III with inverted bony margins. The authors concluded that ultrasound could give additional information about the os acromiale if radiological assessment is unclear because of superimposing bones.
Axillary lateral radiograph demonstrating a meso-acromion (arrow).
(A) Anteroposterior radiograph demonstrating the double-density sign, with the cortical margin of a meso-acromion (OS) superimposed over the cortical margin of the base of the acromion (Ac) at the nonunion site. The margins of this os acromiale appear smooth, sharp, and well circumscribed. DC, distal part of the clavicle. (B) Diagrammatic representation of the radiograph.
The radiologic diagnosis of os acromiale remains challenging in young patients. In an adolescent patient presenting with a painful shoulder, it may be difficult to distinguish a normally developing acromion with a secondary ossification center from the early formation of an os acromiale on the basis of age alone. Therefore, MRI and SPECT–CT are receiving more and more attention26, 30-32. Winfeld et al.33 demonstrated that the unique morphologic and signal intensity characteristics of the interface between the native acromion and unfused ossification center strongly assist the ability to diagnose an os acromiale on MRI, because MRI can not only show the abnormal shape but also display the marrow edema along the opposing surfaces (Fig. 5)33. In the correct clinical context, a shoulder MRI of an adolescent with imaging findings consistent with os acromiale should be reported, as this may, in fact, be a sign of ossicle instability and the potential source of symptoms as well as the target of treatment strategies. Recently, Al-faham reported on an 18-year-old male American football player who presented with persistent left shoulder pain without positive findings on X-rays or MRI. SPECT/CT with 99mTc-MDP Bone Scintigraphy was performed for further anatomic localization with the field of view restricted to the shoulders. The images demonstrated incomplete fusion of both acromion processes, which could be age-related in this patient. However, the ossification center in the left apophysis occurred at the mesoacromion rather than at the preacromion (as on the right side) and was associated with more activity (Fig. 6)34, indicating ongoing osteoblastic activity likely from incomplete fusion. This finding was consistent with pain and the youth was diagnosed as having os acromiale.
Axial proton density-weighted fat-saturated image of the left shoulder of a 17-year-old boy demonstrates an ununited ossicle adjacent to the acromion suggestive of os acromiale. There is a fluid-like signal at the interface (arrow) and marrow edema along the opposing surfaces (curved arrows) of the distal acromial ossification center (asterisk) and the rest of the acromion33.
Top row shows static bone scan and blood-pool images, middle row images shows fused SPECT/CT images, and bottom row shows attenuation correction CT. Arrows are placed at ossification centers of apophyses. Center is at meso-acromion on the left (white arrow) but at preacromion on the right (black arrow). The right apophysis is nearly fused and has less activity than the unfused apophysis of the left acromion.
Treatment
Nonsurgical management: Most cases of os acromiale are asymptomatic and, thus, require no specific treatment35. Primary management of symptomatic os acromiale should be nonsurgical. Nonsteroidal anti-inflammatory drugs, in conjunction with physiotherapy, are prescribed for a typical impingement treatment protocol. Subacromial and nonunion site corticosteroid injection also may be used to relieve symptoms13. Usually, conservative treatment should be tried for at least 6 months15.
Once all conservative means have failed, surgical treatment should be considered. Numerous surgical procedures have been introduced, including open or arthroscopic excision of the os fragment, open reduction-internal fixation with or without bone grafting, arthroscopic subacromial decompression with acromioplasty, and arthroscopically assisted reduction–internal fixation. Depending on the individual situation, various techniques have different indications. Basically, surgical techniques should focus on the os acromiale itself when the non-healing site is unstable and painful only; however, the concomitant pathology, including rotator cuff tears or shoulder impingement, need to be solved together in some cases.
Open/Arthroscopic Assisted Reduction and Internal Fixation
As to the unstable and painful os acromiale, internal fixation can fix the fragment and relieve the pain from the pulling of deltoid; therefore, its primacy and significance are widely recognized9, 21, 36-40. Fusion is sometimes difficult to accomplish, so some surgeons9, 36, 38, 40 prefer to use a transacromial approach to preserve the terminal branches of the thoracoacromial artery (Fig. 7)36; furthermore, some doctors tend to use local bone graft or iliac crest bone graft to improve the fusion39, 41. During the operation, there are two key points which need to be considered. First, the sclerotic edges of the pseudarthrosis should be excised with marginal dorsal wedge cuts by use of a microsaw while preserving as much bone as possible; then the anterior portion of the acromion is fixed in a tilted upward position with a large subacromial space, which makes the acromioplasty non-essential21, 38. Second, although the K-wire and tension band provide stable fixation and good outcomes, nonunion and hardware discomfort are not uncommon. For these reasons, cannulated screws and the tension band technique was recommended42. In addition, it is reported that polyethylene sutures and stainless steel wire have similar biomechanical strength in the cannulated screw tension band fixation, which may prevent soft-tissue problems35.
(A) Deltoid-off approach: Terminal branches of thoracoacromial artery have been divided. Hence, unfused acromial epiphysis is devascularized. (B) Transacromial approach. Terminal branches of thoracoacromial artery remain intact. Acromial epiphysis remains vital and maintains full healing potential.
In addition to these open surgeries, the arthroscopic technique is intended to preserve the blood supply to the os acromiale, to minimize deltoid muscle injury by avoiding its detachment, to improve the cosmetic results, and to preclude the need for hardware removal. Atoun et al.8 pointed out one arthroscopically-assisted internal fixation with absorbable screws (Fig. 8)8 provided promising clinical, cosmetic, and radiologic results with high patient satisfaction. The arthroscope is introduced to the subacromial space through the same skin incision, and an evaluation of the bursal side of the rotator cuff, acromion, and os acromiale is performed. A shaver blade is introduced through a standard lateral portal (4 to 5-cm lateral to the lateral edge of the acromion at the line of the anterior distal clavicle) and used to expose the os acromiale by removing the inferior soft tissues. After full assessment and debridement of the nonunion site, two biodegradable 4.5-mm screws (Inion, Tampere, Finland) are used to achieve a good compression of the mesoacromion and meta-acromion fragments. However, the biomechanical strength of biodegradable screws requires further research, and it is difficult to make a marginal dorsal wedge excision and fix the acromion at a tilted upward position, which means subacromial decompression is hard to avoid.
(A) Schematic drawing shows compression of the acromion and the os acromiale fragment. (B) Arthroscopic view shows compression of the acromion and the os acromiale fragment.
Open/Arthroscopic Resection of Os Acromiale
It is generally recommended that small acromial fragments should be excised, and that large ones should be fused9. However, the outcomes of open excision do not seem very satisfactory owing to the postoperative weakness and dysfunction of deltoid. Mudge et al.43 had eight rotator cuff tears associated with os acromiale. Six underwent fragment excision and rotator cuff repair, including suturing of the deltoid to the acromion. Four of them had excellent results postoperatively, while the remaining two had poor results. Warner et al.21 demonstrated a good outcome in one pre-acromion excision and poor outcomes in two meso-acromion excisions with lingering weakness and pain. Boehm et al.14 used an anterior approach releasing deltoid in all 33 patients and reconstructed the rotator cuff before treatment of the os acromiale. After repair of the cuff, the authors used one of three surgical procedures to treat the os acromiale, including excision, acromioplasty, and fusion. The constant scores were 82, 81, 81, and 84% for patients who had excision, acromioplasty, successful fusion and unsuccessful fusion, respectively. There were no statistically significant differences. The study concluded that a small mobile os acromiale can be resected, a large stable os acromiale treated by acromioplasty, and a large unstable os acromiale treated by fusion to the acromion. Even without radiological fusion, the clinical outcome can be good.
Arthroscopic excision has the possible benefit of less periosteal and deltoid attachment injury, potentially lending to better results than open excision44. Campbell et al.45 demonstrated no decrease in deltoid function or strength compared with the contralateral arm and found no difference in results when the excision was performed with or without a rotator cuff repair. In addition, Kawaguchi et al.46 reported a case of impingement syndrome of the left shoulder secondary to unstable meso-acromiale, which accepted the arthroscopic excision of the unstable fragment and was successful without residual dysfunction of the deltoid muscle.
Os Acromiale Combined with Shoulder Impingement or Rotator Cuff Tear
Although the surgical management of simple os acromiale and its results have been accepted, the ideal treatment for os acromiale-related diseases is remains controversial. In some studies, os acromiale with shoulder impingement or rototar cuff tear has been described as a depressing event. Hutchinson and Veenstra47 discussed the unsatisfactory results for three patients who underwent routine arthroscopic subacromial decompression. All the patients initially had a good outcome (in the first few months). However, the three patients experienced a return of their preoperative symptoms 1 year postoperatively and two of them underwent repeat surgery. Hence, the study concluded that arthroscopic subacromial decompression is probably not a solution for impingement syndrome secondary to os acromiale. Abboud et al.48 treated eight patients (os acromiale associated with rotator cuff tears) with open reduction-internal fixation and open rotator cuff repair. Although all the os fragments achieved union, only three (37.5%) obtained a satisfactory result. The authors inferred that the poor results may be related to the hardware-sourced pain even after the nonunion healed, as well as the bias in population in part (47% were involved in workers’ compensation claims). In contrast, Wright et al.49 presented an extended arthroscopic subacromial decompression. The goal of the modified arthroscopic acromioplasty was resection of adequate bone to remove the mobile anterior acromial tip. In general, this consisted of more bony resection than for the typical arthroscopic acromioplasty. All patients achieved full strength of the anterior deltoid and rotator cuff muscles by 6 months postoperatively as evaluated by manual muscle testing. At the final follow-up (average 29 months, range from 20 to 72 months), 12 of the 13 shoulders were rated by the patients as having a satisfactory result. The study reminds us the os acromiale may not affect the strength of anterior deltoid obviously. Walch et al.50 demonstrated that preoperative acromial lesions such as os acromiale are not a contraindication to reverse shoulder arthroplasty (RSA). These patients can also acquire a good postoperative range of motion, Constant score, or subjective results compared to normal acromial patients, even without osteosynthesis of the free fragment when performing RSA. One of the possible reasons in the study was that the main part of the deltoid was still attached firmly to the spine of the scapula and clavicle and was obviously strong enough to compensate for the middle part. In the same way, Aibinder et al.51 observed that RSA did not seem to be negatively affected by the presence of an os acromiale. Inferior tilting of the unfused segment is observed in approximately one-third of the shoulders after RSA and does not seem to change the overall outcome of the procedure. This means that even if the RSA requires particularly good function of the deltoid, healing and stability of the os acromiale are not necessary.
The Relationship between Os Acromiale and Acromioclavicular Joint
In addition to the deltoid, the articulation of os acromiale with the lateral end of the clavicle is another area of interest. Based on the review, there is only one published paper in the English literature: it investigated 211 volunteers (control group) and 33 subjects without or with os acromiale52. Half of the acromions of the control group (52.1%) had the articular facet of the acromioclavicular joint (ACJ) on the acromion tip, whereas in 45.4% the facet tip was located distally. In contrast, of 33 subjects with os acromiale, 18.1 and 81.1%, respectively, had the AC joint lying on or distal to the acromion tip. The author suggested that the greater the distance of the AC joint from the anterior edge of the acromion, the higher the likelihood of an os acromiale. In other words, the AC joint position was responsible for a higher predisposition to os acromiale. Because of the limited samples and lack of post and successive studies, the real cause-and-effect relationship between os acromiale and AC joint is still not clear. Another possible explanation is that the os acromiale affects the development of ACJ. The instability resulting from os acromiale may produce the chronic dislocation of ACJ to the posterior side, which could answer why the frequency of the mesoacromion is higher than that of the preacromion. There is no published data evaluating the association of os acromiale with degenerative change of ACJ and there is no published study assessing the stability of os acromiale following resection of lateral end clavicle for OA of ACJ. Clearly, more studies need to be done in the future.
Complications
As previously mentioned, hardware-sourced problems were often occurred after tension band fixation. Depending on the fixation technique, the incidence of nonunion after internal fixation was from 0% to 100%37. In addition, Boehm et al.14 showed the postoperative infection rate with two superficial infections (6%) and four deep infections (13%). One of the deep infection cases was following ORIF (5%, 1/22), one case was following open excision (17%, 1/6), and two cases were following open acromioplasty (40%, 2/5) as well. Two cases of superficial infection followed ORIF (9%, 2/22).
Conclusion
Os acromiale is not a rare finding in patients with painful shoulders and the meso-acromion type is found in clinic most frequently. There is a strong relationship between os acromiale and race, except for Korean patients, while the correlation between os acromiale and rotator cuff tears is controversial. Os acromiale in adults is easily diagnosed by X-ray, particularly on the axillary view; however, the differential diagnosis of adolescents may require MRI or SPECT–CT. Generally, nonoperative therapy for symptomatic os acromiale should be commenced, including physiotherapy, and administration of nonsteroidal anti-inflammatory drugs and injections. Surgical treatment is indicated after failed conservative treatment. In symptomatic patients with fixable os acromiale, the tension band technique should be used so that the anterior aspect of the acromion is elevated from the humerus head. In patients with small fragments which are unsuitable for reattachment, excision might be the best therapeutic option and can lead to good outcomes. Whether internal fixation or resection, the arthroscopic technique results in a better outcome and fewer complications, especially in older patients or athletes with overhead movement, because of the high incidence of shoulder impingement or rotatar cuff tears which can be treated concurrently. In reviewing the literature, it is found that extended arthroscopic subacromial decompression, successful rotator cuff repair, and RSA could also achieve a good result in subacromial impingement, rotator cuff tear, or end-stage cuff tear arthropathy, respectively, even without osteosynthesis of the os acromiale. In the future, a prospective study is necessary to answer this question of whether the os acromiale is related to those patients with high incidence of subacromial impingement or rotator cuff tears.
1Buss DD, Freehill MQ, Marra G. Typical and atypical shoulder impingement syndrome: diagnosis, treatment, and pitfalls. Instr Course Lect, 2009, 58: 447– 457. PubMed Google Scholar 2Maffulli N, Longo UG, Berton A, Loppini M, Denaro V. Biological factors in the pathogenesis of rotator cuff tears. Sports Med Arthrosc Rev, 2011, 19: 194– 201. Crossref PubMed Web of Science®Google Scholar 3Acar B, Kose O. Shoulder pain after falling from bicycle. Turk J Emerg Med, 2016, 16: 91– 92. Crossref PubMed Web of Science®Google Scholar 4Familiari F, Huri G, Gonzalez-Zapata A, McFarland EG. Scapula fracture and os acromiale after reverse total shoulder arthroplasty. Orthopedics, 2014, 37: 434, 492–495. PubMed Web of Science®Google Scholar 5Yammine K. The prevalence of os acromiale: a systematic review and meta-analysis. Clin Anat, 2014, 27: 610– 621. Wiley Online Library CAS PubMed Web of Science®Google Scholar 6Harris JD, Griesser MJ, Jones GL. Systematic review of the surgical treatment for symptomatic os acromiale. Int J Shoulder Surg, 2011, 5: 9– 16. Crossref PubMed Web of Science®Google Scholar 7Sahajpal D, Strauss EJ, Ishak C, Keyes JM, Joseph G, Jazrawi LM. Surgical management of os acromiale: a case report and review of the literature. Bull NYU Hosp Jt Dis, 2007, 65: 312– 316. PubMed Google Scholar 8Atoun E, Van Tongel A, Narvani A, Rath E, Sforza G, Levy O. Arthroscopically assisted internal fixation of the symptomatic unstable os acromiale with absorbable screws. J Shoulder Elbow Surg, 2012, 21: 1740– 1745. Crossref PubMed Web of Science®Google Scholar 9Edelson JG, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg Br, 1993, 75: 551– 555. Crossref CAS PubMed Web of Science®Google Scholar 10Prescher A. Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. Eur J Radiol, 2000, 35: 88– 102. Crossref CAS PubMed Web of Science®Google Scholar 11Macalister A. Notes on acromion. J Anat Physiol, 1893, 27: 244.1– 244.251. CAS PubMed Google Scholar 12McClure JG, Raney RB. Anomalies of the scapula. Clin Orthop Relat Res, 1975, 110: 22– 31. Crossref PubMed Web of Science®Google Scholar 13Johnston PS, Paxton ES, Gordon V, Kraeutler MJ, Abboud JA, Williams GR. Os acromiale: a review and an introduction of a new surgical technique for management. Orthop Clin North Am, 2013, 44: 635– 644. Crossref PubMed Web of Science®Google Scholar 14Boehm TD, Matzer M, Brazda D, Gohlke FE. Os acromiale associated with tear of the rotator cuff treated operatively. J Bone Joint Surg Br, 2003, 85: 545– 549. Crossref CAS PubMed Web of Science®Google Scholar 15Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic os acromiale. J Am Acad Orthop Surg, 2006, 14: 12– 19. Crossref PubMed Web of Science®Google Scholar 16Liberson F. Os acromiale: a contested anomaly. J Bone Joint Surg Am, 1937, 19: 683– 689. Google Scholar 17Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg, 1996, 5: 1– 11. Crossref CAS PubMed Google Scholar 18Sammarco VJ. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am, 2000, 82: 394– 400. Crossref CAS PubMed Web of Science®Google Scholar 19Case DT, Burnett SE, Nielsen T. Os acromiale: population differences and their etiological significance. Homo, 2006, 57: 1– 18. Crossref CAS PubMed Web of Science®Google Scholar 20Kumar J, Park WH, Kim SH, Lee HI, Yoo JC. The prevalence of os acromiale in Korean patients visiting shoulder clinic. Clin Orthop Surg, 2013, 5: 202– 208. Crossref CAS PubMed Google Scholar 21Warner JJ, Beim GM, Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg Am, 1998, 80: 1320– 1326. Crossref CAS PubMed Web of Science®Google Scholar 22Satterlee CC. Successful osteosynthesis of an unstable mesoacromion in 6 shoulders: a new technique. J Shoulder Elbow Surg, 1999, 8: 125– 129. Crossref CAS PubMed Web of Science®Google Scholar 23Boehm TD, Rolf O, Martetschlaeger F, Kenn W, Gohlke F. Rotator cuff tears associated with os acromiale. Acta Orthop, 2005, 76: 241– 244. Crossref PubMed Web of Science®Google Scholar 24Ouellette H, Thomas BJ, Kassarjian A, et al. Re-examining the association of os acromiale with supraspinatus and infraspinatus tears. Skeletal Radiol, 2007, 36: 835– 839. Crossref CAS PubMed Web of Science®Google Scholar 25Roedl JB, Morrison WB, Ciccotti MG, Zoga AC. Acromial apophysiolysis: superior shoulder pain and acromial nonfusion in the young throwing athlete. Radiology, 2015, 274: 201– 209. Crossref PubMed Web of Science®Google Scholar 26Zember JS, Rosenberg ZS, Kwong S, Kothary SP, Bedoya MA. Normal skeletal maturation and imaging pitfalls in the pediatric shoulder. Radiographics, 2015, 35: 1108– 1122. Crossref PubMed Web of Science®Google Scholar 27Frizziero A, Benedetti MG, Creta D, Moio A, Galletti S, Maffulli N. Painful os acromiale: conservative management in a young swimmer athlete. J Sports Sci Med, 2012, 11: 352– 356. PubMed Web of Science®Google Scholar 28Lee DH, Lee KH, Lopez-Ben R, Bradley EL. The double-density sign: a radiographic finding suggestive of an os acromiale. J Bone Joint Surg Am, 2004, 86: 2666– 2670. Crossref PubMed Web of Science®Google Scholar 29Boehm TD, Kenn W, Matzer M, Gohlke F. Ultrasonographic appearance of os acromiale. Ultraschall Med, 2003, 24: 180– 183. Crossref CAS PubMed Web of Science®Google Scholar 30Rovesta C, Marongiu MC, Corradini A, Torricelli P, Ligabue G. Os acromiale: frequency and a review of 726 shoulder MRI. Musculoskelet Surg, 2017, 101: 201– 205. Crossref CAS PubMed Google Scholar 31Tawfik AM, El-Morsy A, Badran MA. Rotator cuff disorders: how to write a surgically relevant magnetic resonance imaging report? World J Radiol, 2014, 6: 274– 283. Crossref PubMed Google Scholar 32Usmani S, Marafi F, Esmail A, Ahmed N. Initial experience with 18F-sodium fluoride (NaF) PET-CT: a viable functional biomarker in symptomatic Os acromiale. Br J Radiol, 2018, 91: 20170741. Crossref PubMed Web of Science®Google Scholar 33Winfeld M, Rosenberg ZS, Wang A, Bencardino J. Differentiating os acromiale from normally developing acromial ossification centers using magnetic resonance imaging. Skeletal Radiol, 2015, 44: 667– 672. Crossref PubMed Web of Science®Google Scholar 34Al-faham Z, Jolepalem P. Use of SPECT/CT with 99mTc-MDP bone scintigraphy to diagnose symptomatic os acromiale. J Nucl Med Technol, 2015, 43: 236– 237. Crossref PubMed Web of Science®Google Scholar 35Shiu B, Song X, Iacangelo A, et al. Os acromiale fixation: a biomechanical comparison of polyethylene suture versus stainless steel wire tension band. J Shoulder Elbow Surg, 2016, 25: 2034– 2039. Crossref PubMed Web of Science®Google Scholar 36Hertel R, Windisch W, Schuster A, Ballmer FT. Transacromial approach to obtain fusion of unstable os acromiale. J Shoulder Elbow Surg, 1998, 7: 606– 609. Crossref CAS PubMed Web of Science®Google Scholar 37Ryu RK, Fan RS, Dunbar WH. The treatment of symptomatic os acromiale. Orthopedics, 1999, 22: 325– 328. CAS PubMed Web of Science®Google Scholar 38Peckett WR, Gunther SB, Harper GD, Hughes JS, Sonnabend DH. Internal fixation of symptomatic os acromiale: a series of twenty-six cases. J Shoulder Elbow Surg, 2004, 13: 381– 385. Crossref PubMed Web of Science®Google Scholar 39Barbier O, Block D, Dezaly C, Sirveaux F, Mole D. Os acromiale, a cause of shoulder pain, not to be overlooked. Orthop Traumatol Surg Res, 2013, 99: 465– 472. Crossref CAS PubMed Web of Science®Google Scholar 40Lebus GF, Fritz EM, Hussain ZB, Pogorzelski J, Millett PJ. Operative treatment of symptomatic Meso-type Os Acromiale. Arthrosc Tech, 2017, 6: e1093– e1099. Crossref PubMed Web of Science®Google Scholar 41Atinga M, Gregor R, Selvaraj KM, Hong TF. Os acromiale open reduction and internal fixation: a review of iliac crest autogenous bone grafting and local bone grafting. J Shoulder Elbow Surg, 2018, 27: 1030– 1036. Crossref PubMed Web of Science®Google Scholar 42Spiegl UJ, Smith SD, Todd JN, Wijdicks CA, Millett PJ. Biomechanical evaluation of internal fixation techniques for unstable meso-type os acromiale. J Shoulder Elbow Surg, 2015, 24: 520– 526. Crossref PubMed Web of Science®Google Scholar 43Mudge MK, Wood VE, Frykman GK. Rotator cuff tears associated with os acromiale. J Bone Joint Surg Am, 1984, 66: 427– 429. Crossref CAS PubMed Web of Science®Google Scholar 44Stetson WB, McIntyre JA, Mazza GR. Arthroscopic excision of a symptomatic Meso-acromiale. Arthrosc Tech, 2017, 6: e189– e194. Crossref PubMed Web of Science®Google Scholar 45Campbell PT, Nizlan NM, Skirving AP. Arthroscopic excision of os acromiale: effects on deltoid function and strength. Orthopedics, 2012, 35: e1601– e1605. Crossref PubMed Web of Science®Google Scholar 46Kawaguchi S, Fukuta S, Tsutsui T, et al. Arthroscopic excision of unstable os acromiale associated with impingement syndrome: a case report. J Med Invest, 2016, 63: 131– 134. Crossref PubMed Web of Science®Google Scholar 47Hutchinson MR, Veenstra MA. Arthroscopic decompression of shoulder impingement secondary to os acromiale. Art Ther, 1993, 9: 28– 32. CAS Google Scholar 48Abboud JA, Silverberg D, Pepe M, et al. Surgical treatment of os acromiale with and without associated rotator cuff tears. J Shoulder Elbow Surg, 2006, 15: 265– 270. Crossref PubMed Web of Science®Google Scholar 49Wright RW, Heller MA, Quick DC, Buss DD. Arthroscopic decompression for impingement syndrome secondary to an unstable os acromiale. Art Ther, 2000, 16: 595– 599. CAS Google Scholar 50Walch G, Mottier F, Wall B, Boileau P, Molé D, Favard L. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg, 2009, 18: 495– 502. Crossref PubMed Web of Science®Google Scholar 51Aibinder WR, Schoch BS, Cofield RH, Sperling JW, Sánchez-Sotelo J. Reverse shoulder arthroplasty in patients with os acromiale. J Shoulder Elbow Surg, 2017, 26: 1598– 1602. Crossref PubMed Web of Science®Google Scholar 52Gumina S, De Santis P, Salvatore M, Postacchini F. Relationship between os acromiale and acromioclavicular joint anatomic position. J Shoulder Elbow Surg, 2003, 12: 6– 8. Crossref PubMed Web of Science®Google Scholar
What would Codman have thought about this?
The anatomy of the human shoulder
It would be very convenient for the reader if all that Gray has to say about the structures composing the shoulder could be reprinted here for ready reference. It is not necessary to specify which Gray or even to state the title of his book, although I may note that the date of my own copy is 1887. This young man, for he died when he was only thirty-five, bequeathed a real legacy to almost every English-speaking doctor who has studied medicine since his time. A doctor may throw away his Bible, but he always keeps his Gray. In spite of the convenience it would be to have the standard facts of anatomy at hand, most purchasers of this book would probably prefer to have it published at less expense and to let them refer when necessary to the "Gray's" which they themselves have already thumb-marked. Yet I know that when I read about a subject in which I am only half interested, I do not bother to use reference books as I should, and probably do the author an injustice by not being sure of the fundamental facts which he assumes I know, but which I have in truth forgotten.
The other extreme would be to assume that every doctor who may read this book already knows the standard anatomic structures of the shoulder, so that the whole chapter could be omitted. This alternative cannot be accepted because it is highly probable that even the graduating classes of the best medical schools could hardly qualify in this respect. Later, as year by year passes after graduation, our anatomic memories are crowded out by other more vital ones, so that it is very unlikely that half the fund of knowledge acquired by early anatomic instruction persists a decade. After two decades of practice, any surgeon will admit that he has forgotten such matters as the branches of the brachial plexus or the origin and insertion of the levator anguli scapulae. Even if my readers know all the well-recognized facts about anatomy, I should still have to write a chapter on the subject to accentuate the proportionate values of certain points which appeal to me. Moreover, there are a few undescribed facts which I need to present. Obviously compromise is necessary for I can neither assume that my readers know their anatomy nor wish me to repeat every detail which they may turn to in their text books. Nevertheless, to do justice to me they should refresh their memories, and for this purpose a list is presented of all the terms which concern the shoulder used by Gray in my own worn edition. By running his eye over this list the reader may detect the weak spots in his own memory and, if he pleases, can turn to his Gray and revivify them. I beseech him to do so. Moreover, since this book is written quite as much for the coming generation as for my own and the present one, this list is presented in three columns so that it may serve as a glossary to all three generations. It appears that the professors of anatomy intend that future medical students in all countries shall be taught the international Basle Anatomic Nomenclature.
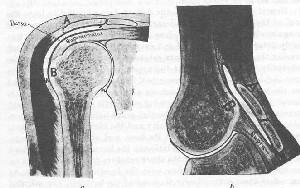
The writer believes that numbers 2, 3, and 4 of the above list are essentially one bursa, although they are often separated by thin, movable films of tissue.
He believes numbers 5 and 6 to be really extensions of the joint as is also the synovial lining of the bicipital canal, number 18 in Fig. 18, p. 29. The bursas numbered 9, 10, 11, 12, in the same diagram, are inconstant and have no official anatomic names.
Even if you have satisfied your mind that each term in the B. N. A. list carries its appropriate picture, let me give you my personal way of thinking of some of the parts of the human shoulder.
The shoulder. In descriptive anatomy there are no more sharp lines of distinction separating the regions called the shoulder, the neck, the back, the chest, the upper arm and the armpit, than we indicate in our ordinary uses of these words. Even the bones which compose its skeletal support cannot be sharply defined. Does the upper end of the humerus belong to the shoulder? Anatomists are accustomed to say no, and describe it with the arm. Surgeons certainly think of the upper end as a part of the shoulder, but would have no distinct lower limit. We shall include the upper end of the humerus above the deltoid tubercle, and leave the other limits still somewhat vague.
The shoulder girdle is not a complete girdle because the clavicles are separated by the manubrium (top of the sternum) in front, and the scapulae do not quite meet behind. In birds the clavicles do meet and form the wish bone, In fact, "girdle" means the two bones of one side only, so it takes two shoulder girdles to not quite girdle the body. It means for man the two bones which form a saddle for the arm to ride on the body, i.e., the scapula and the clavicle, but in birds and some other creatures it includes the coracoid as a separate bone, which is more massive than the scapula.
Did time and space permit, it would be instructive to discuss the comparative anatomy of the shoulder in the lower animals, for in different species there is great variation in the relative sizes and shapes of the muscles and bones and even in the proportions of the three component parts of the scapula itself. Most animals have only a trace of the acromion process which in man and in the monkey is extremely well developed, probably to stabilize the joint for its many newly developed uses.
So far as I know, no one has yet attempted to study the reasons which have led to the development of the variations of the different parts of the human scapula. Possibly I was the first to draw attention to a fundamental difference between the human and the quadruped mechanism in the use of the forelimb; i.e., the quadruped uses his supraspinatus to accelerate a pendulum, while in man, in raising the arm, this muscle acts at a disadvantage against gravity and under great strain.
I hope to convince the reader in later chapters, that rupture of this muscle in man is almost equivalent to dividing the hamstring in an animal. If man walked on his forelegs, patients with this lesion would limp pitiably and get much more sympathy than they do now when they can only allege that they cannot raise their arms. At any rate, from a mechanical point of view, man's ambitious change to the upright position resulted in a new form of shoulder joint. He has a relatively large and powerful acromion process to act as the mast of a derrick, to which his enormously developed deltoid is attached, and under which a relatively small supraspinatus is chiefly useful in holding the boom (humerus) on the fulcrum (the glenoid). We are proud that our brains are more developed than those of animals; we might also boast of our clavicles. It seems to me that the clavicle is one of man's greatest skeletal inheritances, for he depends to a greater extent than most animals except the apes and monkeys, on the uses of his hands and arms. The clavicle holds the shoulder away from the body and therefore permits us to use our arms with power and skill in abduction and adduction to a degree which few animals except the monkeys can approach. The gorilla's shoulder girdle is as well if not better developed than man's. Some of the lower monkeys have less developed ones resembling those of the quadrupeds, but all have clavicles.

Mammals that specialize in swimming (e.g., seals and whales) or in running (dogs, foxes, wolves) or in grazing (horses, cows, deer, pigs and other hoofed animals) have no clavicles. Even the carnivorous cat tribe (lions, tigers, leopards and the domestic cat) have only rudimentary or very small collar bones. In the bats, the clavicles are long and curved like those of birds. Moles have short, almost cuboid bones which are homologous with the clavicle, combined with the coracoid. Those species which do have clavicles appear to be flyers or climbers. Some of the rodents which climb trees—for instance, squirrels, have them. Other rodents have none whatever. Interestingly enough, some of the more ancient but waning species, such as the duckbill platypus, kangaroo, opossum and armadillo, have well-developed clavicles. Furthermore, the armadillo has the longest known acromion process and very few other animals have any to speak of. It appears that the acromion is developed in this animal to aid in carrying his shell.
The beaver has the most highly developed clavicle of any four-footed animal that I know of. His skeleton is also notable because he has a well-developed acromion process and a large deltoid tuberosity. His shoulder girdle is the best instance I can find for my theory that animals with strong clavicles use their arms in adduction and abduction, for the beaver's mechanical skill in building his huts and constructing his dams is well known. Bears are my worst examples, for bears are clever in climbing, and yet have no clavicles.
The sterno-clavicular joint
Any one can easily feel the joint where his clavicle touches the top of his sternum and realize that this is the only point at which the weight or power of his shoulder can get direct support from the rest of his skeleton when he pushes with his arm. And yet after removal of the clavicle, a man has pretty good use of his shoulder just as do horses and dogs who have no clavicles.
The acromio-clavicular joint
One can feel this at the other end of the clavicle and realize that this, too, must through its small surface transmit power or weight. One can also feel that the clavicular side is higher than the acromial side of the joint. It is an important fact. When one looks at the clavicle from above, one sees no joint surface, but when one looks at it from below one sees a joint surface at each end. This provides for upward displacement at either extremity, and therefore we never find downward dislocation of either end of the clavicle.
The coracoid process
The coracoid process is in shape and size much like a crooked forefinger projecting forward from the neck oi the scapula just as the acromion process projects back of the joint. The outer end of the clavicle crosses it transversely and is very firmly united to it by the coraco-clavicular ligaments which one cannot palpate because they are wholly underneath it. One can just feel the end of this process below the outer end of the clavicle. It seems to be a part of the head of the humerus, but by rotating the latter, one may note motion between the two.
The acromion process
This forms the whole of the posterior part of the top of the shoulder, while the head of the humerus makes the rounded forward outline. The acromion extends well behind the articular head and the plane of its broad end is obliquely downward and backward and outward. Notice on your own shoulder how you can put your finger under the back of it. Notice that you cannot, with a club, hit a man from above or from behind on the top of his humerus, for the acromion is always in the way. If the arm is raised, flexed forward or abducted; i.e., when he is raising his arms to fight or crawling away on hands and knees, the whole humeral head is protected by the acromion and you could not hit the top of it from any direction. If his elbow is drawn backward, you could, from in front, strike on the front of the top of the tuberosities but not on the articular cartilage. This is a very important anatomic point for the surgeon, for only when the arm is in dorsal flexion can one feel the gap where a supraspinatus tendon has been ruptured. It also leads to the conclusion that histories are unreliable which claim an injury to the top of a humerus from a fall or a blow. One cannot fall on the top of one's humerus, or strike any one else on the top of his humerus.
The spine of the scapula
The spine of the scapula is the long base of the acromion and there are two little bony lumps on its lower edge which one can always feel and which are very useful as measuring points. The dorsal surfaces of the acromion and of the spine of the scapula are subcutaneous ; i.e., there are no muscles between them and the skin. Evidently the ridge which they form was made to be hit; i.e., to protect the shoulder joint and the brachial plexus from blows from above and behind. Consider the mechanics of its structure and notice how, with the clavicle, it forms a movable arch over the vessels and nerves of the arm. This arch flaps like a wing as you hunch your shoulder and lower it, or abduct your arm and lower it. Observe also that the spine of the scapula rises between the supra- and infraspinatus to give attachment to the superficial layer of great muscles, i.e., the trapezius and the deltoid. The two sets of muscles would be separated by sawing through the spine of the scapula.
The glenoid
The glenoid is the shallow cartilage-covered surface where the head of the humerus obtains its fulcrum as the arm is raised. Notice that the plane of its surface is at no particular angle with the rest of the scapula, for it faces somewhat forward and upward, and outward. Notice its narrow superior portion.
The blade
The upper portion of the blade of the scapula from the lateral view forms in most people an obtuse angle with the rest of the blade so that it can fit over the curve of the upper ribs at the base of the neck. Thus the thin blade of the scapula when pressed forward from behind fits nicely over the back of the upper seven ribs. Furthermore, the bony structure of the scapula is beautifully arranged to distribute force applied from behind.

The clavicle
The clavicle is a strut which connects the rest of the shoulder with the skeleton. It prevents the upper portion of the shoulder from jamming up against the rest of the body. In other words, the clavicle acts as does the iron rod a man uses to hold a bull who has a ring in the end of his nose. The clavicle is capable of a limited degree of circumduction, which is facilitated by the double joint at the sternal end. Circumduct your whole arm with the forefinger of the opposite hand on the outer tip of the clavicle and you will find that the latter passes through an irregular circle about three inches in diameter. The clavicle is the boom of a derrick (the neck) and enables the trapezius to raise the whole shoulder.
The ligaments
It is well to distinguish four kinds of ligaments which occur about the shoulder. (1) Those that pass between two different bones about a joint, such as the capsular ligaments of the sterno-clavicular, the acromio-clavicular and the scapulo-humeral joints, or strengthening bands in these capsules such as the superior acromio-clavicular ligament or coraco-humeral and gleno-humeral ligaments which are merely slightly firmer portions of the capsular ligaments. (2) Those that bind two bones together without a joint but permit a very limited amount of motion. The coraco-clavicular ligament composed of conoid and trapezoid portions is a very typical example. (3) The interarticular fibro-cartilages are usually classed as ligaments. There are three of these related to the shoulder; a very typical one in the sterno-clavicular joint; a less typical, often rudimentary one in the acromio-clavicular joint; and the glenoidal labrum which encircles the glenoid cavity and makes it slightly deeper. (4) Those that pass between two processes of one bone in a static manner, apparently with a purpose of restraining the mobility of other structures. In the shoulder there is such a ligament crossing the suprascapular notch through which the nerve and vessel pass. The transverse humeral ligament which makes the bicipital groove into a canal to restrain the long tendon of the biceps, is another. The coraco-acromial ligament is one of this kind, and we must speak of it in more detail.
[[File:Sensitive-content.pnge many degrees in all directions by the aid of the subacromial bursa. The reader must understand that the dissection pictured above is quite artificial. Such a capsule does not exist unless made at the expense of the musculotendinous cuff.]]
The coraco-acromial ligament
The coraco-acromial ligament will be mentioned again and again in this volume. It is wholly a scapular ligament, passing between the two processes from which it takes its name which are parts of one bone. Its under surface forms most of the posterior part of the roof of the subacromial bursa, and the tuberosities of the humerus pass upward underneath it when the arm is elevated. It lies between the bursa and the acromio-clavicular joint. Its function appears to be largely to restrain the head of the humerus from gaining a fulcrum on this joint or on the under side of the end of the clavicle. It is more elastic than bone but quite firm. Evidently the coraco-acromial ligament has an important duty and should not be thoughtlessly divided at any operation. One always finds it if the bursal incision is carried upward. The bursa, with this ligament and the two bones to which it is attached, really forms a secondary shoulder joint.
The other ligaments with simple but confusing names—the acromio-clavicular and the sterno-clavicular—surround their respective joints and pass between two different bones and have the functions usual in other joints. We have already spoken of the coraco-clavicular ligaments (p. 9) which are not connected with any joint and are the mainstay in binding the shoulder blade by the coracoid process to the collar bone. The coraco-humeral and gleno-humeral ligaments should never have been described as entities. They are merely somewhat variable parts of the joint capsule.
The muscles
I have few particular comments to make about the muscles which seem to be easier to remember from our student days. I would like to call attention to the compact entity formed by the short rotators when the deltoid and trapezius have been removed. When one thinks of the shape of each of these individual muscles, one must remember that the joint is mobile and that the position of the humeral head on the glenoid greatly alters the shape of each muscle attached to its tuberosities.
Taking the group as a unit they form an entity which remains of about the same shape whether the arm is rotated in or out, but each of these muscles becomes hooked around in the direction toward which the humeral head happens to be rotated. Not only is this true, but their shapes are much altered by whether the humerus is pointing downward or upward. I should like to make a plea for teaching the student that in thinking of the shapes of muscles, he should be able to visualize their positions in the extremes of motion of the adjacent joint. The subclavius muscle is seldom alluded to in practical surgery. Its function seems to be to draw the clavicle down toward the ribs when the former has been raised by the trapezius, either in hunching the shoulder or in abducting the arm. Possibly it has some importance when division of the nerve supply causes contracture, just as the clavicular portion of the pectoral may limit the motion of the arm by contracture when its nerve supply has been destroyed by careless dissection of the axilla. The subclavius is mentioned chiefly because no one has yet reported any clinical condition in which it is an important factor. Here is a chance for original work.
The head of the humerus is very much larger than the glenoid cavity of the scapula on which it rests and on which it has to gain its fulcrum whatever the position of the arm when in use. There is no fulcrum in the standing position with the arm at rest at the side, or in any other position in which the arm is at rest without any of the muscles in use. In such positions of rest, the head of the humerus is held in contact with the glenoid surface by atmospheric pressure. The capsule of the joint is quite unlike the capsule of other joints, for it must admit of motion in any direction, and hence it cannot have any of its parts in a state of tension when it is in a mid-position; therefore, the capsule is approximately twice as big as the size of the anatomic head of the bone, and any part of its circumference will only be tense when the extreme of motion is reached in the opposite direction.

The short rotators
Another peculiarity of the joint is the fact that the tendons of the short rotators, viz., the supraspinatus, the infraspinatus, teres minor and subscapularis, are closely incorporated with the capsule through almost their whole extent. The tendons are broad and flat and only about an inch in length. This matter is spoken of more at length on page 74. It is impossible either to dissect these tendons from the capsule on the one hand, or from the synovial base of the subacromial bursa on the other. Within a half inch of the sulcus which surrounds the cartilaginous head of the bone, even a microscopic section in this region shows no distinction between the tendon substance and the joint capsule. Anatomists have concluded that this arrangement of the tendons prevents the redundant portions of the capsule from getting caught between the articular surfaces as the joint moves. Figure shows a section through the supraspinatus tendon at the sulcus and illustrates the manner in which the tendon is inserted into the bone.
The student who is taught his anatomy from the dried bones, may get a false impression from having the facets of insertion of the short rotators pointed out to him as specifically the places where these muscles are attached to the bone. As a matter of fact the attachment takes place throughout most of the upper half of the sulcus, which is called the anatomic neck, and which separates the cartilaginous edge from the tuberosities. Doubtless the heavier portions of these tendons are inserted in the smooth facets which anatomists point out on the tuberosities. However, if one excises the head of the humerus with these short rotators attached to it, one finds that the insertions of all four muscles are so intimately incorporated with the capsule, and with each other, that one cannot, even with careful dissection, separate any one tendon from the neighboring tendon. This fused structure will be alluded to as the musculo-tendinous cuff.
The musculo-tendinous cuff
This musculo-tendinous cuff does not extend completely around the head of the bone. It occupies approximately the upper half of the circular depression, called the anatomic neck. There are no tendons inserted on the lower axillary side, and in this' region the capsule is reflected farther away from the rim of the cartilage than it is in the portion where the tendons are inserted. There is no very definite mark on the bone on this axillary side to show where the capsule was attached.

The sulcus and anatomic neck
Looking from the inside of the joint of a fresh cadaver there is no sulcus in the upper portion opposite the attachments of the supra-spinatus and infraspinatus, or opposite most of the adjacent parts of the subscapularis and teres minor. About opposite the middle of the insertion of the teres minor on the one side, and the middle of that of the subscapularis on the other side, the line between the cartilage edge and the insertion of the cuff begins to get broader; i.e., the lower portions of the insertions of the subscapularis and of the teres minor are slightly farther from the articular rim than are the insertions of the other muscles. On both sides, as we pass downward, the line gets broader until at its broadest point, it is nearly a half inch wide on the axillary side of the capsule. The reader must understand that all this refers to the sulcus before the tendons are removed and while the membrane is still intact. After maceration, the bare bone sulcus (the anatomic neck) is quite the reverse, and is broad where it was formerly narrow. When looking at the bare bone, one sees a deep sulcus (the anatomic neck) between the tuberosities and the rim of the articular surface and one must realize that in life this sulcus is filled by the musculo-tendinous cuff. In the bare bone one sees that there are many vascular foramina in this part of the sulcus. The reader should see for himself the points described in this paragraph, because many shoulder symptoms may be accounted for by the evulsion of fibers of insertion at the articular margin of this sulcus. In cases of complete rupture of the tendons the bony sulcus is palpable even through the thick deltoid. I believe that when at autopsy one finds any sulcus present between the cartilage and the attachment of the supraspinatus, or a broadening of the sulcus opposite the attachments of the other muscles so as to expose bare bone, we have proof that a pathologic condition has existed. I have never seen any mention of one of these rim rents in any book on anatomy, pathology or surgery, yet on examination of these joints at autopsy it is a very common finding. In fact, in aged people it is hard to obtain a perfectly normal shoulder joint, just as it is to find a perfectly normal aorta.
Bursa about the shoulder
It is very difficult to find any accurate description of the subacromial or subdeltoid bursa, and I feel that even if I could give a clear description I could not in any words convey as much as I could by one demonstration. At the time I first wrote about this bursa its importance was not recognized, and even its anatomic outlines were very poorly described. The main reason for the inaccuracy of our knowledge was that no one had studied it from inside. In dissecting, anatomists removed the deltoid muscle and then described the bursa, the upper portion of which, together with some of the periphery, was necessarily removed with the deltoid. All that was left of the bursa was an inconspicuous portion about the size of a half dollar which remained attached to the greater tuberosity. The portion of the roof, which was attached to the under side of the acromion, would not be noticed. Furthermore, in the average dissecting room specimen, the tissues are badly discolored and the limits of the synovial membrane, which is very thin indeed, are not clearly marked.
The functions and structure of bursa in general should be considered before going any further. Nature provides bursas in many parts of the body where a considerable degree of motion between parts of the anatomy is necessary, and yet no cartilaginous joint is required. Especially is this true where two muscles cross each other in opposite directions, or where a muscle or a tendon and a bone move past each other without actual articular contact. Some of the best known bursas occur between some portion of the skeleton and the skin over it. The skin is more or less movable over most parts of the body, and the mobility is permitted by the fatty or areolar tissue which lies between it and the deep fascia, but occasionally, as over the patella and over the elbow, the skin must move to a considerable extent, so that spaces are formed in the areolar tissue which allow it to glide over the bony prominences. The prepatellar bursa, for instance, has a base firmly fixed to the upper surface of the patella and a roof firmly fixed to the under surface of the skin. The same is true of the olecranon bursa at the elbow. It is the mobility of the periphery which permits motion rather than the attached parts of the roof and base. In other parts of the body bursas lie between bony prominences and fascia or between tendons and muscles, but the principle of attached portions and movable peripheries holds good in all. In the shoulder we have examples of the several kinds; e.g., there is a small subcutaneous bursa over the acromion, and a triangular bursa between the tendinous fibers of the trapezius and the dorsum of the scapula at the base of its spine.
File:Sensitive-content.pngable.
The surfaces have been depicted as if separated, but of course in the normal living tissue these surfaces are in contact and their motion is linear as suggested in Fig. 13. One must realize that the thin, movable periphery sometimes has to fold on itself as base and roof move about. The nictitating folds seen on the inside of a bursa are double layers of the periphery, so very thin that they readily roll on one another as do the membranes which come across a bird's eyes.
In the subacromial bursa the section of the space in most positions is a curved line which represents a section through the segment of an almost perfect hemisphere.
It seems to me that it is very doubtful whether it is best to apply the term bursa to extensions of the joint cavities, such as that beneath the tendon of the quadriceps at the knee. This synovial space is chiefly useful to enable the tendon of the quadriceps to ride over the anterior portions of the condyles of the femur. In a fully flexed knee, practically the whole of this surface has passed downward over the cartilage. It is simpler to regard this so-called quadriceps bursa as part of the synovial lining of the joint, where it does not need a true capsule, because of being reinforced by muscle. In the shoulder joint there are two so-called bursae which the anatomists describe (Bursa M. subscapularis and B. M. infraspinati), which to my mind are simply extensions of the joint for the same purpose as that of the quadriceps bursa at the knee. It requires little imagination to see that when the humerus is rotated inward, the infraspinatus bursa would be largely straightened out with the stretched infraspinatus muscle, and vice versa, the subscapularis bursa would likewise become a part of the capsule of the joint in extreme external rotation.
On examining many joints from inside the capsule, one does find occasionally that the openings from these bursse, or extensions of the joint, may be considerably smaller than the width of the extensions a little further back than the edge of the glenoid. This gives them the appearance of diverticuli. There is a great variation in the size of these openings.
Gray, after describing these two bursal sacs related to the shoulder joint, says, "A third bursal sac, which does not communicate with the joint, is placed between the under surface of the deltoid and the outer surface of the capsule." This description of the subdeltoid or subacromial bursa, which is the only one he gives, is good so far as it goes, but Gray could not have appreciated its extent or its surgical importance or he would have written much more about it. Part of it is placed "between the under surface of the deltoid and the outer surface of the capsule," but that is far from describing its full extent, as will be seen later.
Piersol goes into the description of the bursa in slightly more detail, but it evidently did not greatly interest him and he was not very accurate in regard to it. For instance, he says, "The large subacromial bursa and the subdeltoid bursa have been described as to their possible enlargement;" i.e., he considers that there are two bursae, whereas there is really only one. The fact that he says "as to their enlargement" shows that he did not appreciate that they constituted essentially a secondary joint which needed pages of description on account of its clinical importance. He also says, "Bursas are sacs filled with fluid found in various places where friction occurs between different layers or structures." To describe them as "sacs filled with fluid," gives a wrong impression. They are really spaceless spaces, not filled with fluid, but supplied with a most wonderful self-oiling mechanism, so that their walls glide on one another with their surfaces no farther apart than the thickness of the thinnest sheet of paper. In consequence of this spaceless structure, any method of demonstrating bursae by filling them with opaque materials, as wax, or even with air, causes distention of their cavities and contraction of the periphery. In other words, the circumference of a bursa, when not distended, is very much larger than when it is blown up in the form of a sphere. Piersol states, "The subdeltoid bursa does not usually communicate with the joint," leaving one to think that it occasionally does communicate. As a matter of fact, when I began my work on the bursa, Dr. Thomas Dwight, who was then Professor of Anatomy at Harvard, disputed my finding ruptures of the supraspinatus which permitted the joint fluid to flow into the bursa. He explained these communications as semi-normal openings between the joint and bursa, similar in structure to the communications of the bursas under the infraspinatus and subscapularis. So positive was he on this point, that it took me a long time to convince him that the instances of communication which we found in his dissecting room were pathologic. So frequent are these ruptures in the ordinary anatomic material, that it is quite natural that the anatomists have thought they were merely instances of persistent congenital anomalies and should have ignored them as the results of a common form of trauma.
The subacromial bursa itself is the largest in the body and the most complicated in structure and in its component parts. It is in fact a secondary scapulo-humeral joint, although no part of its surface is cartilage. Instead of being between bone and skin, it is between bone and tendon, muscle and bone. It is firmly attached on its base to the upper and outer three-fourths inch of the greater tuberosity, as well as to about a three-fourths inch of the tendons of the four short rotators where they are attached to the tuberosities. Part of its base covers the bicipital groove. Its roof is firmly attached to the under side of the acromion and to the under side of the coraco-acromial ligament, and to the fibers of origin of the deltoid from the edge of the acromion. Its periphery extends loosely downward under the deltoid, backward and outward under the acromion, and inward under the coracoid, between it and the subscapularis, and under the common origin of the short head of the biceps and the coraco-brachialis. The roof and base are in intimate contact and it is lined by synovial membrane, which is almost as thin as a cobweb. Nevertheless this layer has the property of secreting just enough synovial fluid to render the movement between the two surfaces practically frictionless. Beneath this membrane is always a network of fine blood vessels, so that the secretion can be increased or diminished on demand. This arrangement also permits it to become congested in a short time, just as the peritoneum may. The subacromial bursa is an absolutely necessary part of the shoulder joint. When its surfaces are inflamed so that they cause painful friction, the arm cannot be rotated or abducted. Their complete adhesion has the same effect.
Let us return now to the incision to demonstrate the bursa. One who intends to read this book would save himself much trouble if he could perform on a cadaver the following experiment. Make an incision two inches long from the acromio-clavicular joint downward between the deltoid fibers. The fascia under the deltoid is thin and beneath it will be the roof of the bursa. Pick this up between forceps and incise it as if it were the peritoneum. Enlarge the opening upward until it meets the fibers of the coraco-acromial ligament. Enlarge the incision downward until you arrive at the lower edge of the incised synovial membrane; then pass a probe into the bursa and determine its limits in all directions. You will find that it goes upward beneath the acromion more than three-quarters of an inch; it also extends outward and inward for about the same distance, and you have already opened it an equal extent downward. It is therefore a concavo-convex circular cleft about 1% inches in diameter. Its base is a hemisphere which fits inside its roof, which is the inside of another hemisphere. Its periphery is movable to almost as great an extent as shown in Fig. 16. With the forearm flexed at a right angle, rotate the humerus inward and outward, and the base of the bursa will pass in review across the bottom of your incision. With the arm in extreme internal rotation, mark the most external point on the base which you can see through the incision, then put the arm in extreme external rotation and mark the point on the base which is nearest the inside of the incision. Mark with a knife down to the bone the upper and lower points of the base when the arm is carried into extreme dorsal flexion and extreme frontal flexion. Later on, removing the deltoid, you will be surprised to find that these marks are on the periphery of a circle nearly two and one-half inches in diameter. Next, with retractors in the wound, pull the arm downward so as to allow air to enter the subacromial portion of the bursa. You will find a cavity large enough to put your forefinger in, and you can sweep the finger around to the inner side so that with the arm in internal rotation your finger will pass between the tendon of the subscapularis and the tip of the coracoid process. When you retract the inner edge of the incision and the arm is in internal rotation, you can pass the handle of the knife into the subcoracoid portion of the bursa, which some anatomists have described as a separate bursa, but which in reality is not, although sometimes there is a film of synovial membrane crossing the bursa so as to partially separate this portion from the remainder of the bursa.
If you will repeat this experiment on cadaver after cadaver, you will become convinced that the subacromial bursa, the subdeltoid bursa and the subcoracoid bursa are one and the same thing, although films of tissue may separate them.
When the arm is elevated, even the subdeltoid portion becomes subacromial. When the arm is rotated inward some of the subdeltoid portion becomes subcoracoid.
Now if you please, remove the deltoid, being careful to leave the roof of the bursa which is underneath it. When you have examined it again without the deltoid, clear away the portion which was formerly attached to the deltoid and examine the base to see how much overlies the tendons of the short rotators, and how much overlies the tuberosity. You will find that the upper half of the hemisphere lies over the tendons while the lower half lies over the tuberosity, and yet the whole base presents such an even convex surface that it is almost a perfect hemisphere, showing very little sign of the different structures underneath it. By careful palpation, however, you can determine the edge of the tuberosity and the bicipital sulcus. Next, remove the acromion process at its base, and observe the arrangement of the short rotators in relation to the bursa. This is best done by cutting off the muscles of the short rotators from their origins on the scapula, and reflecting them over the head of the humerus. As you reflect them outward over the head of the humerus, you will find that the dissection readily reveals the glenoid portion of the capsule, but when you come within an inch of the insertion of the tendons into the tuberosities you can only separate the tendons from the capsule by sharp division. Leave the short rotators thus inverted over the head of the bone as a boy pulls his sweater halfway over his head, and remove the glenoid attachment of the capsule. Inside the capsule you will find the long head of the biceps free except for its attachment to the upper edge of the glenoid. Now look inside the capsule from the glenoid end and observe the condition of the sulcus. Note the canal where the biceps tendon follows into the groove through the intertubercular notch. Slit open the groove and follow the tendon down to see where the synovial membrane is reflected. Observe that in doing this you cut across the tendon of the pectoralis major and you pass between the attachments of the pectoralis major on the outer side and those of the teres major and latissimus dorsi on the ridge which forms the inner lip of the groove. Do not forget to examine from the inside of the joint the extensions under the infraspinatus and subscapulars which have been called bursae.
The subcoracoid portion of the bursa (Bursa M. coraco-brachialis) has been described by some anatomists as a separate bursa.[15] has attempted to account for certain clinical symptoms as arising from inflammation in this bursa. I regret that I cannot subscribe to Goldthwait's anatomic description, nor to his interpretation of the clinical symptoms caused by it. I have great admiration for the work which he has done in regard to the conditions in the lumbosacral and sacroiliac regions. He has been a great pathfinder in the treatment of these conditions, but I feel that his articles on the shoulder are less accurate and sometimes misleading. I think that most of the cases which Goldthwait attributes to subcoracoid bursitis are essentially subacromial, for the subcoracoid bursa is only a part of the subacromial bursa. I have already explained that the subacromial bursa in the anatomic position becomes largely subdeltoid, and vice versa, in abduction, becomes largely subacromial. When the arm is behind the back the subdeltoid bursa becomes largely subcoracoid as the humerus is rotated internally. In external rotation the subcoracoid portion is nearly effaced as the movable periphery is stretched outward from beneath the coracoid process. Even in cases in which there may be a synovial fold between the subcoracoid and subdeltoid portions of the bursa, the two portions are essentially one. I have found this partition complete, although not infrequently I find a nictitating fold of the finest synovial membrane which forms only a partial partition between the two. These nictitating folds are always found in the subacromial bursa, not only in this situation, but in other parts. They are really parts of the movable periphery. They fold on themselves when not stretched by some extreme motion, and because they are almost as thin as cobwebs, the double layer has little thickness and is quite transparent. Even when double, they are thinner than the normal peritoneum. After trauma or operation in this region, these film-like partitions in various parts of the bursa may become adherent and cause it to be split up into a number of small sacs. Even when the subdeltoid portion of the bursa has been removed, a new subdivided sac takes its place.
The reader should thoroughly understand that there is a difference between the subcoracoid portion of the subacromial bursa (Bursa M. coracobrachial) and the bursa connecting with the joint which lies under the subscapularis, between it and the edge of the glenoid (Bursa M. subscapularis). This extension of the joint has nothing to do with the subcoracoid bursa about which we are speaking, which lies anterior to the subscapularis. The subcoracoid bursa or, as I prefer to say, the subcoracoid portion of the subacromial bursa, lies between the subscapularis muscle, the coracoid process and the combined origins of the tendons of the short head of the biceps and coracobrachialis, which arise from the coracoid process. It is therefore separated by the whole thickness of the subscapularis muscle from the extension of the joint beneath it. However, bursas, even more than muscles or tendons, vary in form in different individuals. For instance, since both bursas approach each other on the superior surface of the subscapularis, we sometimes find them united over it, so that a horseshoe shaped arch is formed beneath the coracoid process and the tendons arising from it. Under this arch the subscapularis may run with much freedom. I think such communications are not uncommon, particularly where the bursas have become dilated from the presence of fluid.
Since the movement of the subscapularis muscle is at right angles with the tendons of the coracobrachialis, etc., it is quite necessary for nature to supply a bursa in this region. The arc of motion of any point on the lesser tuberosity is somewhere about an inch and a half between the position of internal rotation and the position of external rotation, and this would be a long stretch for simple areolar tissue. When I first wrote about these bursas, I did not fully realize that the subcoracoid and subacromial bursa usually communicated, and the old figures were inaccurate for that reason (Figure 33).
Other bursas about the shoulder have been claimed. Piersol says:"An infraserratus bursa has been described (Terrilon) situated between the inferior scapula angle and the chest wall. Its enlargement gives rise to friction-like crepitation or creaking, which has been mistaken for fracture of ribs or scapula, or for an arthritis of the shoulder." He also quotes Nancrede as discussing these symptoms. Goldthwait has also written on a subscapular bursa which he claims may give similar symptoms. This bursa is said to be between the upper and anterior portion of the blade and the back of the first three ribs. It also would necessarily be "infraserratus."
We must agree that in some people, there are peculiar cracklings when the shoulder blades are moved, and that pain sometimes occurs with the cracklings. Goldthwait is inclined to attribute these peculiar cases, in which there is a painful crepitation or creaking, to this subscapular bursa, and it is quite possible that Terrilon and Nancrede and others have attributed the same symptoms to the above-mentioned infraserratus bursa at the lower angle. I have sometimes thought that such noises were due to unusual friction in the small inconstant subtrapezoid bursa which lies over the triangular surface at the base of the spine of the scapula under the trapezius. This particular bursa is very apt to become sore in cases where there are scapulo-humeral adhesions and the shoulder blade is obliged to do double work. I am apt to attribute such symptoms to this subtrape-zoid bursa and am not prepared to take a positive stand as to the existence of either the infraserratus bursa at the lower angle of the scapula, nor of the subscapular bursa at the upper angle of the scapula. I recognize cases which have painful crepitation in these regions, but practically I do not see cases with severe enough symptoms to make me feel like operating on these patients. Goldthwait's article is worth reading, and he has undoubtedly cured patients with these symptoms by removing the upper portion of the scapula. It seems to me that this is a rather radical operation for a doubtful condition, but the operation is not dangerous and the symptoms sometimes very severe. One should consider the question carefully. The shoulder is prone to reverberate crackling noises which often times are perfectly painless. I can move my own scapula so as to make it sound about the room without the slightest pain, and yet I cannot even locate the exact spot where the primary vibration takes place. Creaking shoulders are as common as creaking knees and are usually painless. One must be on one's guard not to attribute symptoms to conditions which cause creaking noises, for the symptoms may be due to something which accompanies rather than causes the creaking.
Small bursas arc described beneath some of the tendons near their attachments to the humerus on the ridges on each side of the bicipital groove. These bursas probably exist to permit the bone to turn away from the dense tendons when the latter exert their power to rotate the bone on its long axis. The teres major, latissimus dorsi and pectoralis major are said to have such bursae. I have never seen lesions in any of them, although sometimes I have found local tenderness over their locations in living patients. Such cases have usually promptly recovered; I have never known of any chronic condition in one of these bursas.
I have also seen a case where there was a very distinct bursa superior to the coracoid process, between it and an anomalous insertion of the pectoralis minor to the outer side of the process. This anomaly, if found to be a frequent condition, might explain a few cases which are now clinically obscure. The synovial lining of the bicipital canal has sometimes been described as a bursa. To my mind it is more properly called a sheath, but it is in fact merely an extension of the joint cavity with which it freely communicates.
An anatomic point which is readily forgotten in thinking of the shoulder is that the upward motion called hunching is performed by the upper part of the trapezius muscle, and this muscle is supplied by the spinal accessory. Not long ago, a patient was sent to me for shoulder symptoms which had not been attributed to a recent operation on the neck!
An interesting, if not important point, is that the platysma extends down into the skin over the shoulder, and Gray says that it actually has an attachment to the edge of the acromion. In cases where the trapezius has been paralyzed for a long time, one may see the shoulder feebly lifted by the platysma. It does not seem to me necessary in this book to review the situations of the arteries and veins. Surgeons have come to think lightly of arteries because it is so easy to tie them and find no apparent immediate sign of harm following the ligation. As a rule one can safely rely on the anastomoses to supply the region with sufficient blood. Personally I try to save arteries and even large veins when I can. In plastic operations about the shoulder joint, it is doubly necessary, for if one ties too freely, one may tie not only the main artery of the part, but its collaterals, and healing may be delayed. The nerves which supply the muscles about the shoulder will be taken up with the discussion of the various forms of paralysis, but the reader should at least know well the upper portion of the brachial plexus.
There are three free bony surfaces in the shoulder which one should bear in mind, for they are of practical importance beyond the slight attention called to them in anatomic text books. One of these is on the back of the upper end of the humerus, in the region of the surgical neck, internal to the origin of the external head of the triceps. This bare portion of course is not, strictly speaking, bare, for it is covered with periosteum and areolar tissue, but it has no muscular origin or insertion on it, and is opposite the glenoid head of the triceps. The other two similar surfaces are on the inner and outer side of the neck of the glenoid on the body of the scapula. The anterior is beneath the subscapulars and the posterior beneath the infraspinatus. These surfaces should be borne in mind when one is visualizing fractures or dislocations of this neighborhood. The extensions of the joints (B. M. subscapularis and M. infraspinati) under these muscles lie in the spaces over these smooth areas.
References
- ↑ You T, Frostick S, Zhang WT, Yin Q. Os Acromiale: Reviews and Current Perspectives. Orthop Surg. 2019;11(5):738-744
- ↑ Buss DD, Freehill MQ, Marra G. Typical and atypical shoulder impingement syndrome: diagnosis, treatment, and pitfalls. Instr Course Lect, 2009, 58: 447– 457
- ↑ Maffulli N, Longo UG, Berton A, Loppini M, Denaro V. Biological factors in the pathogenesis of rotator cuff tears. Sports Med Arthrosc Rev, 2011, 19: 194– 201
- ↑ Yammine K. The prevalence of os acromiale: a systematic review and meta-analysis. Clin Anat, 2014, 27: 610– 621
- ↑ Harris JD, Griesser MJ, Jones GL. Systematic review of the surgical treatment for symptomatic os acromiale. Int J Shoulder Surg, 2011, 5: 9– 16
- ↑ Sahajpal D, Strauss EJ, Ishak C, Keyes JM, Joseph G, Jazrawi LM. Surgical management of os acromiale: a case report and review of the literature. Bull NYU Hosp Jt Dis, 2007, 65: 312– 316
- ↑ Atoun E, Van Tongel A, Narvani A, Rath E, Sforza G, Levy O. Arthroscopically assisted internal fixation of the symptomatic unstable os acromiale with absorbable screws. J Shoulder Elbow Surg, 2012, 21: 1740– 1745
- ↑ Edelson JG, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg Br, 1993, 75: 551– 555
- ↑ Prescher A. Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. Eur J Radiol, 2000, 35: 88– 10210
- ↑ Macalister A. Notes on acromion. J Anat Physiol, 1893, 27: 244.1– 244.251
- ↑ McClure JG, Raney RB. Anomalies of the scapula. Clin Orthop Relat Res, 1975, 110: 22– 31
- ↑ Johnston PS, Paxton ES, Gordon V, Kraeutler MJ, Abboud JA, Williams GR. Os acromiale: a review and an introduction of a new surgical technique for management. Orthop Clin North Am, 2013, 44: 635– 644
- ↑ 13.0 13.1 Boehm TD, Matzer M, Brazda D, Gohlke FE. Os acromiale associated with tear of the rotator cuff treated operatively. J Bone Joint Surg Br, 2003, 85: 545– 549
- ↑ Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic os acromiale. J Am Acad Orthop Surg, 2006, 14: 12– 19
- ↑ Goldthwait JE. An anatomic and mechanical study of the shoulder joint, explaining many of the cases of painful shoulder, many of the recurrent dislocations and many of the cases of brachial neuralgia or neuritis. Am J Ortho Surg. 1909;6:579-60
- ↑ Flower WM. An Introduction to the Osteology of the Mammalia, third edition, London Macmillan,1885
- ↑ Parker WK. A monograph on the structure and development of the shoulder-girdle and sternum in the Vertebrata. Ray Society. London, Hardwicke, 1868
- ↑ Jarjavay JF. Die Anatomie und Pathologie der Schleimbeutel und Sehnen-scheiden, Erlangen, 1863
- ↑ Gruber W. Die Oberschulterhakenschleimbeutel (Bursse mucosae, supra-coracoidese). Eine Monographic mit Vorbemerkungen enthaltend: Beitrage zur Anatomie der Regio infraclavicularis und deltoidea, 4th, St. Petersburg, 1861